| Author | Affiliation |
|---|---|
| Steven Pincus, MBBS, BSc | Emergency Department, Ballarat Health Services, Ballarat, Victoria, Australia |
| Merle Weber, MBBS | Emergency Department, Ballarat Health Services, Ballarat, Victoria, Australia |
| Alex Meakin, MBBS | Radiology Department, Ballarat Health Services, Ballarat, Victoria, Australia |
| Ross Breadmore, MBBS | Radiology Department, Ballarat Health Services, Ballarat, Victoria, Australia |
| David Mitchell, MBBS | Orthopaedic Unit, Ballarat Health Services, Ballarat, Victoria, Australia |
| Luke Spencer, MBBS | Orthopaedic Unit, Ballarat Health Services, Ballarat, Victoria, Australia |
| Nathan Anderson | Emergency Department, Ballarat Health Services, Ballarat, Victoria, Australia |
| Phil Catterson, BN, MBA | School of Medicine, University of Melbourne, Parkville, Victoria, Australia |
| Steve Farish, BSc, Med | School of Medicine, University of Melbourne, Parkville, Victoria, Australia |
| Jaycen Cruickshank, MBBS, MCR | Emergency Department, Ballarat Health Services, Ballarat, Victoria, Australia |
ABSTRACT
Introduction:
We developed and implemented clinical practice guideline (CPG) using computerized tomography (CT) as the initial imaging method in the emergency department management of scaphoid fractures. We hypothesized that this CPG would decrease unnecessary immobilization and lead to earlier return to work.
Methods:
This observational study evaluated implementation of our CPG, which incorporated early wrist CT in patients with “clinical scaphoid fracture”: a mechanism of injury consistent with scaphoid fracture, anatomical snuff box tenderness, and normal initial plain x-rays. Outcome measures were the final diagnosis as determined by orthopaedic review of the clinical and imaging data. Patient outcomes included time to return to work and patient satisfaction as determined by telephone interview at ten days.
Results:
Eighty patients completed the study protocol in a regional emergency department. In this patient population CT detected 28 fractures in 25 patients, including six scaphoid fractures, five triquetral fractures, four radius fractures, and 13 other related fractures. Fifty-three patients had normal CT. Eight of these patients had significant ongoing pain at follow up and had an MRI, with only two bone bruises identified. The patients with normal CTs avoided prolonged immobilization (mean time in plaster 2.7 days) and had no or minimal time off work (mean 1.6 days). Patient satisfaction was an average 4.2/5.
Conclusion:
This CPG resulted in rapid and accurate management of patients with suspected occult scaphoid injury, minimized unnecessary immobilization and was acceptable to patients.
INTRODUCTION
The traditional approach to diagnosis of scaphoid fracture is based upon a combination of historical clinical signs that are sensitive but not specific.1,2 When combined with dedicated scaphoid radiographs in acute wrist injury, this process fails to diagnose a scaphoid fracture in 7–36% of cases.3–10 Clinical scaphoid fracture is defined as patients with suspected fracture not seen on initial radiographs, a mechanism of injury consistent with scaphoid fracture, and anatomical snuff box tenderness. Historically these were immobilized for 10–14 days, before re-examination and repeat radiographs. Early definitive diagnosis has the potential to avoid unnecessary immobilization. Our center has previously demonstrated the potential benefit of computerized tomography (CT) scanning in the early diagnosis of scaphoid fractures.11 This follow-up study examined the implementation of a Clinical Practice Guideline (CPG) incorporating early CT in patients with clinical scaphoid fracture. We did not review patients with wrist and scaphoid fractures seen on x-rays. Previous research in our center made it difficult to compare the CPG outcomes to a historical control.
Our primary hypothesis was that early CT with this CPG would avoid unnecessary immobilization. We also hypothesized that this would result in early return to normal duties and satisfied patients.
METHODS
This was a prospective observational study of the care of a group of patients with a clinical diagnosis of scaphoid fracture presenting to a regional emergency department (ED) of a 230-bed hospital. The ED has an annual census of ~40,000 patients. The clinical practice guideline was approved via the institutional clinical governance process. These resources are freely available atwww.scaphoidfracture.com.au. The study was approved by the local Human Research Ethics Committee. The procedures followed conform to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh in 2000) and Australian ethical requirements. Informed written consent was obtained by in all participants. Patients < 18 years old also required written consent from parent or legal guardian. The study was registered on the Australian Clinical Trials Registry and conforms to International Conference on Harmonisation/Good Clinical Practice guidelines.
