| Author | Affiliation |
|---|---|
| Rick Hong, MD | Cooper University Hospital, Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey |
| Molly Meenan, MD | Cooper University Hospital, Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey |
| Erin Prince, DO | Cooper University Hospital, Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey |
| Ronald Murphy, NREMTP | Cooper University Hospital, Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey |
| Caitlin Tambussi, BA | Cooper University Hospital, Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey |
| Rick Rohrbach, RN | Cooper University Hospital, Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey |
| Brigitte M Baumann, MD, MSCE | Cooper University Hospital, Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey |
Introduction
Materials and methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
We wanted to compare 3 existing emergency medical services (EMS) immobilization protocols: the Prehospital Trauma Life Support (PHTLS, mechanism-based); the Domeier protocol (parallels the National Emergency X-Radiography Utilization Study [NEXUS] criteria); and the Hankins’ criteria (immobilization for patients <12 or >65 years, those with altered consciousness, focal neurologic deficit, distracting injury, or midline or paraspinal tenderness).To determine the proportion of patients who would require cervical immobilization per protocol and the number of missed cervical spine injuries, had each protocol been followed with 100% compliance.
Methods
This was a cross-sectional study of patients ≥18 years transported by EMS post-traumatic mechanism to an inner city emergency department. Demographic and clinical/historical data obtained by physicians were recorded prior to radiologic imaging. Medical record review ascertained cervical spine injuries. Both physicians and EMS were blinded to the objective of the study.
Results
Of 498 participants, 58% were male and mean age was 48 years. The following participants would have required cervical spine immobilization based on the respective protocol: PHTLS, 95.4% (95% CI: 93.1–96.9%); Domeier, 68.7% (95% CI: 64.5–72.6%); Hankins, 81.5% (95% CI: 77.9–84.7%). There were 18 cervical spine injuries: 12 vertebral fractures, 2 subluxations/dislocations and 4 spinal cord injuries. Compliance with each of the 3 protocols would have led to appropriate cervical spine immobilization of all injured patients. In practice, 2 injuries were missed when the PHTLS criteria were mis-applied.
Conclusion
Although physician-determined presence of cervical spine immobilization criteria cannot be generalized to the findings obtained by EMS personnel, our findings suggest that the mechanism-based PHTLS criteria may result in unnecessary cervical spine immobilization without apparent benefit to injured patients. PHTLS criteria may also be more difficult to implement due to the subjective interpretation of the severity of the mechanism, leading to non-compliance and missed injury.
INTRODUCTION
Cervical spine injury occurs in 2–6% of all blunt trauma cases, with higher rates in patients with severe closed head injury.1–7 Even though the incidence of these injuries is low, the morbidity and mortality associated with them can be devastating; and without appropriate immobilization, 10–25% of all patients with spine injuries will deteriorate.8 Consequently, traditional emergency medical services (EMS) practice is to assume a potential cervical spine injury in any trauma patient with an appropriate mechanism of injury.9,10 Because a concern during the initial management of patients with potential cervical spine injuries is that neurological function may be further impaired by pathological motion of the injured vertebrae, full spinal immobilization of these patients consists of a cervical collar, a rigid fiberglass or plastic backboard, and stabilization of the head.11
Recently, mechanism-based immobilization practices have come under question since the immobilization process can lead to morbidity. Extrication and transfer of patients from the scene is prolonged, and immobilization itself can cause pain, respiratory compromise and decreased capillary blood flow to sacral and occipital soft tissue.12–18 Thus, the goal of current EMS cervical spine immobilization protocols is to appropriately immobilize patients at high risk of cervical spine injury while avoiding immobilization in those who are at low risk. Several protocols currently exist for EMS providers, a common one being the conventional, mechanism-based Prehospital Trauma Life Support (PHTLS) protocol. The PHTLS program was developed by the National Association of Emergency Medical Technicians in cooperation with the American College of Surgeons Committee on Trauma to promote a national standard for prehospital trauma care.19 Although the PHTLS protocol has been used since 1979, it does require immobilization for a large proportion of trauma patients, given that it is mechanism-based, as opposed to signs and symptoms based.
