| Author | Affiliation |
|---|---|
| Mark A. Merlin, DO, EMT-P | Newark Beth Israel Medical Center, Barnabas Health, Newark, New Jersey |
| Alessia Carluccio, MD | Mount Sinai Medical Center, New York City, New York |
| Neil Raswant, BS | University of Medicine and Dentistry of New Jersey-School of Osteopathic Medicine, Strafford, New Jersey |
| Frank DosSantos, CDR, MC | United States Navy |
| Pamela Ohman-Strickland, PhD | University of Medicine and Dentistry of New Jersey, School of Public Health, Strafford, New Jersey |
| David P. Lehrfeld, MD, EMT-P | University of Texas, Southwestern, Dallas, Texas |
ABSTRACT
Introduction:
Loading of thiamine prior to glucose administration during hypoglycemia to prevent Wernicke’s encephalopathy is routine in the prehospital setting. To date no study has looked at the validity of this therapy.
Methods:
We evaluated a retrospective cohort of 242 patients who received intravenous glucose for hypoglycemia comparing those who received thiamine supplementation versus those who did not. Study endpoints were heart rate, blood pressure, Glasgow Coma Scale (GCS), reentry into the 911 system, and emergency department (ED) discharge rates.
Results:
There were no significant differences between the thiamine, and without-thiamine groups. All patients were discharged neurologically intact or were alert and oriented when refusing transport to the hospital. None of the 242 patients re-called 911 within the immediate 24-hour period or returned to the ED.
Conclusion:
To our knowledge this is the first study in the literature which evaluated the use of thiamine with glucose to prevent Wernicke’s encephalopathy in the prehospital setting. We found that routine administration of thiamine with glucose did not result in differences in respiratory rate, systolic blood pressure, GCS or ED hospital discharge rates. Until further research is done to validate our results emergency medical services leadership should consider whether the routine use of thiamine in the prehospital setting is appropriate for their system.
INTRODUCTION
Wernicke’s encephalopathy is a neurological condition characterized by confusion, opthalmoplegia, and cerebellar ataxia.1 It is caused by a deficiency of intracellular thiamine (vitamin B1), which is necessary for normal glucose utilization. Thiamine serves as a cofactor for pyruvate and α-ketoglutarate dehydrogenase reactions, which produce adenosine triphosphate (ATP).2 Without it intracellular energy deficits would increase, eventually leading to cell death. To prevent this, the body can store up to 30–50 mg of thiamine and requires only1–2 mg of thiamine per day to function properly.2While alcohol consumption may accelerate thiamine depletion by driving the pyruvate dehydrogenase reaction, it would take at least 4–6 weeks to exhaust the body’s natural thiamine stores by malnutrition alone.3 Acute hypoglycemic episodes occur most commonly in diabetic patients and are associated with inadequate food intake, increased physical exertion, medication interactions or sepsis. These patients would not require routine thiamine loading unless they are at risk for thiamine deficiency. The requirement that administration of thiamine should always precede the administration of glucose to prevent the precipitation of acute Wernicke’s encephalopathy is unfounded.4A Cochrane review determined insufficient evidence of the efficacy of thiamine for the treatment of Wernicke-Korsakoff syndrome, stating recommendations about the dosage and duration are acknowledged to be arbitrary. The reviewconcluded that there is insufficient evidence to guide clinicians in the dose, frequency, route, or duration of thiamine treatment for prophylaxis against or treatment of Wernicke’s due to alcohol abuse.5
Current Advanced Life Support (ALS) protocols in many states require that all acutely hypoglycemic patients receive intravenous (IV) thiamine before the administration of glucose to prevent the development of Wernicke’s encephalopathy.6 In our review of national protocols, we were able to find 24 that routinely give thiamine prior to glucose. Recommendations of thiamine loading prior to glucose administration were formulated after Watson et al. published an article in 1981 detailing four case reports of patients who developed Wernicke’s encephalopathy after glucose loading without thiamine administration.7 Each of these patients, however, had been suffering from an episode of acute hypoglycemia related to chronic malnutrition. These patients developed Wernicke’s hours after receiving glucose and all 4 had complete resolution of their neurological symptoms when thiamine was administered later in the hospitalization.8 Recent case reports of patients with Wernicke’s have shown similar results.8–10
Our state spends approximately 40,000 dollars annually on prehospital thiamine injections for routine loading in all hypoglycemic patients regardless of alcoholism or malnutrition history. The potential benefit of this cost has not been assessed in an empiric way, nor been weighed against the added risk for prehospital providers and patients due to the additional needle stick required for the thiamine. These guidelines may even be detrimental to patients in situations when glucose is delayed in order to administer thiamine. In addition, although uncommon, anaphylaxis from IV thiamine can occur, with life-threatening consequences.11,12
In this study we hypothesize that patients would have no difference in physiological parameters, including mental status, when treated with glucose alone vs. thiamine with glucose.