We designed our implementation strategy using the features described by Grimshaw et al.12 as having a high probability of being effective. First, a local development strategy to develop a CPG for scaphoid fracture was led by a multidisciplinary team with members from the orthopaedic, radiology, and emergency departments. This CPG is described below and available atwww.scaphoidfracture.com.au. Second, our dissemination strategy for this CPG involved specific educational interventions. Web-based online tutorials were available 24/7 on our intranet and atwww.meditute.org. Education sessions for medical and nursing staff were conducted and repeated to allow for staff rotations. Third, our implementation strategy included patient-specific reminders at the time of consultation: promotional flyers in every treatment room; stickers with checkboxes for improved documentation of clinical signs, including snuff box tenderness, tenderness on anterior-posterior compression of scaphoid, and tenderness on axial compression of the thumb. Scaphoid x-ray and CT were ordered on specially designed radiology request forms with checkboxes.
This study involved minimal additional cost and human resources. Clinical leaders facilitated and promoted the CPG. Our staff developed the materials, study database, and education program as a part of work duties. Our institution had already developed the web-based tutorials and maintains them on our intranet.
Patients who presented to the ED were identified by triage nursing and medical staff who gave patients a study information sheet. Trained ED faculty or residents obtained informed consent.
Inclusion criteria were as follow: age of at least 14; a mechanism of injury consistent with scaphoid trauma and tenderness in the anatomical snuff box; and normal x-rays of wrist and scaphoid. ED faculty or residents determined the x-ray diagnosis, which was later confirmed on formal report by a specialist radiologist and included in the results. Exclusion criteria were as follow: less than 14 years of age; pregnancy; unable to consent or refused consent. These criteria were consistent with published literature and reflect the scope of practice of our CPG.
CT was performed on a Siemens Somatom Sensation 64 slice CT scan (Siemens, Munich, Germany), using 1mm slices, and reported in an unblinded fashion by a radiologist. Radiation dose of extremity CT is 0.5 mSv.13 Patients with a diagnosis fracture of the scaphoid or any other fracture were immobilized in a plaster of Paris cast and referred to the orthopaedic fracture clinic for further treatment. The patient and CT images were reviewed by orthopaedic consultant or registrar to confirm diagnosis, and duration of plaster and further treatment were recorded.
Patients with normal CT and without significant pain (rated <5/10) were allowed to commence mobilizing the wrist immediately. Supportive plaster was offered to patients if they had significant pain. They were subsequently surveyed at day 10 with a telephone interview and asked about loss of function and to rate ongoing pain on a scale of 1–10. Patients with pain >4/10 were reviewed and MRI arranged. Our final diagnosis of “no fracture” was based on resolution of symptoms at day 10, or normal MRI. We asked patients at this stage if they had days off work and how many, and if they had returned to normal duties. We recorded occupation and asked participants if they would have been able to perform normal duties if they had plaster immobilization for 10 days. A research assistant recorded demographic details, reviewed each medical record to ensure that the patient met the criteria for the study, recorded the initial x-ray and subsequent CT reports, and any additional medical imaging performed.
The patient information sheet advised that the CPG involved early CT instead of the historical immobilization for 10 days and repeat imaging and review. Patient satisfaction with their treatment was rated on a scale of 1–5, poor-excellent, under the headings: “overall impression of new protocol,” “explanation of management protocol,” “waiting times,” “attention to detail,” “quality of service,” “patient centeredness,” and “met or exceeded expectations.”
We performed a power calculation using MedCalc for Windows, version 9.3.0.0 (MedCalc Software, Mariakerke, Belgium). A sample of 81 would give 90% power to detect a result of 98% for sensitivity, or negative predictive value (a= 0.05, b = 0.9). Graphpad quickcalcs (GraphPad Software San Diego, California) was used to calculate confidence intervals for percentages and means.
