| Author | Affiliation |
|---|---|
| Morgan D Wilbanks, MD | University of Alabama at Birmingham, School of Medicine, Birmingham, Alabama |
| James W Galbraith, MD | University of Alabama at Birmingham, Department of Emergency Medicine, Birmingham, Alabama |
| William M Geisler, MD, MPH | University of Alabama at Birmingham, Department of Medicine, Birmingham, Alabama |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
The clinical presentation of genital Chlamydia trachomatis infection (chlamydia) in women is often indistinguishable from a urinary tract infection. While merited in the setting of dysuria, emergency department (ED) clinicians do not routinely test for chlamydia in women. The primary aim of our study was to evaluate the frequency of chlamydia testing among women presenting to the ED with dysuria.
Methods
We conducted a retrospective chart review of women 19–25 years of age presenting with dysuria to an urban ED and who had been coded with urinary tract infection (UTI) as their primary diagnosis (ICD-9 599.0) from October 2005 to March 2011. We excluded women who were pregnant, had underlying anatomical or neurological urinary system pathology, had continuation of symptoms from UTI or a sexually transmitted infection (STI) diagnosed elsewhere, or were already on antibiotics for a UTI or STI. We identified the rates of sexual history screening, pelvic examination and chlamydia assay testing and evaluated predictors using univariate and multivariate analyses.
Results
Of 280 women with dysuria and a UTI diagnosis, 17% were asked about their sexual history, with 94% reporting recent sexual activity. Pelvic examination was performed in 23%. We were unable to determine the overall chlamydia prevalence as only 20% of women in the cohort were tested. Among the 20% of women tested for chlamydia infection, 21% tested positive. Only 42% of chlamydia-positive women were prescribed treatment effective for chlamydia (azithromycin or doxycycline) at their visit; the remaining were prescribed UTI treatment not effective against chlamydia. Predictors of sexual history screening included vaginal bleeding (OR 5.4, 95% CI=1.5 to 19.6) and discharge (OR 2.8, 95% CI=1.1 to 6.9). Predictors of a pelvic examination being performed included having a complaint of vaginal discharge (OR 11.8, 95% CI=4.2 to 32.9), a sexual history performed (OR 2.5, 95% CI=1.1 to 5.8), abdominal pain (OR 2.2, 95% CI=1.1 to 4.4), or pelvic pain (OR 15.3, 95% CI=2.5 to 92.2); a complaint of urinary frequency was associated with a pelvic examination not being performed (OR 0.34, 95% CI=0.13 to 0.86).
Conclusion
Sexual histories, pelvic examinations, and chlamydia testing were not performed in the majority of women presenting with dysuria and diagnosed with UTI in the ED. The performance of a sexual history along with the availability of self-administered vaginal swab and first-void urine-based chlamydia tests may increase identification of chlamydia infection in women with dysuria.
INTRODUCTION
Chlamydia trachomatis infection (chlamydia) is the most prevalent bacterial sexually transmitted infection (STI) in the United States, with over 1.4 million cases reported in 2011.1 While the majority of cases are asymptomatic, chlamydia can present with dysuria (i.e., “acute urethral syndrome”) and resemble a urinary tract infection (UTI). This poses a diagnostic dilemma for providers as UTI and chlamydia have different clinical courses and treatments. Untreated chlamydia can cause serious complications, including pelvic inflammatory disease, infertility, and ectopic pregnancy. For women with a possible chlamydia-associated syndrome, ascertaining demographics and a sexual history can be used to stratify risk, as chlamydia rates are disproportionately higher in adolescents/young adults, African Americans, and those with new or multiple sexual partners.1,2 Furthermore, high STI rates have been reported in women evaluated in an urban emergency department (ED) and diagnosed with UTI.3
The Centers for Disease Control and Prevention (CDC) recommends that sexually active women <25 years of age and older women at risk receive annual chlamydia screening. Approximately half of eligible women receive screening,4 and symptomatic chlamydia infections remain under-recognized in ED settings.3 Our study examined whether women presenting to a large urban ED with dysuria and diagnosed with a UTI had a sexual history performed, underwent pelvic examination, or received chlamydia testing, as well as which factors predicted these outcomes.