Due to concerns about excessive immobilization requirements via the PHTLS protocol by our EMS providers and inconsistent immobilization of trauma patients post-EMS transfer to our emergency department (ED), we set out to systematically investigate our local EMS practices. We focused on trauma patients presented to the ED only, and not to the trauma service, as the latter patients were uniformly immobilized by prehospital providers. We compared 3 EMS immobilization protocols — the PHTLS (focuses on mechanism of injury); the Domeier protocol (parallels the National Emergency X-Radiography Utilization Study [NEXUS] criteria); and the refined Hankins clinical criteria (requires immobilization for those <12 or >65 years, with altered consciousness, focal neurologic deficit, distracting injury, and midline or paraspinal tenderness) — to local EMS practices, to determine the number of patients who would require cervical immobilization.19–22 Our secondary objective was to determine the percentage of missed cervical spine injuries, had each protocol been followed with 100% compliance.
MATERIALS AND METHODS
Design
This was a cross-sectional study of local EMS practices in cervical spine immobilization in trauma patients. All trauma patients transported to the ED by EMS were prospectively screened for inclusion by trained research assistants who completed a standardized data form on all eligible patients. The form included all the variables from 3 cervical spine immobilization protocols: the PHTLS (currently in use by EMS agencies working under our medical direction), the Domeier and the Hankins protocols.19–22 Data forms were completed by the treating physicians, who were blinded to the objective of this investigation. Our primary objective was to determine the proportion of patients who required cervical spine immobilization, based on each protocol’s criteria. Our secondary objective was to determine the percentage of missed cervical spine injuries, had each protocol been followed with 100% compliance. Our institutional review board (IRB)did not require written informed consent, as no interventions were undertaken and all data forms were recoded immediately after medical record review with a unique patient identifier instead of patient names. This study was approved by our IRB, which waived the requirement for written informed consent.
Setting
The study was conducted from March to November 2010 at an urban, Level 1 trauma center with an annual ED census of 62,000 visits during the study period. Cooper University Hospital has a 2-tiered EMS system providing basic and advanced life support services. There is no standardized statewide list of criteria mandating prehospital immobilization; immobilization practices are determined by the individual EMS agencies and their medical directors.
Patients
During the study period, trained research associated assessed all patients transported to the ED by EMS for a traumatic mechanism of injury. Patients were included in this cohort if they were 18 years or older and experienced a blunt trauma that was not isolated to an extremity (e.g. crush injury to the forearm or isolated ankle sprain would be excluded). Patients that met our internal Trauma Alert activation criteria (Appendix) were immediately evaluated by the Trauma Team and were excluded from the study. We excluded these patients because insufficient immobilization of these referred patients was not a concern. All patients deemed to require a trauma evaluation were automatically placed in immobilization by the prehospital providers, so noncompliance with the PHTLS protocol did not occur. Instead, we wished to assess compliance with cervical spine immobilization criteria in a more varied population where compliance was already a concern, namely patients who presented to the ED. ED patients were screened from 9 AM – 10 PM, which corresponded to our peak ED volume periods. Enrollment occurred 7 days a week.
Protocol
Upon arrival to the ED, patients were screened and enrolled by research assistants who obtained demographic information and recorded who (EMS versus ED personnel) placed the cervical collar. Data was prospectively collected using a standardized data collection form. Demographic data, including patient age, sex, and mechanism of injury, was obtained from EMS personnel or from the patient by the trained research assistants. Additional data regarding mechanism of injury, presence of intoxication, level of consciousness and physical examination findings, reflecting variables in the PHTLS, Domeier and Hankins cervical spine immobilization criteria, was also collected.19–22 This data collection was completed by the treating physicians who were blinded to the objectives of this investigation and was recorded shortly after the history and physical examination and prior to radiologic imaging.
Medical record review was completed by one of the investigators who was blinded to the clinical characteristics (presence/absence of cervical spine immobilization and presenting signs and symptoms) of enrolled patients. The investigator reviewed medical records for results of radiographic imaging, including cervical spine series, computed tomography and magnetic resonance imaging. Completion of radiographic imaging was solely at the discretion of the treating physician. All radiographic studies were interpreted by radiologists who did not have access to our data. However, complete blinding of radiologists was not possible, due to clinical interaction between treating physicians and radiology staff. The presence or absence of cervical spine injuries was based on the final interpretation of all imaging studies. Cervical spine injuries were categorized as vertebral fractures, subluxations/dislocations and spinal cord injuries. Clinically important cervical spine injury was defined as any fracture, dislocation, or ligamentous instability requiring internal fixation or treatment with a halo, brace, or rigid collar.