RESULTS
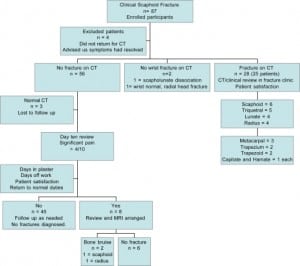
We enrolled 87 patients between April 2006 and March 2008, 80 of whom completed the study protocol (Figure 1). We extended the original recruitment period from one to two years to obtain a larger sample size. The four patients who withdrew without returning for CT cited resolution of symptoms, with one patient being advised by their general practitioner that CT was not necessary.
Forty-one patients were male, median age was 25 (interquartile range, 18–43). Clinical examination findings from medical staff included anatomical snuff box tenderness present in all patients (inclusion criteria). Tenderness on axial compression of thumb present in 6/6 scaphoid fractures, 21/25 patients with fractures overall, and 43/53 patients without fracture. Tenderness on anterior-posterior compression of scaphoid present in 6/6 scaphoid fractures, 22/25 patients with fractures overall, and 44/53 of patients without fracture. CT was performed on average 1.3 days post injury (range 1–10).
There were 28 fractures in 25 patients. These fractures included scaphoid (6 *one with lunate), triquetral (5 *one with lunate), radius (4), lunate (4), metacarpal (3), trapezoid (2), trapezium (2), capitate and hamate (1 each in same patient). Retrospective review of the original x-ray report by specialist radiologist revealed that one scaphoid and one triquetral fractures were reported (but not identified prior to CT), one scaphoid and one triquetral were reported as “possible fracture” (with further imaging recommended). One radiologist report of fracture radius (ED faculty report normal) was not confirmed when the CT was reported. Two patients had no fracture on wrist CT, but other injuries occurred: one patient had scapholunate dissociation, and the other had normal wrist but a co-existent fracture of the radial head. They were not analysed in the group with “normal CT.”
Of the 56 patients with a normal CT scan, three were lost to follow up (unable to be contacted via phone or mail). Fifty-three with no fracture on CT were further analyzed. These patients reported a mean pain score of 1.6/10 (range 0–10) on review, with 29/53 reporting ongoing pain and 20/53 patients ongoing reduced function. For the 8/53 with significant symptoms at day 10, MRI did not reveal any missed cortical fractures, but two patients had bone bruises (one scaphoid, one radius). The two with bone bruising skewed the results for duration of plaster; the scaphoid bone bruise had duration of plaster lasting 56 days (Figure 2).
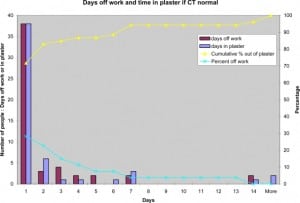
Sensitivity of CT (compared to final diagnosis) was 100% (95% CI 93.5–100) and negative predictive-value was 100% (95% CI 93.5–100%). Participants spent a mean 2.85 days (range 0–56) in plaster, and while only 25/53 required time off work, the mean time off was 1.6 days (range 0–14). Most participants had three or less days off work (45/53), with 51/53 back at work by day seven. While 39/53 participants had already returned to normal duties before day 10, only 10/53(19%) felt they could have returned to normal duties if they had plaster immobilization.
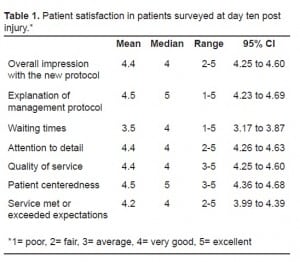
The average patient satisfaction score for waiting times was lower compared to other questions (Table 1). This was supported by the qualitative feedback provided, with a number of comments relating to waiting “too long” to be told the CT report was normal. There were no significant differences between other scores, with average scores of 4.2–4.5, reflecting relatively good patient satisfaction with their management using the protocol.
DISCUSSION
The aim of this study was to evaluate implementation of our CPG for patients presenting with clinical scaphoid fracture, incorporating early CT. It has previously been suggested that well designed CPGs guide practice and improve quality and efficiency, as well as saving costs.14–16 To be effective, a CPG must have adequate administrative support and be designed to support medical staff in their practice, without being seen as disempowering.15
Our previous research demonstrated 96.7% negative predictive value for fracture in this population, with no missed scaphoid fractures.11 This study involved collaboration between the orthopaedic, radiology and emergency departments, with agreement that there was enough evidence to support the use of early CT in our CPG. We developed a guideline with a clear purpose, scope, and inclusion and exclusion criteria. In implementing the evidence, our CPG ensured the targeted use of radiological investigations in a consistent manner by ED medical staff.