METHODS
The study is a retrospective cohort. It has been approved by our university’s institutional review board, which has a subcontract with our hospital. No patient consent was required by the IRB due to the de-identified nature of the data.
This study was conducted in an urban setting at a Level I trauma center. The county population of approximately 800,000 residents is made up of 68.4% Caucasian, 13.9% Asian, 13.6% Hispanic, and 9.1% African-American residents. The county occupies 323 square miles with a combination of cities and suburban communities. The emergency medical services (EMS) system is 2-tiered, comprised of a combination of paid and volunteer basic life support (BLS) units and paid hospital-based Advanced Life Support (ALS) that contain 2 paramedics per unit. Based out of our hospital, there are 8 BLS units and 6 ALS units that respond to approximately 30,000 dispatches per year, 6,500 of these being treated by ALS.
In our system, glucose is administered in the form of 50% dextrose containing 25 grams for patients over the age of21. In patients over the age of 2, 25% dextrose is given. One hundred mg of thiamine can be administered either intramuscularly or intravenously. We have glucometers on all ALS units with protocols for dextrose replacement if the glucometers indicates capillary blood glucose (CBG) is less than 70mg/dl.
As no previous studies have shown the incidence of Wernicke’s induction with glucose administration, we selected a consecutive sample of 242 patients who were treated by ALS for hypoglycemia between May 1, 2008 and August 11, 2009.
The search terms “hypoglycemia” and “IV glucose” were used in our electronic medical record (EMR) (www.emscharts.com, Atlanta, Georgia). This database was cross-referenced with the ED database, Sunrise Clinical Manager (SCM) (Eclipsys Corporations, Atlanta, Georgia) to investigate outcomes data.
All patients who were administered thiamine received 100 mg IV. Patients received glucose in the form of D50 if above 21 and D25 if above 2 years of age. No patients in our study were less than 2.
In choosing outcome measures we reviewed case reports of Wernicke’s encephalopathy for signs and symptoms that might be captured in routine EMS charting. Our review identified abnormal vital signs being induced by the carbohydrate load of glucose as an early predictor of Wernicke’s encephalopathy. These endpoints are routinely measured by prehospital care providers. Opthalomoplegia and ataxia are not documented routinely nor are they taught in our paramedic programs, but the Glasgow Coma Scale (GCS) has been shown to have high inter-rater reliability, is predictive of changes in mental status, and is routinely captured in EMS charts. GSC was our primary outcome with changes in heart rate, respiratory rate, and blood pressure as secondary outcomes. We also evaluated rates of discharge and reentry into the 911 system for patients who refused transport to the hospital. We estimated that a decrease in GCS of > 1, an increase in systolic blood pressure (SBP) > 10mmHG, and a heart rate increase by 20 to indicate a clinically significant change.
We calculated simple means and standard deviations of health indicators were calculated at each individual time point for patients administered and not administered thiamine. Means and standard deviations of percent changes in these health indicators were also calculated.
We used linear models to examine the effects of administration of thiamine (versus not) on changes in health indicators, adjusting for age and gender. Age- and gender-adjusted mean percent changes are presented along with 95% confidence intervals. We conducted sensitivity analyses excluding individuals who were administered Thiamine after D50 from the analyses described.