Outcomes
The primary outcome measure was to determine the proportion of patients who would require cervical immobilization based on each protocol. The secondary outcome measure was to determine the number of missed cervical spine injuries given 100% compliance, which may validate the use of these protocols in the prehospital setting based on the number of missed injuries and number of unnecessary cervical immobilizations without any benefit to injured patients.
Data Analysis
We reported measurements using descriptive statistics, with means and standard deviations (SD) presented for continuous variables that were normally distributed. For nonparametric data, medians and interquartile ranges (IQR) are presented. We calculated the proportion of patients who required cervical spine immobilization, based on each protocol’s criteria. These proportions are presented with 95% confidence intervals (95% CI). The percentage of missed cervical spine injuries, had each protocol been followed with 100% compliance, is also presented. We conducted the analysis using SPSS 15.0 (SPSS Inc, Chicago, IL). Sample size was determined using a baseline estimate of 70% compliance with immobilization protocols. To achieve a 95% CI within 10%, 400 subjects were needed. Additionally, we wished to enroll enough subjects to achieve at least 10 cervical spine injuries. Based on prior studies, where cervical spine injury rates were between 2–4%, we needed a minimum of 500 subjects to achieve this goal. Thus, we endeavored to enroll 500 subjects.
RESULTS
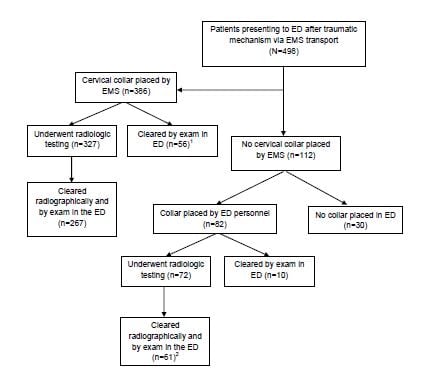
During the study period, 5,158 patients were transported to the ED by EMS. Of these, 1,340 experienced a blunt traumatic mechanism, with 371 patients with trauma isolated to a distal extremity, 259 patients <18 years of age and 189 patients evaluated only by the trauma team. This resulted in 521 eligible patients, of whom 498 were enrolled and 23 were missed, due to an enrollment attempt after radiologic imaging had been viewed by the treating physician. The majority (78%) of patients underwent cervical spine immobilization by EMS. The mean age of patients was 47.8 (19.5) years, over half of patients were male, and 85% had a complaint of pain. Median pain score was 7.0 (IQR: 4.0, 9.0) and median Glasgow coma scale score was 15 (IQR: 15, 15). Clinical and radiologic clearance of these patients, as well as the initiation of cervical spine immobilization of EMS patients by ED personnel, is outlined in the Figure.
Figure
Immobilization practices of emergency medical services (EMS) and emergency department (ED) personnel.
1Three Patients removed their cervical collars against medical advice.
2One patient removed cervical collar against medical advice.
We present criteria used for the PHTLS protocol and compliance with these criteria in Table 1. The majority of patients experienced sudden acceleration, deceleration or lateral bending forces, a fall, or a violent impact to the head or neck. At least one PHTLS criterion was noted in 95.4% of patients by the treating physician. Tables 2 and 3 present the Domeier and refined Hankins criteria, respectively. Treating physicians noted at least one Domeier criterion in 68.7% of patients and at least one Hankins criterion in 81.5% of patients.
Table 1. Implementation of Current Prehospital Trauma Life Support (PHTLS) Criteria.
| PHTLS Immobilization Criteria | Criteria noted by treating physician (N=498) | C spine collar placed by EMS | Total compliance by EMS and ED (N=498) |
|---|---|---|---|
| n (%) | n (compliance%) | n (compliance%) | |
| Anatomic deformity of spine | 2 (<1) | 2/2 (100) | 2 (100) |
| Inability to communicate | 40 (8.0) | 26/40 (65.0) | 38 (95) |
| Mechanism produced violent impact to head | 292 (58.6) | 221/292 (75.7) | 281 (96.2) |
| Mechanism produced violent impact to neck | 223 (44.8) | 186/223 (83.4) | 220 (98.7) |
| Mechanism produced violent impact to torso | 153 (30.7) | 132/153 (86.3) | 151 (98.7) |
| Mechanism produced violent impact to pelvis | 123 (24.7) | 107/123 (87.0) | 119 (96.8) |
| Patient sustained a fall | 193 (38.8) | 130/193 (67.4) | 175 (90.7) |
| Patient ejected or fall from motorized vehicle | 38 (7.6) | 31/38 (81.5) | 37 (97.4) |
| Victim of shallow water diving accident | 2 (<1) | 1/2 (50) | 1 (50) |
| Sudden acceleration, deceleration or lateral bending forces | 253 (50.8) | 214/253 (84.6) | 245 (96.8) |
| At least one PHTLS criteria present | 475 (95.4) | 367/475 (77.3) | 447 (94.1) |
EMS, emergency medical services; ED, emergency department; C spine, cervical spine
Table 2. Implementation of Domeier Criteria.