Other alternatives to plain x-rays for scaphoid fracture diagnosis have been described. Bone scan at day 4 post injury17,18 has excellent sensitivity and negative predictive values (95–100%), although the poor specificity (60–95%) and positive predictive value (65%) represent a limitation to its use.17,19,20 Ultrasound, while a potentially useful diagnostic tool, has not been shown to diagnose fractures of adjacent bones masquerading as or associated with scaphoid injuries, as is the case with other advanced imaging techniques.21
MRI has been demonstrated to be accurate in the diagnosis of scaphoid fractures, with a reported 100% negative predictive value, sensitivity and specificity.5,6,22–26 It is now regarded by many as the gold standard for the imaging of suspected scaphoid fractures when initial radiographs are normal.3,27
CT has been shown to be useful in the diagnosis of scaphoid fractures (sensitivity 72–100% and specificity of 80–100%),7,11,28–35 and is superior to other modalities in the detection of clinically significant displacement, which is fundamental to potentially poor clinical outcomes.28,36
In Australian practice, CT is roughly half the cost of MRI and has a significantly higher availability.37,38 Additionally, CT scans may be ordered by any medical practitioner, unlike MRI which generates a Medicare rebate only when ordered by registered specialists, thus generally restricting its use. In our population, patients with scaphoid tenderness and normal plain x-ray and a normal early CT scan were only immobilized to treat symptoms. For the 15% with significant symptoms at day 10, the use of MRI did not demonstrate any missed fractures, but two patients had bone bruises and required longer immobilization. This confirms both the excellent negative predictive value of CT and the need for further medical review if symptoms persist.
Eighty-five percent of patients with normal CT scans had less than three days in plaster, and less time in plaster may mean earlier return to normal duties. Using a traditional approach to scaphoid fracture, all of these patients would have had 10 days of plaster immobilization, with 43/53 of our patients reporting they would have been unable to return to normal duties. Overall our patients were highly satisfied with their management (score 4.2/5). To our knowledge this is the first study to publish results of patient satisfaction for management of this clinical condition.
Several studies have highlighted the difficulties of implementing and using clinical guidelines to direct practice in the diagnosis of clinical scaphoid fracture. In the absence of established practice guidelines there tends to be marked variation in the approach to this condition.39 Where guidelines have been developed, the use and knowledge of them is often poor. This may be especially relevant in clinical settings such as EDs with high staff turnover.37
We have demonstrated the successful implementation of a CPG for diagnosis of occult scaphoid and carpal fractures. Generalized use of such a guideline requires a balance between expert consensus and local resources. While the British guideline for the diagnosis of scaphoid fracture is currently being updated, most American guidelines rank MRI over CT in situations where plain radiography is normal.39 As yet there is no national Australian guideline.
To improve the probability of success at a local level we found Grimshaw’s13 principles to be useful. Our study provides evidence to support both early CT and a CPG in current practice, especially given the recommendations that use of guidelines could be improved. Our research has the potential to change current practice. It is possible that national bodies, institutions, or clinicians at a local level may decide to place a different emphasis on different medical imaging technologies. Issues such as access, availability and cost may be subject to local variation, and follow up may vary between EDs, general practitioners and Fracture Clinics.
LIMITATIONS
Rather than comparing CT to a reference standard such as MRI, we have assessed the performance of early CT in a clinical practice guideline for suspected scaphoid fracture. We had a safety net with all patients who had persisting symptoms despite a normal CT receiving an MRI, yet missed fractures are still possible. Our reported figure of sensitivity and negative predictive value should be interpreted with some caution.
All patients with CT diagnosis of scaphoid fracture were reviewed in our fracture clinic at 10 days by an orthopedic surgeon or specialist registrar (resident), who agreed with the original CT report after review of both the patient and the CT images. It is possible that some patients may have had a false positive diagnosis on CT, and hence specificity and positive predictive value are not reported.
Patient satisfaction answers may have been biased by the word “new” in front of protocol, and by the interview process. Time off work and return to normal duties will depend on the patient population, and not necessarily be applicable to other populations.
CONCLUSION
Successful implementation of a CPG in our institution resulted in early diagnosis using CT, including scaphoid and other fractures. Patients with a normal CT avoided unnecessary periods of plaster immobilization, returned to work and normal duties earlier, and were satisfied with this approach.
