| Authors | Affiliations |
|
Samuel H.F. Lam, MD |
Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
|
Anthony Grippo, MD |
Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
|
Chistopher Kerwin, MD |
Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
|
P. John Konicki, DO |
Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
|
Diana Goodwine, MD |
Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
|
Michael J. Lambert, MD |
Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Appendicitis is a common condition presenting to the emergency department (ED). Increasingly emergency physicians (EP) are using bedside ultrasound (BUS) as an adjunct diagnostic tool. Our objective is to investigate the test characteristics of BUS for the diagnosis of appendicitis and identify components of routine ED workup and BUS associated with the presence of appendicitis.
Methods
Patients four years of age and older presenting to the ED with suspected appendicitis were eligible for enrollment. After informed consent was obtained, BUS was performed on the subjects by trained EPs who had undergone a minimum of one-hour didactic training on the use of BUS to diagnose appendicitis.They then recorded elements of clinical history, physical examination, white blood cell count (WBC) with polymophonuclear percentage (PMN), and BUS findings on a data form. We ascertained subject outcomes by a combination of medical record review and telephone follow-up.
Results
A total of 125 subjects consented for the study, and 116 had adequate image data for final analysis. Prevalence of appendicitis was 40%. Mean age of the subjects was 20.2 years, and 51% were male. BUS was 100% sensitive (95% CI 87-100%) and 32% specific (95% CI 14-57%) for detection of appendicitis, with a positive predictive value of 72% (95% CI 56-84%), and a negative predictive value of 100% (95% CI 52-100%). Assuming all non-diagnostic studies were negative would yield a sensitivity of 72% and specificity of 81%. Subjects with appendicitis had a significantly higher occurrence of anorexia, nausea, vomiting, and a higher WBC and PMN count when compared to those without appendicitis. Their BUS studies were significantly more likely to result in visualization of the appendix, appendix diameter >6mm, appendix wall thickness >2mm, periappendiceal fluid, visualization of the appendix tip, and sonographic Mcburney’s sign (p<0.05). In subjects with diagnostic BUS studies, WBC, PMN, visualization of appendix, appendix diameter >6mm, appendix wall thickness >2mm, periappendiceal fluid were found to be predictors of appendicitis on logistic regression.
Conclusion
BUS is moderately useful for appendicitis diagnosis. We also identified several components in routine ED workup and BUS that are associated with appendicitis generating hypothesis for future studies. [West J Emerg Med. 2014;15(7):-0.]
INTRODUCTION
Appendicitis is the most common acute abdominal disorder that requires surgery.1-2 The diagnosis is commonly made on the grounds of a combination of history, physical examination, laboratory tests, and diagnostic imaging findings. As these diagnostic steps often take place in a serial fashion in the emergency department (ED), patients suspected of appendicitis tend to stay for prolonged periods of time, requiring considerable staff and physical resources.3-5
To avoid excessive testing while minimizing missed diagnosis, investigators have derived various appendicitis scores based on components of history, physical examination, and laboratory test results.6-13 Typically these scores are used to rule out appendicitis, yielding a post-test population with moderate to high probability for the condition. While most of these scoring systems have high sensitivities, they cannot be used solely to select patients for surgical intervention because of inadequate specificities. Often further imaging is required to clarify the diagnosis, corresponding to a considerable time and resource burden as patients wait for its completion and interpretation. In addition, the accuracies of these scores tend to worsen when tested by unaffiliated investigators at different sites.13,14
In recent years, studies have been published on the use of beside ultrasound (BUS) to diagnose appendicitis in the ED.15-17 This is based on the radiology literature, which has shown that ultrasound is moderately to highly sensitive and specific in the diagnosis of appendicitis.18 Furthermore, BUS emits no ionizing radiation, and can be performed and interpreted rapidly at the bedside, providing obvious advantages to clinicians and patients alike.
The purpose of the study was to determine if emergency physicians (EP) can accurately diagnose appendicitis using BUS, after a brief training in graded-compression abdominal ultrasonography. We also aimed to identify components of ED history, physical examination, laboratory workup, and BUS associated with the diagnosis of appendicitis.