| Domeier Criteria | Criteria noted by treating physician (N=498) | C spine collar placed by EMS | Total compliance by EMS and ED (N=498) |
|---|---|---|---|
| n (%) | n (compliance%) | n (compliance%) | |
| Focal neurologic deficit present | 16 (3.2) | 14/16 (87.5) | 15 (93.8) |
| Midline spinal tenderness present | 152 (30.5) | 128/152 (84.2) | 152 (100) |
| Altered level of consciousness | 98 (19.7) | 71/98 (72.5) | 97 (99.0) |
| Intoxicated | 81 (16.3) | 56/81 (69.1) | 80 (98.8) |
| Distracting injury present | 149 (29.9) | 123/149 (82.6) | 141 (94.6) |
| At least one Domeier criteria present | 342 (68.7) | 273/342 (79.8) | 333 (97.4) |
EMS, emergency medical services; ED, emergency department; C spine, cervical spine
Table 3. Implementation of Refined Hankins Clinical Criteria.
| Hankins Criteria | Criteria noted by treating physician (N=498) | C spine collar placed by EMS | Total compliance by EMS and ED (N=498) |
|---|---|---|---|
| n (%) | n (compliance%) | n (compliance%) | |
| Extremes of age:<12 or >65 years* | 94 (18.9) | 70/94 (74.5) | 89 (94.7) |
| Altered level of consciousness | 98 (19.7) | 71/98 (72.5) | 97 (99.0) |
| Focal neurologic deficit present | 16 (3.2) | 14/16 (87.5) | 15 (93.8) |
| Distracting injury present | 149 (29.9) | 123/149 (82.6) | 141 (94.6) |
| Midline spinal/paraspinal tenderness present | 292 (58.6) | 242/292 (82.9) | 289 (99.0) |
| At least one Hankins criteria present | 406 (81.5) | 324/406 (79.8) | 392 (96.6) |
*Only >65 years was used for this investigation, as all enrolled patients were 18 years or older EMS, emergency medical services; ED, emergency department; C spine, cervical spine
Tables 4–6 demonstrate the compliance with the PHTLS, Domeier and Hankins cervical spine immobilization protocols, respectively. The following proportions of patients would have required cervical spine immobilization based on the respective protocols: PHTLS, 95.4% (95% CI: 93.1–96.9%); Domeier, 68.7% (95% CI: 64.5–72.6%); Hankins, 81.5% (95% CI: 77.9–84.7%).
Table 4. Use of cervical immobilization in patients based on Current Prehospital Trauma Life Support (PHTLS) immobilization criteria.
| Number of criteria present/positive | Cervical collar not placed by EMS | Cervical Collar placed by EMS | Total |
|---|---|---|---|
| No current criteria present/positive | 4 (17%) | 19 (83%) | 23 (100%) |
| At least one PHTLS criteria present/positive | 108 (23%) | 367 (77%) | 475 (100%) |
| Total | 112 | 386 | 498 |
EMS, emergency medical services
Table 5. Use of cervical immobilization in patients based on Domeier immobilization criteria.
| Number of criteria present/positive | Cervical collar not placed by EMS | Cervical Collar placed by EMS | Total |
|---|---|---|---|
| No current criteria present/positive | 44 (28%) | 113 (72%) | 157 (100%) |
| At least one Domeier criteria present/positive | 68 (20%) | 273 (80%) | 341 (100%) |
| Total | 112 | 386 | 498 |
EMS, emergency medical services
Table 6. Use of cervical immobilization in patients based on Refined Hankins immobilization criteria.