Footnotes
Supervising Section Editor: Paul Walsh, MD, MSc
Submission history: Submitted April 24, 2009; Revision Received September 24, 2009; Accepted September 29, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Address for Correspondence: Dr Jaycen Cruickshank, MBBS, FACEM, MCR, Department of Emergency Medicine, Ballarat Health Services, Ballarat, 3350, Victoria, Australia
Email: jaycenc@bhs.org.au
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. This study was funded by Ballarat Health Services, supported by an “implementing the evidence” research grant from the National Institute of Clinical Studies.
REFERENCES
1. Esberger DA. What value the scaphoid compression test? J Hand Surg Br. 1994;19:748–9.[PubMed]
2. Parvizi J, Wayman J, Kelly P, Moran CG. Combining the clinical signs improves diagnosis of scaphoid fractures. A prospective study with follow-up. J Hand Surg Br. 1998;23:324–7. [PubMed]
3. Brydie A, Raby N. Early MRI in the management of clinical scaphoid fracture. [see comment] Br J Radiol. 2003;76:296–300. [PubMed]
4. Dorsay TA, Major NM, Helms CA. Cost-effectiveness of immediate MR imaging versus traditional follow-up for revealing radiographically occult scaphoid fractures. [see comment] AJR Am J Roentgenol. 2001;177:1257–63. [PubMed]
5. Gaebler C, Kukla C, Breitenseher M, et al. Magnetic resonance imaging of occult scaphoid fractures.J Trauma. 1996;41:73–6. [PubMed]
6. Hunter JC, Escobedo EM, Wilson AJ, et al. MR imaging of clinically suspected scaphoid fractures.AJR Am J Roentgenol. 1997;168:1287–93. [PubMed]
7. Roolker W, Tiel-van Buul MM, Ritt MJ, et al. Experimental evaluation of scaphoid X-series, carpal box radiographs, planar tomography, computed tomography, and magnetic resonance imaging in the diagnosis of scaphoid fracture. J Trauma. 1997;42:247–53. [PubMed]
8. Tiel-van Buul MM, van Beek EJ, Dijkstra PF, Bakker AD, Griffioen FM, Broekhuizen TH. Radiography of the carpal scaphoid. Experimental evaluation of “the carpal box” and first clinical results. Inves Radiol. 1992;27:954–9.
9. Brondum V, Larsen CF, Skov O. Fracture of the carpal scaphoid: frequency and distribution in a well-defined population. Eur J Radiol. 1992;15:118–22. [PubMed]
10. Pillai A, Jain M. Management of clinical fractures of the scaphoid: results of an audit and literature review. Eur J Emerg Med. 2005;12:47–51. [PubMed]
11. Cruickshank J, Meakin A, Breadmore R, et al. Early computerized tomography accurately determines the presence or absence of scaphoid and other fractures. Emerg Med Australas.2007;19:223–8. [PubMed]
12. Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342:1317–22. [PubMed]
13. Cross TM, Smart RC, Thomson JE. Exposure to diagnostic ionizing radiation in sports medicine: assessing and monitoring the risk. Clin J Sport Med. 2003;13:164–70. [PubMed]
14. Little AB, Whipple TW. Clinical pathway implementation in the acute care hospital setting. J Nurs Care Qual. 1996;11:54–61. [PubMed]
15. Abbott J, Hronek C, Mirecki JK. The leap to automating clinical pathways. J Healthc Resour Manag. 1995;13:8–16. [PubMed]
16. Jousimaa J, Kunnamo I, Makela M. An implementation study of the PDRD primary care computerized guidelines. Scand J Prim Health Care. 1998;16:149–53. [PubMed]
17. Beeres FJ, Hogervorst M, Den Hollander P, et al. Diagnostic strategy for suspected scaphoid fractures in the presence of other fractures in the carpal region. J Hand Surg Br. 2006;31:416–8.[PubMed]
18. Akdemir UO, Atasever T, Sipahiolu S, Turkolmez S, Kazimolu C, Sener E. Value of bone scintigraphy in patients with carpal trauma. Ann Nucl Med. 2004;18:495–9. [PubMed]