METHODS
This was a single-site, prospective study on patients treated at the Advocate Christ Medical Center Emergency Department for suspected appendicitis. It was approved by the Advocate Health Care Institutional Review Board. The hospital is a community tertiary referral center with approximately 100,000 ED visits per year. The ED is staffed entirely by board-certified EPs and sponsors a three-year emergency medicine residency training program. On-site staff radiologists provide interpretation of radiologic studies at all hours.
Patients four years of age and older presenting to the ED with abdominal pain concerning for appendicitis (as determined by the ED attending physician after history and physical examination) were eligible for enrollment. Exclusion criteria included previous appendectomy, pregnancy, unstable vital signs, frank peritonitis, neurological deficits interfering with the ability to localize abdominal pain, wards of the state, and subject/guardian refusal of consent. Potentially eligible subjects were identified by treating EPs, study investigators or the research nurse, by screening of the ED patient tracking board. Enrollment was by convenience sampling, depending on whether a study investigator was available. Investigators were EPs who had undergone a minimum of one-hour didactic training given by the senior investigator (ML) on the use of ultrasound to diagnose appendicitis. Topics discussed during the didactic session included the use of graded compression technique and anatomical landmarks to identify the appendix, appearance of the normal and inflamed appendix, and examples of sonographic findings associated with acute appendicitis as delineated in the data collection sheet. Study investigators were allowed to simultaneously function as treating EPs, and were not blinded to the presentation and clinical history of the subjects.
After informed consent was signed, a focused clinical history and physical examination was obtained from each study subject, followed by a focused BUS of the abdomen performed using a Zonare Z. One (Mountain View, CA) or Sonsite M-Turbo (Bothell, WA) machine. Each subject was asked to direct the investigator to the point of maximal pain. The area was then scanned with a high frequency (5-10 Mhz) transducer using graded compression technique. Investigators concluded their BUS when, in their judgment, the best possible images in the subjects were obtained. All BUS studies were completed prior to any radiology department studies or surgical consultations. Study images were recorded and archived at the ED ultrasound office, and were reviewed weekly for quality assurance. Investigators’ overall impressions of the BUS, based on real-time sonographic findings as recorded on the data collection sheet, were documented in the patients’ medical records. All patients were treated according to the judgment of the ED attending physicians or consultants.
Subject data collected included age, sex, height, weight, body mass index (BMI), time of onset of symptoms, menarche if applicable, ED treatment (pain medication, intravenous fluid, antiemetic) prior to BUS; the presence or absence of anorexia, pyrexia, nausea, vomiting, diarrhea, right lower quadrant (RLQ) pain, migration of pain to right lower quadrant from elsewhere in the abdomen, tenderness to percussion/cough/hopping, leukocyte (WBC) count, and polymorphonuclear neutrophil (PMN) percentage.
Sonographic data collected included visualization and compressibility of the appendix; diameter and wall thickness of the appendix; presence of free fluid, fecalith, or any complex mass in right lower quadrant; and sonographic McBurney’s sign (elicitation of pain when concerning structure is compressed with the ultrasound transducer).
Diagnostic test and imaging results, pathological reports, intra-operative findings, and subject hospital course, if available, were obtained by review of the medical record. A research nurse made follow-up telephone calls at 24 hours and 30 days to subjects who were discharged from the ED or who did not receive operative intervention. Three separate attempts to establish contact were made before subjects were deemed lost to follow-up. One of the investigators (SL) adjudicated final patient outcome based on the information obtained by the above-mentioned means. Diagnosis of appendicitis was based on intraoperative or pathological findings. Diagnosis of “no appendicitis” was based on intraoperative findings, presence of alternate diagnosis, resolved symptoms during inpatient observation or at follow-up telephone calls, lack of appendectomy at subsequent ED visits, or negative abdominal computed tomography results in patients who were otherwise unable to be followed up.