| Number of criteria present/positive | Cervical collar not placed by EMS | Cervical Collar placed by EMS | Total |
|---|---|---|---|
| No current criteria present/positive | 30 (33%) | 62 (67%) | 92 (100%) |
| At least one Hankins criteria present/positive | 82 (20%) | 324 (80%) | 406 (100%) |
| Total | 112 | 386 | 498 |
EMS, emergency medical services
Even though the current PHTLS criteria required the largest proportion of patients to undergo cervical spine immobilization, the actual compliance rates with the PHTLS protocol did not differ from the compliance with the other 2 non-implemented protocols: PHTLS 77.3% (95% CI:73.3–80.8%); Domeier, 79.8% (95% CI:75.2–83.8%); Hankins, 79.8% (95% CI:75.6–83.4%).
Cervical spine injuries were determined via medical record review of radiologic imaging. Of the 386 patients who underwent cervical spine immobilization by EMS, 327 underwent radiologic imaging. Of these, there were 11 vertebral fractures, 2 subluxation/dislocation injuries and 3 spinal cord injuries. Two patients had multiple injuries in this group, and all sustained a clinically important cervical spine injury, defined as any fracture, dislocation, or ligamentous instability requiring internal fixation or treatment with a halo, brace, or rigid collar. In the additional 82 patients who had a cervical collar placed in the ED, 72 of them underwent radiologic imaging. There was one vertebral fracture and one spinal cord injury in this subgroup. Both of these injuries were clinically important, as defined above. If the PHTLS cervical spine immobilization criteria had been followed by all EMS personnel and every patient with at least one positive finding had been immobilized, all 16 patients with injuries would have been immobilized appropriately 0% (95% CI: 0–23%). Complete compliance with either the Domeier or the Hankins protocols would also have resulted in appropriate cervical spine immobilization of all 16 injured patients.
DISCUSSION
In this investigation, we attempted to demonstrate the rate and appropriateness of prehospital immobilization based on the protocols and missed injuries, as well as EMS consistency with 3 cervical spine immobilization protocols using the treating physicians’ assessments of patients’ signs and symptoms as the gold standard for cervical spine immobilization at ED presentation. We chose these particular protocols as they have been implemented by many EMS agencies, though they may not be used for the EMS agencies transporting patients to our ED. Using these parameters, we demonstrated that EMS consistency with the current PHTLS protocol is 77%. Had all patients been appropriately immobilized based on at least one positive PHTLS criterion, 475 (95.4%) of enrolled patients would have required cervical spine immobilization. Factors with the lowest level of consistency included shallow water diving accident (50%), inability to communicate (65%) and fall (67%). In comparison, the percentage of patients requiring immobilization was only 69% using the Domeier criteria and 82% using the Hankins criteria. For the Domeier criteria, the lowest levels of compliance were in patients who were intoxicated (69%) and those who had an altered level of consciousness (73%). For the Hankins protocol, the lowest levels of compliance were in patients at extremes of age (75%) and, again, those with an altered level of consciousness (73%). These latter findings are not surprising, since the criteria in the Domeier and Hankins protocols with the lowest levels of compliance were solely based on clinical findings and not mechanism of injury.
The original standards for prehospital transport supported spine immobilization for patients with symptoms possibly stemming from spine injury.23 The practice of prehospital immobilization shifted from clinical indicators toward mechanism of injury due to significant failures in EDs to correctly identify patients at risk of spinal injury.24 This led to routine immobilization and imaging practices of trauma patients, which continued well into the early 1990s. As recently as 1989, 96% of the 125 North American hospitals with experience in acute trauma routinely obtained cervical radiographs as a protocol study on all patients who suffered major trauma.25 This comprehensive inclusion of trauma patients for cervical spine imaging is also reflected in the mechanism-based PHTLS cervical spine immobilization protocol, where, in our study sample, 95% of our patients should have been immobilized. Mirvis et al. questioned this practice and suggested that asymptomatic, neurologically intact patients may not need further imaging. In a sample of 408 patients with a history of major blunt trauma, 138 were mentally alert patients without symptoms referable to cervical spine injury. The investigators demonstrated the very low yield of imaging a non-displaced transverse process fracture of C7. Yet the combined cost of computed tomography and radiography per patient was $427, with total costs over $59,000.25
Others also questioned the utility of cervical spine radiography in alert, non-intoxicated and asymptomatic trauma patients and continued to demonstrate low yields of clinically relevant injuries while imaging costs escalated.26–28 The NEXUS criteria and the Canadian C-Spine Rule are the culmination of these earlier investigations. The NEXUS low-risk criteria consists of clinical criteria that identify trauma patients with a very low probability of clinically significant cervical spine injury.29 The Canadian C-Spine Rule includes both clinical indicators and mechanism of injury to assess need for radiography.30 While both of these criteria are solely intended for the determination of the need for cervical spine imaging, they have also been used to develop prehospital cervical spine immobilization protocols, such as the Hankins and especially the Domeier protocols.