19. Tiel-van Buul MM, Broekhuizen TH, van Beek EJ, et al. Choosing a strategy for the diagnostic management of suspected scaphoid fracture: a cost-effectiveness analysis. [see comment] J Nucl Med. 1995;36:45–8. [PubMed]
20. Murphy DG, Eisenhauer MA, Powe J, et al. Can a day 4 bone scan accurately determine the presence or absence of scaphoid fracture? Ann Emerg Med. 1995;26:434–8. [PubMed]
21. Fusetti C, Poletti PA, Pradel PH, et al. Diagnosis of occult scaphoid fracture with high-spatial-resolution sonography: a prospective blind study. J Trauma. 2005;59:677–81. [PubMed]
22. Cook PA, Yu JS, Wiand W, et al. Suspected scaphoid fractures in skeletally immature patients: application of MRI. J Comput Assist Tomogr. 1997;21:511–5. [PubMed]
23. Fowler C, Sullivan B, Williams LA, et al. A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture. Skeletal Radiol. 1998;27:683–7. [PubMed]
24. Tiel-van Buul MM, van Beek EJ. Value of MR imaging in the detection of occult scaphoid fractures. [comment] Radiology. 1998;206:291–2. [PubMed]
25. Breitenseher MJ, Metz VM, Gilula LA, et al. Radiographically occult scaphoid fractures: value of MR imaging in detection. [see comment] Radiology. 1997;203:245–50. [PubMed]
26. Kumar S, O’Connor A, Despois M, et al. Use of early magnetic resonance imaging in the diagnosis of occult scaphoid fractures: the CAST Study (Canberra Area Scaphoid Trial) N Z Med J.2005;118:U1296. [PubMed]
27. Johnson KJ, Haigh SF, Symonds KE. MRI in the management of scaphoid fractures in skeletally immature patients. Pediatr Radiol. 2000;30:685–8. [PubMed]
28. Lozano-Calderon S, Blazar P, Zurakowski D, et al. Diagnosis of scaphoid fracture displacement with radiography and computed tomography. J Bone Joint Surg Am. 2006;88:2695–703. [PubMed]
29. Adey L, Souer JS, Lozano-Calderon S, et al. Computed tomography of suspected scaphoid fractures. J Hand Surg Am. 2007;32:61–6. [PubMed]
30. Kusano N. Diagnosis of Occult Scaphoid Fracture: A Comparison of Magnetic Resonance Imaging and Computed Tomography Techniques. Tech Hand Up Extrem Surg. 2002;6:119–23. [PubMed]
31. Tiel-van Buul MM, van Beek EJ, Borm JJ, et al. The value of radiographs and bone scintigraphy in suspected scaphoid fracture. A statistical analysis. J Hand Surg Br. 1993;18:403–6. [PubMed]
32. Breederveld RS, Tuinebreijer WE. Investigation of computed tomographic scan concurrent criterion validity in doubtful scaphoid fracture of the wrist. J Trauma. 2004;57:851–4. [PubMed]
33. Memarsadeghi M, Breitenseher MJ, Schaefer-Prokop C, et al. Occult scaphoid fractures: comparison of multidetector CT and MR imaging–initial experience. Radiology. 2006;240:169–76.[PubMed]
34. Sanders WE. Evaluation of the humpback scaphoid by computed tomography in the longitudinal axial plane of the scaphoid. J Hand Surg Am. 1988;13:182–7. [PubMed]
35. Haisman JM, Rohde RS, Weiland AJ., American Academy of Orthopaedic S Acute fractures of the scaphoid. J Bone Joint Surg Am. 2006;88:2750–8. [PubMed]
36. Ring D, Jupiter JB, Herndon JH. Acute fractures of the scaphoid. J Am Acad Orthop Surg.2000;8:225–31. [PubMed]
37. Tai CC, Ramachandran M, McDermott ID, Ridgeway S, Mirza Z. Management of suspected scaphoid fractures in accident and emergency departments–time for new guidelines. Ann R Coll Surg Engl. 2005;87-5:353–7. [PMC free article] [PubMed]
38. N’Dow J, N’Dow K, Maffulli N, Page G. The suspected scaphoid fracture. How useful is a unit policy? Bulletin of the Hospital for Joint Diseases. 1998;57-2:93–5.
39. Groves AM, Kayani I, Syed R, et al. An international survey of hospital practice in the imaging of acute scaphoid trauma. AJR Am J Roentgenol. 2006;187:1453–6. [PubMed]