METHODS
Study Design
We retrospectively reviewed electronic medical records (EMRs) of female ED patients with a primary diagnosis of UTI by ICD-9 code and a chief complaint of dysuria. The study was approved by the University of Alabama at Birmingham Institutional Review Board.
Study Setting and Population
We evaluated females 19–25 years of age presenting to an urban ED (>75,000 annual adult visits) from October 2005 to March 2011. The upper age limit of 25 was chosen as this is the age cutoff for CDC-recommended annual chlamydia screening in sexually active women. We included females with primary ICD-9 code for UTI (ICD-9 599.0) and a chief complaint of dysuria through review of the ED physician’s EMR documentation for the visit. No secondary diagnoses by ICD-9 were excluded. We excluded patients on the basis of pregnancy, current or recent treatment for UTI/STI, continuation of symptoms from UTI/STI diagnosed or treated elsewhere, or underlying anatomical or neurological urinary system pathology.
Study Protocol
We compiled records based on ICD-9 coding and inclusion and exclusion criteria. We reviewed the EMR for eligible subjects and collected the following data onto standardized collection forms: demographics, symptoms, sexual history, prior STI, results of pelvic examination and diagnostic testing, and treatment.
Data Analysis
We evaluated predictors of having a sexual history performed, receiving a pelvic examination, and receiving chlamydia testing initially by univariate analyses using chi-squared or Fisher’s exact test. We then evaluated variables significant at the α=0.10 level in a multivariable logistic regression model. Analyses were performed using Stata (Stata Corp. Release 8.0, College Station, TX).
RESULTS
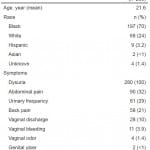
Characteristics of 280 eligible women evaluated are shown in Table. The majority were African American. In addition to dysuria, 29% reported urinary frequency. Abdominal pain was reported frequently (32%), while genital symptoms were reported less frequently, with complaints of vaginal discharge being present in 10%. Prior chlamydia was documented in 8%.
Table. Patient characteristics of women presenting with dysuria.
 Only 47 (17%) women were asked questions pertaining to a sexual history, with 44 (94%) reporting recent activity. A sexual history was performed more often in women reporting vaginal bleeding (55% versus 15%, p=0.004), pelvic pain (45% versus 16%, p=0.023), or vaginal discharge (39% versus 14%, p=0.001), and less often in those reporting urinary frequency (10% versus 20%, p=0.048). However, a sexual history was not performed in the majority of women reporting vaginal discharge (60%), pelvic pain (54%), or vaginal bleeding (45%). Having a sexual history performed was not associated with race or other symptoms. On multivariate analysis, having a sexual history performed remain predicted by the presence of vaginal bleeding symptoms (OR 5.4, 95% CI=1.5 to 19.6) or vaginal discharge (OR 2.8, 95% CI=1.1 to 6.9).
Only 47 (17%) women were asked questions pertaining to a sexual history, with 44 (94%) reporting recent activity. A sexual history was performed more often in women reporting vaginal bleeding (55% versus 15%, p=0.004), pelvic pain (45% versus 16%, p=0.023), or vaginal discharge (39% versus 14%, p=0.001), and less often in those reporting urinary frequency (10% versus 20%, p=0.048). However, a sexual history was not performed in the majority of women reporting vaginal discharge (60%), pelvic pain (54%), or vaginal bleeding (45%). Having a sexual history performed was not associated with race or other symptoms. On multivariate analysis, having a sexual history performed remain predicted by the presence of vaginal bleeding symptoms (OR 5.4, 95% CI=1.5 to 19.6) or vaginal discharge (OR 2.8, 95% CI=1.1 to 6.9).