The impetus for using cervical spine immobilization protocols based on clinical criteria is to reduce the frequency of unnecessary immobilization. Our results demonstrate that the requirement for cervical spine immobilization in our patient population was less using the Domeier (68.7%) and Hankins (81.5%) protocols, as compared to the PHTLS protocol (95.4%). This is particularly noteworthy since we also demonstrated that complete compliance with any of the 3 protocols would have resulted in appropriate immobilization of all 16 patients who had cervical spine and cord injuries. Why should the reduction of unnecessary immobilization in trauma patients be a priority for healthcare providers? Appropriate and effective immobilization requires time for proper patient positioning and application of immobilization devices, which extends EMS field time and delays transport to definitive care.22, 31–33 The immobilization process may also cause discomfort to patients. Pain caused by the initial trauma may be exacerbated by immobilization devices or they may lead to new pain reports in previously asymptomatic patients.22,31,34,35 If physicians are unable to differentiate the source of the presenting pain (trauma versus immobilization), this may lead to unnecessary radiographic studies, prolong the ED evaluation and further decrease overall ED throughput.12,31,36,37 Other complications due to supine immobilization include airway and respiratory compromise, increased risk of aspiration, sacral and occipital soft tissue damage, and skin ulcer formation.15–18,35,38,39 A move away from mechanism-based protocols and greater reliance on clinical indicators, as found in the Domeier and Hankins protocols, may also benefit the EMS system. Decreased use of immobilization equipment will result in reduced costs for disposable items, such as cervical collars, and replacement equipment for reusable items.31,37 Also, because EMS providers are at risk from injuries due to repeated lifting of immobilized patients, reducing this risk will support existing workforces and lessen financial compensation for work-related injuries.39 Finally, decreased run times from limiting unnecessary immobilization will lead to faster transport times and increased availability of EMS personnel for new calls.22,31–33
LIMITATIONS
There are several limitations to this investigation. First, this was a convenience sample of patients who were transported to our ED during the hours of 9 AM–10 PM. We likely missed patients who arrived during the overnight hours. However, given that our institution is the only Level 1 trauma center in the southern New Jersey area, we think that our sample is representative of our ED trauma patients. What this sample may not adequately represent is EMS immobilization practices of night shift personnel, which may change based on a different presenting population (e.g., greater proportion of intoxicated patients). A second limitation is that this study was only conducted at one center and we excluded patients who were immediately cared for by the trauma service. Thus, our findings may not be representative of other EMS systems or patient populations. This single-center study design was intentional because our secondary intent was to examine our EMS responders’ compliance with the current cervical spine immobilization protocol in trauma patients presenting to the ED. Our exclusion of patients presenting to the trauma service was intentional, as these patients are always immobilized. A third limitation is that the criteria for cervical spine immobilization were completed by the treating physician, which may have been biased. EMS personnel who are able to witness the motor vehicle collision or who are involved in the extrication of a patient may have had more information about the mechanism of injury than the treating physicians had. This bias, however, would likely have led to an under-reporting of criteria by the treating physicians, leading to an underestimate of the number of patients who should have undergone cervical spine immobilization. Alternatively, treating physicians could have obtained information about the injury from multiple sources, including the patient, EMS and witnesses at the scene. It is possible that over the course of medical evaluation and management in the ED, treating physicians may have obtained more information, leading to the reporting of a greater number of cervical spine immobilization criteria as compared to what was obtained by EMS personnel. This would have led to a higher estimate of patients who should have undergone cervical spine immobilization. We attempted to limit this effect by having our research assistants approach the treating physicians immediately after the initial patient encounter. To better address these discrepancies, future studies should have both EMS personnel and the treating physicians complete the immobilization criteria for each patient. If there are discrepancies between the two, particularly if EMS notes fewer criteria than the treating physicians, then further investigation should be undertaken to determine if the criteria are being accurately recorded or if on-scene time constraints and limited history-taking may be at fault. At this time, the available literature suggests that the agreement between EMS and emergency physician assessments for individual immobilization criteria (paralleling the Domeier and NEXUS criteria) ranges from good (K=0.81) to poor (K=0.35).9 However, when final immobilization determinations were made, EMS performed well. In only 7.7% of assessments, the emergency physician assessment indicated immobilization when the EMS did not.9 This value is almost half of our best performance with our 3 protocols, suggesting that there is a great deal of room for improvement at our institution. Finally, not every patient who had positive criteria for the current PHTLS protocol or the Domeier or Hankins protocols underwent imaging. Thus, we do not know the true rate of cervical spine injury. However, in patients who did undergo imaging, our overall incidence of cervical spinal and cord injury was 4%, which is consistent with prior studies.1–7 Comparing the sensitivity of these decision rules was not our intent; our primary objective was to examine the compliance by EMS with its current cervical spine immobilization policy. For future investigations, a larger sample size from multiple sites should be implemented to increase the total number of cervical spinal injuries. This will further aid in determining the true sensitivity of these decision rules.