Because percent change in GCS was not normally distributed, we used a non-parametric analysis of variance as a sensitivity analysis. Specifically, we used a Kruskal-Wallis test to examine differences between the Thiamine and non-Thiamine groups in percent change in GCS. The significance of the effect of Thiamine derived from the Kruskal-Wallis test was similar to that reported from the linear model (data not shown).
We used the SAS software (SAS system for Windows, version 9.1.3; SAS Institute Inc, Cary, North Carolina) for all analyses.
RESULTS
During the 15-month study period 242 hypoglycemia patients were treated for hypoglycemia. Two hundred five patients (84.7%) received a loading dose of thiamine, while 37 (15.3%) did not receive the loading dose.
Means and standard deviations of pre- and post-treatment means are presented in Table. Also presented are the adjusted percent changes. There were no significant differences between the thiamine and no thiamine groups.
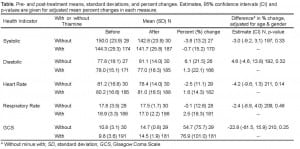
Pre- and post-treatment means, standard deviations, and percent changes. Estimates, 95% confidence intervals (CI) and p-values are given for adjusted mean percent changes in each measure.
Of the 242 patients evaluated, 180 refused transport to the hospital. They signed an “against medical advice” (AMA) form after their mental status return to baseline (as measured by GCS). Sixty-two patients (25.6%) were transported to the hospital. All of these patients were discharged neurologically intact from the ED or the hospital. None of the patients were clinically intoxicated as subjectively judged by EMS. None of the 242 patients reentered the 911 system within 24 hours or returned to the original ED.
DISCUSSION
State guidelines for thiamine administration to the hypoglycemia patients are inconsistent. Some use it in every case of hypoglycemia, others give it only to the malnourished, and a few do not give thiamine at all. Despite these state-to-state discrepancies in protocols, overall cases of dextrose-induced Wenicke’s encephalopathy are exceedingly rare. Administering it to only those patients at the highest risk for developing Wernicke’s would be the most efficacious strategy for treating hypoglycemia in the prehospital setting. Administering thiamine to only this subset of patients in the prehospital setting would reduce both costs and needle stick injuries. None of our patients who received thiamine were judged to be acutely intoxicated;however, it is possible that chronic alcoholism or other malnourished states existed.
LIMITATIONS
Our study is limited to a single institution in our specific geographic region. EMS systems in various locations could produce different results. However, we do not believe that hypoglycemia would present differently in various locations.
A limitation of this study was loss to follow up after patients were successfully relieved of their hypoglycemic symptoms. We know that none of them re-entered the 911 system, but cannot exclude that they were seen by providers outside this system. Seventy-four percent of the patients we studied refused medical attention after ALS resolved their symptoms with either thiamine and dextrose or just dextrose. However, were able to verify that none of the “refusing medical attention” group returned to our ED within 24 hours. It is possible that patients could have developed Wernicke’s after discharge from the ed. We were only able to follow-up patients returning to our ED and not surrounding hospitals.
All patients should have received thiamine under state standing orders. It is possible that those not receiving thiamine were sicker as determined by the paramedic and they subsequently did not have time to draw up the thiamine and inject it. Thiamine is under standing orders in the state. Paramedics must make contact with the base-station physician at some point during standing orders, which include dextrose and then thiamine. The paramedic can make an individual decision when to contact the base-station physician. If base station contact is made prior to administration of thiamine then it is the physician’s discretion whether to give it to the patient.
We only used the search terms “IV and glucose.” It is possible that patients were missed in our EMR secondary to improper data input. Since our system uses drop down menus, a few potential patients were lost. In addition we only searched data using IV. It is possible that some patients received oral glucose loading and resolved without IV access; however, we believe this is rare since oral glucose loading is not under state standing orders.
Lastly, we used GCS as a measure of mental status because it was available. Since the initial sign of Wernicke’s may be confusion it could cause changes in the GCS. However we acknowledge that GCS may decrease for other reasons than confusion.