Pelvic examination was performed in 23%, more often in women with pelvic pain (82% versus 20%, p<0.001), vaginal discharge (79% versus 16%, p<0.001), vaginal bleeding (64% versus 21%, p=0.003), a sexual history documented (35% versus 12%, p<0.001), or abdominal pain (33% versus 17%, p=0.003), and less often in women with urinary frequency (9% versus 28%, p<0.001). This was not associated with race or other symptoms. On multivariate analysis, having a pelvic examination performed remained predicted by a complaint of vaginal discharge (OR 11.8, 95% CI=4.2 to 32.9) or having a sexual history performed (OR 2.5, 95% CI=1.1 to 5.8), pelvic pain (OR 15.3, 95% CI=2.5 to 92.2) or abdominal pain (OR 2.2, 95% CI = 1.1 to 4.4); a complaint of urinary frequency was associated with a pelvic examination less often being performed (OR 0.34, 95% CI=0.13 to 0.86).
Chlamydia testing was performed in 56 (20%) women (71% of women receiving a pelvic examination), more often in women with vaginal discharge (75% versus 14%, p<0.001), pelvic pain (72% versus 18%, p<0.001), having a sexual history performed (45% versus 15%, p<0.001), vaginal bleeding (45% versus 19%, p=0.047), or abdominal pain (32% versus 14%, p<0.001), and less often in women with urinary frequency (7% vs. 25%, p<0.001). Having chlamydia testing performed was not associated with race or other symptoms. On multivariate analysis, having chlamydia testing performed remain predicted by having a complaint of vaginal discharge (OR 11.3, 95% CI=4.2 to 30.1) or a sexual history performed (OR 3.4, 95% CI=1.5 to 7.9), pelvic pain (OR 8.4, 95% CI=1.6 to 44.1) or abdominal pain (OR 2.9, 95% CI=1.4 to 6.1); a complaint of urinary frequency was associated with chlamydia testing not being performed (OR 0.34, 95% CI=0.13 to 0.94).
Of 56 women tested for chlamydia, 12 (21%) tested positive. Only 7 of 23 (30%) women with prior chlamydia were tested, and 3 of these 7 (42%) tested positive. Of women with dysuria as their only symptom, 67% had a negative urinary nitrite; however, only 7% received chlamydia testing. Of 12 women with a positive chlamydia test, 83% had a negative urinary nitrite. Only 5 (42%) of chlamydia-positive women were prescribed CDC-recommended chlamydia treatment (azithromycin or doxycycline) at their visit; the remaining were prescribed UTI treatment not effective against chlamydia (trimethoprim-sulfamethoxazole or ciprofloxacin).
DISCUSSION
We found women 19–25 years of age presenting to an ED with dysuria and receiving a UTI diagnosis infrequently had sexual history, pelvic examination, or chlamydia testing performed (all <20%), confirming that chlamydia is an under-recognized etiology of dysuria seen in EDs. Although most chlamydia-infected women are asymptomatic, dysuria in these women (acute urethral syndrome) is well described.5 We found that 21% of our study population receiving a chlamydia test were positive, supporting that this is a population for which testing is appropriate. However, since only 20% received chlamydia testing, there were likely missed opportunities for chlamydia diagnosis and treatment, leaving infected patients at risk for chlamydia complications. Most UTI treatment regimens are not effective for chlamydia.
We found that select genital symptoms were associated with having a sexual history performed and receiving a pelvic examination and chlamydia testing. Most genital symptoms are nonspecific for chlamydia and it is likely that the chlamydia positivity rate would have been high in women without genital symptoms. However, most women without genital symptoms did not receive testing. Though we do not suggest every woman presenting to an ED with dysuria undergo chlamydia testing, asking a few additional questions may allow a provider to stratify chlamydia risk and the need for testing. Females in this age range who have had recent unprotected intercourse, multiple sexual partners, or prior chlamydia may be at higher risk and are appropriate for chlamydia testing. Because the sensitivity of urine nitrite in diagnosing bacterial UTI varies widely in the literature,6 a negative nitrite should not necessarily exclude UTI from the differential; rather, negative nitrites in the setting of positive leukocyte esterase may prompt a provider to also consider chlamydia testing in sexually-active women.