CONCLUSION
In summary, of the 3 protocols we investigated the mechanism-based PHTLS protocol required immobilization of the greatest percentage of patients. Yet compliance with the PHTLS protocol did not differ from compliance with the 2 other investigated protocols that were not implemented during this investigation. Although physician-determined presence of cervical spine immobilization criteria cannot be generalized to the findings obtained by EMS personnel, our findings suggest that compliance with mechanism-based criteria may result in unnecessary cervical spine immobilization in trauma patients transported to the ED. Furthermore, due to inadequate compliance with the PHTLS protocol, 2 patients (12.5%) with clinically relevant injuries were missed. PHTLS criteria may be more difficult to implement due to the subjective interpretation of the severity of the mechanism, leading to non-compliance and missed injury. Further study is needed to determine if EMS compliance with protocols based on clinical indicators, such as the Domeier or the Hankins protocols, would be improved over current PHTLS compliance. Finally, a larger sample size will be needed to test the sensitivity of any replacement cervical spine immobilization protocol in correctly identifying patients at high risk of cervical spine and cord injuries.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Rick Hong, MD, Cooper Medical School of Rowan University, Cooper University Hospital, One Cooper Plaza, Camden, NJ, 08103. Email: hong-rick@cooperhealth.edu. 7 / 2014; 15:471 – 479
Submission history: Revision received August 13, 2013; Submitted September 19, 2013; Accepted February 21, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 . National Hospital Ambulatory Medical Care Survey: 2008 Emergency Department Summary Tables. ;
2 Sciubba DM, Petteys RJ Evaluation of blunt cervical spine injury. South Med J. 2009; 102:823-828
3 Goldberg W, Mueller C, Panacek E Distribution and patterns of blunt traumatic cervical spine injury. Ann Emerg Med. 2001; 38:17-21
4 Mattera CJ Spinal trauma: new guidelines for assessment and management in the out-of-hospital environment. J Emerg Nurs. 1998; 24:523-34
5 Crosby ET Airway management in adults after cervical spine trauma. Anesthesiology. 2006; 104:1293-1318
6 Davis JW, Phreaner DL, Hoyt DB The etiology of missed cervical spine injuries. J Trauma. 1993; 34:342-6
7 Grossman MD, Reilly PM, Gillett T National survey of the incidence of cervical spine injury and approach to cervical spine clearance in U.S. trauma centers. J Trauma. 1999; 47:684-90
8 Podolsky S, Baraff LF, Simon RR Efficacy of cervical spine immobilization methods. J Trauma. 1983; 23:461-5
9 Brown LH, Gough JE, Simonds WB Can EMS providers adequately assess trauma patients for cervical spine injury?. Prehospital Emergency Care. 1998; 2:33-36
10 Domeier RM, Evans RW, Swor RA The reliability of prehospital clinical evaluation for potential spinal injury is not affected by the mechanism of injury. Prehosp Emerg Care. 1999; 3:332-7
11 Hadley MN, Walters BC, Grabb PA Guidelines for the management of acute cervical spine and spinal cord injuries. ClinNeurosurg. 2002; 49:407-98
12 Vaillancourt C, Charette M, Kasaboski A Evaluation of the safety of C-spine clearance by paramedics: design and methodology. BMC Emerg Med. 2011; 11:1-11
13 Cross DA, Baskerville J Comparison of perceived pain with different immobilization techniques. Prehosp Emerg Care. 2001; 5:270-4