We recorded all study information on patient data sheets,and then entered it onto an Excel (2007, Microsoft Corp., Redmond, WA) spreadsheet for analysis. All data entries were double-checked by one of the investigators for accuracy. We analyzed data by SPSS (version 20.0, IBM Corp., Armonk, NY). Student’s t test was used for continuous variables and chi square for categorical variables. We calculated the sensitivity, specificity, positive predictive value, negative predictive value of ED BUS studies using the defined outcomes above as the gold standard. We performed univariate analysis on the recorded demographic, history, laboratory, and BUS findings to identify factors associated with appendicitis. Multivariate logistic regression was then performed incorporating significant findings in univariate analysis to determine predictive factors of appendicitis and calculate the degree of association in diagnostic BUS studies.
RESULTS
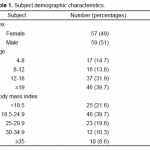
A total of 125 subjects consented for the study, and 116 had adequate image data for final analysis. Subject demographics are listed in Table 1. Mean age of the subjects was 20.2 years, and 51% were male. Sixty percent were 18 years of age or younger. Prevalence of appendicitis was 40%.
Table 1. Subject demographic characteristics.
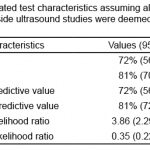
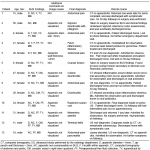
Fifty-two (45%) of the 116 BUS studies were diagnostic. There were 33 true positive, 13 false positive, 6 true negative, and no false negative BUS studies. This corresponds to a sensitivity of 100% (95% CI 87-100%), specificity of 32% (95% CI 14-57%), positive predictive value of 72% (95% CI 56-84%), and negative predictive value of 100% (95% CI 52-100%) of BUS. Alternatively calculated test characteristics assuming all non-diagnostic BUS studies were deemed negative at the bedside are listed in Table 2. Inclusion of subjects with inadequate image data did not worsen these test characteristics. Table 3 lists the BUS findings, final diagnoses, image review comments, and clinical course of subjects with false positive BUS. The majority of these 13 cases had intra-abdominal or pelvic pathology leading to the presence of peritoneal free fluid. Nine of the cases did not have the appendix clearly depicted, or depicted an appendix with a diameter <6mm as determined at the time of image review.
Table 2. Calculated test characteristics assuming all non-diagnostic bedside ultrasound studies were deemed negatives at the bedside.
Table 3. Bedside ultrasound (BUS) findings, final diagnoses, image review comments, and clinical course of false positive BUS.
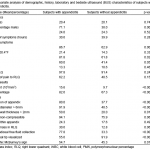
Table 4 compares the demographic, history, laboratory and BUS characteristics of subjects with and without appendicitis. There was a male predominance in subjects with appendicitis. On univariate analysis, subjects with appendicitis had a significantly higher occurrence of anorexia, nausea, vomiting, and a higher WBC count and PMN percentage. BUS of these subjects were also significantly more likely to result in visualization of the appendix, appendix diameter >6mm, appendix wall thickness >2mm, periappendiceal fluid, visualization of the appendix tip, and sonographic Mcburney’s sign (p<0.05).
Table 4. Univariate analysis of demographic, history, laboratory and bedside ultrasound (BUS) characteristics of subjects with and without appendicitis.
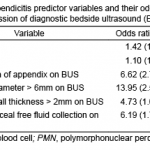
In subjects with diagnostic BUS studies, WBC, PMN, visualization of appendix, appendix diameter >6mm, appendix wall thickness >2mm, periappendiceal fluid were found to be predictors of appendicitis on multivariate logistic regression (Table 5).
Table 5. Appendicitis predictor variables and their odds ratios on logistic regression of diagnostic bedside ultrasound (BUS) studies.
BUS success and accuracy were independent of operator, parenteral narcotic or antiemetic administration, or scanning time.