The availability of highly sensitive nucleic acid amplification tests (NAAT) for C. trachomatis that can be performed on a self-administered vaginal swab (SAVS) or first-void urine samples should expedite screening in the ED. In busy ED settings, the option of performing chlamydia testing on a SAVS or first-void urine rather than having to perform pelvic examinations (when not necessary for other gynecologic concerns) might be preferred by providers and patients. Because NAAT has a higher sensitivity on SAVS samples compared to first-void urine samples (i.e., detects more chlamydia infections in SAVS samples), the Centers for Disease Control and Prevention currently recommends SAVS as the optimal specimen type for chlamydia screening in women.8 In addition, first-void urine samples are difficult to obtain in the ED due to the preference for mid-stream urine collection for UTI evaluation at the initiation of the visit. For this reason, a SAVS performed by the patient would be the best method of sample collection.
Since access to healthcare could prevent some women from receiving routine chlamydia screening by a primary care provider, an ED visit for urinary symptoms might be their only opportunity to have chlamydia diagnosed and treated.
LIMITATIONS
Our study took place in an urban ED that treats a large number of high-risk patients and our results may not be applicable to other populations. The retrospective study design may have limited accuracy and completeness of data extracted from ED providers’ documentation, and there could be bias in types of information recorded by providers. It is possible that some sexual histories obtained from ED providers were not recorded in the EMR. Follow-up data on women testing chlamydia-positive were not available and attempts to contact individuals in this study regarding future STI testing and results were not performed.
CONCLUSION
Women presenting to an ED with dysuria and diagnosed with a UTI did not routinely have a sexual history performed or undergo pelvic examination or chlamydia testing. When chlamydia testing was performed, the positivity rate was high. The majority of chlamydia-infected women received UTI treatment not effective for chlamydia. The performance of a sexual history along with the availability of self-administered vaginal swab and first-void urine-based chlamydia tests may increase identification of chlamydia infection in women with dysuria.
ACKNOWLEDGEMENTS
We thank Henry Wang, MD, and Joel Rodgers, MA, for their contributions.
Footnotes
Address for Correspondence: James W Galbraith, MD, University of Alabama at Birmingham, Department of Emergency Medicine, 619 19th Street South, JTN 266, Birmingham, AL 35249. Email: jgalbraith@uabmc.edu. 3 / 2014; 15:227 – 230
Submission history: Revision received July 15, 2013; Submitted November 26, 2013; Accepted December 5, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2011. Atlanta: U.S. Department of Health and Human Services ; 2012. Available at: http://www.cdc.gov/std/stats11/Surv2011.pdf. Accessed December 19, 2012.
2. Eggleston E, Rogers SM, Turner CF infection among 15–35 year-olds in Baltimore, MD, USA. Sex Transm Dis. 2012; 38:743-749.
3. Berg E, Benson DM, Haraszkiewcz P High prevalence of sexually transmitted diseases in women with urinary infections. Acad Emerg Med. 1996; 3:1030-1034.
4. National Committee for Quality Assurance. The state of healthcare quality 2011. Washington (DC): National Committee for Quality Assurance; 2011. 77-78.
5. Stamm WE, Wagner KF, Amsel R Causes of the acute urethral syndrome in women. New Engl J Med. 1980; 303:409-415.
6. St John A, Boyd JC, Lowes AJ The use of urinary dipstick to exclude urinary tract infection. Am J Clin Pathol. 2006; 126:428-436.
7. Yealy DM, Greene TJ, Hobbs GD Underrecognition of cervical and infections in the emergency department. Acad Emerg Med. 1997; 4:962-967.
8. Association of Public Health Laboratories and the Centers for Disease Control and Prevention. Laboratory Diagnostic Testing for Chlamydia trachomatis and Neisseria gonorrhea. Atlanta; 2009. Available at: http://www.aphl.org/aphlprograms/infectious/std/Documents/ID_2009Jan_CTGCLab-Guidelines-Meeting-Report.pdf. Accessed October 9, 2013.