14 Totten VY, Sugarman DB Respiratory effects of spinal immobilization. Prehosp Emerg Care. 1999; 3:347-52
15 Bauer SJ, Kowalski R Effect of spinal immobilization devices on pulmonary function in the healthy, nonsmoking man. Ann Emerg Med. 1988; 17:915-918
16 Hauswald M, Hsu M, Stockoff C Maximizing comfort and minimizing ischemia: a comparison of four methods of spinal immobilization. Prehosp Emerg Care. 2000; 4:250-2
17 Krell JM, McCoy MS, Sparto PJ Comparison of the Ferno Scoop Stretcher with the long backboard for spinal immobilization. Prehosp Emerg Care. 2006; 10:46-51
18 Sheerin F, de Frein R The occipital and sacral pressures experienced by healthy volunteers under spinal immobilization: a trial of three surfaces. J Emerg Nurs. 2007; 33:447-50
19 Salomone JP, Pons PT . Prehospital Trauma Life Support. 2011;
20 Domeier RM, Evans RW, Swor RA Prehospital clinical findings associated with spinal injury. Prehosp Emerg Care. 1997; 1:11-15
21 Domeier RM, Swor RA, Evans RW Multicenter prospective validation of prehospital clinical spinal clearance criteria. J. Trauma. 2002; 53:744-750
22 Hankins DG, Rivera-Rivera EJ, Ornato JP Spinal immobilization in the field: clinical clearance criteria and implementation. Prehosp Emerg Care. 2001; 5:88-93
23 . Emergency Care and Transportation of the Sick and Injured. 1971; :111-5
24 Bohlman HH Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979; 61:1119-42
25 Mirvis SE, Diaconis JN, Chirico PA Protocol-driven radiologic evaluation of suspected cervical spine injury: efficacy study. Radiology. 1989; 170:831-4
26 Gonzalez RP, Fried PO, Bukhalo M Role of clinical examination in screening for blunt cervical spine injury. J Am Coll Surg. 1999; 189:152-7
27 Hoffman JR, Schriger DL, Mower W Low-risk criteria for cervical-spine radiography in blunt trauma: a prospective study. Ann Emerg Med. 1992; 21:1454-60
28 Velmahos GC, Theodorou D, Tatevossian R Radiographic cervical spine evaluation in the alert asymptomatic blunt trauma victim: much ado about nothing. J Trauma. 1996; 40:768-74
29 Hoffman JR, Mower WR, Wolfson AB Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000; 343:94-9
30 Stiell IG, Wells GA, Vandemheen K The Canadian cervical spine radiography rule for alert and stable trauma patients. JAMA. 2001; 286:1841-8
31 Cone DC, Wydro GC, Mininger CM Current practice in clinical cervical spine clearance: implication for EMS. Prehosp Emerg Care. 1999; 3:42-6
32 McHugh TP, Taylor JP Unnecessary out-of-hospital use of full spinal immobilization. Acad Emerg Med. 1998; 5:278-80
33 Orledge JD, Pepe PE Out-of-hospital spinal immobilizations: is it really necessary?. Acad Emerg Med. 1998; 5:203-4
34 Chan D, Goldberg R, Tascone A The effect of spinal immobilization on healthy volunteers. Ann Emerg Med. 1994; 23:48-51
35 Kwan I, Bunn F Effects of prehospital spinal immobilization: a systematic review of randomized trials on healthy subjects. Prehospital Disaster Med. 2005; 20:47-53
36 March JA, Ausband SC, Brown LH Changes in physical examination caused by use of spinal immobilization. Prehosp Emerg Care. 2002; 6:421-4
37 Sahni R, Menegazzi JJ, Mosesso VN Paramedic evaluation of clinical indicators of cervical spinal injury. Prehosp Emerg Care. 1997; 1:16-8
38 Baez AA, Schiebel N Is routine spinal immobilization an effective intervention for trauma patients?. Ann Emerg Med. 2006; 47:110-1
39 Dunn TM, Dalton A, Dorfman T Are emergency medical technician-basics able to use a selective immobilization of the cervical spine protocol?: a preliminary report. Prehosp Emerg Care. 2004; 8:207-11