DISCUSSION
Apart from individual case reports, currently there have been three published clinical trials on EP-performed BUS for the diagnosis of appendicitis. Chen et al. found that BUS had a sensitivity of 96.4% and a specificity of 67.6% for diagnosis of appendicitis, compared to 86.2% sensitivity and 37% specificity based on surgeons’ clinical judgment.15 However, prevalence of appendicitis was 75% in their study, and all physician sonographers had extensive BUS experience, reflecting a setting atypical for most EDs in the United States Fox et al. published two studies on the topic. Their first study was a retrospective registry review, which revealed that EPs without focused training on the use of BUS to diagnose appendicitis had a sensitivity of 39% and specificity of 90%.16 This was followed by a prospective study (in which all physician investigators received standardized training), which concluded that BUS was 65% sensitive and 90% specific in diagnosing appendicitis.17 This latter study was conducted in a similar setting to ours (teaching hospital, moderate appendicitis prevalence, brief training of sonographers). The major difference between our study and theirs was the diagnosis criteria for appendicitis. In the Fox study, diagnosis was based on three chosen criteria after visualization of the appendix on BUS (internal diameter > 6mm, lack of peristalsis, noncompressibility in the transverse plane), and absence of any of these findings or inability to visualize the appendix was considered a negative BUS study. In our study, diagnosis of appendicitis was based on overall beside impression of the BUS, and investigators were allowed to deem their BUS as non-diagnostic. As a result, there were only a few negatives, but many non-diagnostic BUS studies. This likely accounted for the unusually low calculated specificity in our results. Indeed, when the test characteristics were calculated assuming all non-diagnostic BUS were negative studies, the results fell within the same range as the Fox study. Additionally, as far as the authors are aware, our study was also the first to examine the association of appendicitis with specific BUS findings.
On multivariate logistic regression BUS findings, we found that appendix diameter of > 6mm was the strongest predictor of appendicitis, followed by visualization of appendix, periappendiceal free fluid collection, and appendix wall thickness > 2mm. In addition, visualization of the appendix tip on BUS and sonographic McBurney’s sign were found to be significant on univariate analysis. This is largely in concordance with the current radiology literature. Goldin et al. found that classifying studies based on findings of appendix diameter ≥7mm or appendix wall thickness >1.7mm would have accomplished 97% diagnostic accuracy in a retrospective review of pediatric ultrasound studies performed at their institution.19 This is similar to the study by Kessler et al., which found that appendix diameter ≥6mm on ultrasound had both sensitivity and specificity of 98%.20 Likewise, Je et al. determined that the optimal appendix diameter and wall thickness cutoff for diagnosis of pediatric appendicitis were 5.7mm and 2.2mm respectively.21 In another study, Van Randen et al found that thickened appendix (>6mm), transducer tenderness, and periappendiceal fat infiltration to be significant variables predicting ultrasound diagnostic accuracy.22 Pinpoint tenderness under ultrasonography was also found by Soda et al. to be 87% sensitive and 90% specific for appendicitis diagnosis.23 Both Goldin and Franke found periappendiceal fluid collection to be highly specific (99%) but insensitive (20%, 14% respectively) for appendicitis diagnosis, yielding a moderate accuracy (77%).19,24 Due to the design of most bedside ultrasound machines and abbreviated scanning time of most BUS studies, findings such as periappendiceal fat infiltration might be difficult to discern, and it is possible that some of the significant findings in BUS might be different from those derived from radiology department ultrasound studies. Hence, further studies with a larger sample size might be required to confirm our study findings.
Our BUS had a lower sensitivity and specificity than that generally reported in the radiology literature.25-27 We also had a significant number of false positive BUS studies. We speculate this might be related to the limited application-specific training and experience of our sonographers. Appendiceal sonography can be hard to master given the difficulty in visualizing the uninflamed appendix, frequent anatomical variation, common interference from the surrounding structures, and mimics from other intra-abdominal pathologies. Though all of our investigators were relatively experienced sonographers (fellow or attending credentialed in emergency ultrasound in our ED), many were new to the application at the time of the study, with limited hands-on experience beyond the one-hour didactic training. On image review by expert sonographers, many of the false positives were deemed not to have the appendix clearly depicted. If all such cases were excluded, specificity would have improved to 91%, making BUS quite useful for ruling in appendicitis. It might also be helpful to acquire dedicated pelvic BUS views in females, given the prevalence of gynecological pathology. In addition to more in-depth education and hand-on experience prior to implementation of appendix BUS protocol, we would recommend low threshold for confirmatory studies on inconclusive or difficult bedside studies based on our anecdotal experience.