In our study, hypoglycemic patients treated by ALS had the same neurological outcomes after glucose administration regardless of the inclusion of thiamine. On follow up, all 62 patients brought by ALS into our facility had complete resolution of their symptoms, 9 of whom had not received prehospital thiamine. This is because most patients receiving the thiamine with glucose regimen are suffering from a complication of diabetic treatment and are not chronically malnourished or alcoholics. These patients require immediate glucose administration; therefore, delays due to thiamine administration, or the potential for anaphylaxis from thiamine, can be detrimental to patient outcome.
Given the rarity of Wernicke’s encephalopathy, with no known determination of incidence, we likely have not studied sufficient patients to exclude this complication of dextrose administration. It remains possible that thiamine may indeed be necessary to avoid this condition. We did not specifically search for the ED diagnosis of Wernicke’s encephalopathy, instead using vital signs and GCS as surrogate diagnostic markers.
CONCLUSION
This is the first study in the literature known to us which evaluated the use of thiamine with glucose to prevent Wernicke’s syndrome in the prehospital setting. We found that routine administration of thiamine with glucose did not result in differences in respiratory rate, SBP, GCS or emergency department hospital discharge rates. Until further research is done to validate our results EMS leadership should consider whether the routine use of thiamine in the prehospital setting is appropriate for their system.
Footnotes
Supervising Section Editor: David E. Slattery, MD
Submission history: Submitted April 4, 2011; Revision received November 7, 2011; Accepted January 11, 2012
Full text available through open access at http://scholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.1.6760
Address for Correspondence: Mark A. Merlin, DO, EMT-P, Newark Beth Israel Medical Center, Barnabas Health, 201 Lyons Avenue D-11, Newark, NJ 08112
Email: mmerlin@barnabashealth.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Hemphill JC, III, Smith WS. Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. Chapter 269. Neurologic Critical Care, Including Hypoxic-Ischemic Encephalopathy and Subarachnoid Hemorrhage (Chapter) Harrison’s Principles of Internal Medicine. http://www.accessmedicine.com/content.aspx?aID=2888218. Accessed August 12, 2009.
2. Pelley JW, Goljan EF. Rapid Review Biochemistry. 2nd ed. Philadelphia, PA: Mosby; 2006. p. 55.
3. Thomson A, Marshall EJ. The Natural History and Pathophysiology of Wernicke’s Encephalopathy and Korsakoff’s Psychosis. Alcohol Alcohol. 2006;41(2):151–158.[PubMed]
4. Jack JB, Hoffman RS. Thiamine before glucose to prevent Wernicke Encephalopathy:examining the conventional wisdom. JAMA. 1998;279(8):583.[PubMed]
5. Day E, Bentham P, Callaghan R, et al. Thiamine for Wernicke-Korsakoff Syndrome in people at risk from alcohol abuse. Cochrane Database of Systematic Reviews. 2008;(2)
6. Governing Mobile Intensive Care Units New Jersey Dept of Health and Senior Services Office of Emergency Medical Services. 2002;8(41–7):18.
7. Watson AJS, Walker JF, Tomkin GH, et al. Acute Wernickes Encephalopathy Precipitated by Glucose Loading. Ir J Med Sci. 1981;150(10):301–303. [PubMed]
8. Guido ME, Brady W, DeBehnke D. Reversible Neurological Deficits in a Chronic Alcohol Abuser: A Case Report of Wernicke’s Encephalopathy. Am J Emerg Med. 1994;12:238–240. [PubMed]
9. Chotmongkol V, Limpawattana P. Wernicke’s Encephalopathy: Report of a Case. J Med Assoc Thai. 2005;88:855–858. [PubMed]
10. Ramon CG, Pereira C. Wernicke Encephalopathy: The Importance of the Diagnosis.Acta Med Port. 2006;19:442–445. [PubMed]
11. Stephen JM, Grant R, Yeh CS. Anaphylaxis from administration of intravenous thiamine. Am J Emerg Med. 1992;10:61–3. [PubMed]
12. Wrenn KD, Murphy F, Slovis CM. A toxicity study of parenteral thiamine hydrochloride. Ann Emerg Med. 1989;18:867–870. [PubMed]