Based on a combination of presenting symptoms, signs, laboratory findings, as well as radiologist-performed sonography, Tzanakis et al. developed an acute appendicitis scoring system and found it to be highly sensitive and specific in diagnosing appendicitis, with an overall accuracy of 96.5%.28 Ultrasound result carried a much heavier weight than the other components (RLQ tenderness, rebound tenderness, WBC >12,000/μL), though specific sonographic findings were not mentioned. Similarly, we also found significant associations between appendicitis and certain components of history, laboratory workup, and BUS. However, due to limited appendicitis cases and the large number of variables examined, we were unable to derive a predictive model. Future potential trials based on our results may include derivation of a “BUS appendicitis score” comprised of the above-mentioned components, possibly leading to better accuracy than BUS alone. If found to highly accurate as in Tzanakis’ case, BUS may be used as an adjunct to streamline appendicitis workup, and lead to more effective resource allocation in the ED.
LIMITATIONS
A major limitation of the study was convenience sampling of the subjects, leading to selection bias. Nevertheless, our prevalence of appendicitis and demographic characteristics were similar to other published studies on the topic, and BMI of our subjects appeared to follow a normal distribution. Investigators were also unblinded to the history and clinical examination findings of the subjects. Awareness of these findings, however, is exactly what distinguishes BUS from ultrasound performed by non-clinicians, and thuswe do not consider this a weakness of our study. Our sample size was relatively small, leading to large confidence intervals in some of our calculated test characteristics. Future large-scale studies would be necessary to confirm our findings. All investigators who performed BUS in our study were ED ultrasound fellows or faculty, with ultrasound experience exceeding that recommended by the American College of Emergency Physicians.29 Hence, our study findings may not be applicable to operators with different BUS skill levels.
CONCLUSION
Bedside ultrasound performed by emergency physicians with limited training is moderately useful for the diagnosis of appendicitis. We have identified several history, laboratory and BUS components predictive of appendicitis in our study, which might be helpful in generating hypotheses for future studies.
ACKNOWLEDGEMENTS
The authors wish to thank Kathleen Hesse, RN for her diligent followup of the study subjects, and for compilation of the study data spreadsheet. We also thank Christopher Blair, MS for providing statistical support and data analysis. We appreciate the help of Anna Kienicki-Sklar, MD and Cindy Chan, MD in recruitment of study subjects, and Karis Tekwani, MD for reviewing the study manuscript.
Footnotes
Supervising Section Editor: Laleh Gharahbaghian, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Samuel H.F. Lam, MD. Advocate Christ Medical Center, Department of Emergency Medicine, 4440 W. 95th Street, Oak Lawn, IL 60453. Email: HiuFungSamuel.Lam@AdvocateHealth.com
Submission history: Submitted February 9, 2014; Revision received June 9, 2014; Accepted September 2, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910-25.
- Bundy DG., Byerly JS, Liles EA, et al. Does this child have appendicitis? JAMA. 2007;298:438-51.
- Riesenman PJ, Riesenman KP, Stone TJ et al. Nonfocused enhanced CT evaluation of acute appendicitis increases length of stay in the emergency department but does not increase perforation rate. Am Surg. 2008;74:488-92.
- Nelson KA, Boslaugh SE, Hodge D 3d. Risk factors for extremely long length-of-stay among pediatric emergency patients. Pediatr Emerg Care. 2009;25:835-40.
- Elikashvili I, Tay ET, Tsung JW. The effect of point-of-care ultrasonography on emergency department length of stay and computed tomography utilization in children with suspected appendicitis. Acad Emerg Med. 2014;21:163-70.
- Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15:557-64.
- Ohmann C, Franke C, Yang Q. Clinical benefit of a diagnostic score for appendicitis: results of a prospective international study. Arch Surg. 1999;134:993-96.
- Enochsson L, Gudbjartsson T, Hellberg A, et al. The Fenyö-Lindberg scoring system for appendicitis increases positive predictive value in fertile women–a prospective study in 455 patients randomized to either laparoscopic or open appendectomy. Surg Endosc. 2004;18:1509-13.
- Dado G, Anania G, Baccarani U, et al. Application of a clinical score for the diagnosis of acute appendicitis in childhood: a retrospective analysis of 197 patients. J Pediatr Surg. 2000;35:1320-22.
- Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002;37:877-81.
- van den Broek WT, van der Ende ED, Bijnen AB, et al. Which children could benefit from additional diagnostic tools in case of suspected appendicitis? J Pediatr Surg. 2004;39:570-54.
- Kharbanda AB, Taylor GA, Fishman SJ, et al. A clinical decision rule to identify children at low risk for appendicitis. Pediatrics. 2005;116:709-16.
- Kharbanda AB, Dudley NC, Bajaj L, et al. Validation and refinement of a prediction rule to identify children at low risk for acute appendicitis. Arch Pediatr Adolsc Med. 2012;166:738-44.
- Ohle R, O’Reilly F, O’Brien K, et al. The Alvarado score for predicting acute appendicitis: a systemic review. BMC Med. 2011;9:139.
- Chen SC, Wang HP, Hsu HY, et al. Accuracy of ED sonography in the diagnosis of acute appendicitis. Am J Emerg Med. 2000;18:449-52.
- Fox JC, Hunt MJ, Zlidenny AM, et al. Retrospective analysis of emergency department ultrasound for acute appendicitis. Cal J Emerg Med. 2007;8:41-5.
- Fox JC, Solley M, Anderson CL, et al. Prospective evaluation of emergency physician performed bedside ultrasound to detect acute appendicitis. Eur J Emerg Med. 2008;15:80-5.
- Rosen MP, Ding A, Blake MA, et al. ACR Appropriateness Criteria® right lower quadrant pain—suspected appendicitis. J Am Coll Radiol. 2011;8:749-55.
- Goldin AB, Khanna P, Thapa M, et al. Revised criteria for appendicitis in children improve diagnostic accuracy. Pedaitr Radiol. 2011;41:993-99.
- Kessler N, Cyteval C, Gallix B, et al. Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US and laboratory findings. Radiology. 2004;230:472-78.
- Je BK, Kim SB, Lee SH, et al. Diagnostic value of maximal-outer-diameter and maximal mural-mural-thickness in use of ultrasound for acute appendicitis in children. World J Gastroenterol. 2009;15:2900-03.
- Van Randen A, Lameris W, van Es HW, et al. Profiles of US and CT imaging features with a high probability of appendicitis. Eur Radiol. 2010;20:1657-66.
- Soda K, Nemoto K, Yoshizawa S, et al. Detection of pinpoint tenderness on the appendix under ultrasonography is useful to confirm acute appendicitis. Arch Surg. 2001;136:1136-40.
- Franke C, Bohner H, Yang Q et al. Ultrasonography for diagnosis of acute appendicitis: results of a prospective multicenter trial. Acute Abdominal Pain Study Group. World J Surg. 1999;23:141-46.
- Terasawa T, Blackmore CC, Brent S, et al. Systemic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med 2004;141:537-46.
- Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006;241:83-94.
- van Randen A, Bipat S, Zwinderman AH, et al. Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology. 2008;249:97-106.
- Tzanakis NE, Efstathiou SP, Danulidis K et al. A new approach to accurate diagnosis of acute appendicitis. World J Surg. 2005;29:1151-56.
- American College of Emergency Physicians. Emergency ultrasound guidelines. Ann Emerg Med. 2009; 53: 550-70.