| Author | Affiliation |
|---|---|
| Munseok Seo, DrPH | Management, Policy and Community Health Division, University of Texas Health Science Center, Houston, Texas |
| Charles Begley, PhD | Management, Policy and Community Health Division, University of Texas Health Science Center, Houston, Texas |
| James R. Langabeer, PhD | Management, Policy and Community Health Division, University of Texas Health Science Center, Houston, Texas |
| Jami L. DelliFraine, PhD | Virginia Commonwealth University, Department of Health Administration, Richmond, Virginia |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
This study examines barriers and disparities in the intentions of American citizens, when dealing with stroke symptoms, to call 911. This study hypothesizes that low socioeconomic populations are less likely to call 911 in response to stroke recognition.
Methods
The study is a cross-sectional design analyzing data from the Centers for Disease Control’s 2009 Behavioral Risk Factor Surveillance Survey, collected through a telephone-based survey from 18 states and the District of Columbia. The study identified the 5 most evident stroke-warning symptoms based on those given by the American Stroke Association. We conducted appropriate weighting procedures to account for the complex survey design.
Results
A total of 131,988 respondents answered the following question: “If you thought someone was having a heart attack or a stroke, what is the first thing you would do?” A majority of those who said they would call 911 were insured (85.1%), had good health (84.1%), had no stroke history (97.3%), had a primary care physician (PCP) (81.4%), and had no burden of medical costs (84.9%). Those less likely to call 911 were found in the following groups: 65 years or older, men, other race, unmarried, less than or equal to high school degree, less than $25,000 family income, uninsured, no PCP, burden of medical costs, fair/poor health, previous history of strokes, or interaction between burden of medical costs and less than $50,000 family income (p<0.0001 by X2 tests). The only factors significantly associated with “would call 911” were age, sex, race/ethnicity, marital status, and previous history of strokes.
Conclusion
Barriers and disparities exist among subpopulations of different socioeconomic statuses. This study suggests that some potential stroke victims could have limited access to EMS services. Greater effort targeting certain populations is needed to motivate citizens to call 911.
INTRODUCTION
In the United States (U.S.), acute stroke is the third leading cause of death and the single largest reason for disability.1 It is a medical emergency that demands immediate emergency medical services (EMS) activation for both faster transport to definitive stroke facilities and faster initial medical treatment.2-8 Health and medical experts and professionals have long recognized the necessity of calling 911 over other contacts. Research suggests that immediate EMS activation through 911 calls benefits patients at the stroke onset because such a call is a key factor in the “stroke chain of survival.”9 This chain sequences from recognition of stroke symptoms to calling 911, from EMS dispatch to hospital, from each of the initial medical contacts such as physician examination, computed tomography (CT), neurological evaluation, diagnosis to the decision of the appropriate therapy and administration of appropriate drugs or other interventions.2-6,8,10,11 The American Stroke Association (ASA) categorizes the recommendation of calling 911 for stroke symptoms as “Class I,” based on its usefulness and effectiveness.9
However, a considerably low proportion of patients experiencing the onset of a stroke actually call 911.12,13 National registry data between 2005 and 2007 from 4 states (Georgia, Illinois, Massachusetts, and North Carolina) show that less than half (47.6%) of all stroke patients actually used EMS from the stroke’s onset.12 The data from the TLL Temple Foundation Stroke Project in rural East Texas show an even smaller proportion (38%).13
The question is, why do so many not call 911? One explanation might pertain to lack of knowledge or awareness of a stroke symptom.14-16 Several studies, however, have found that knowledge and stroke symptom awareness are only partially associated with EMS 911calls.2,17-19 This suggests that there may be factors deterring people from calling 911 at the onset of stroke symptoms.2,13-17 This study also assumes disparities in calling 911 might exist among subpopulations with different socioeconomic statuses.
This study examines barriers and disparities in U.S. citizens’ intentions to call 911 when they respond to stroke symptoms. This study, the first of its kind, hypothesizes that socio-economically vulnerable groups might be less likely to call 911, based on care-seeking behavior obstructing access to needed care.20-23
METHODS
Conceptual Model
This study’s conceptual framework is the behavioral model of healthcare utilization developed by Anderson and Aday. Their model explains how healthcare use and outcomes are affected by socio-demographic, health system, and individual factors.20,21 This model proposes 3 determinants of use: predisposing, enabling, and need. Predisposing factors (age, sex, race and ethnicity, marital status, and education) contribute to use. Enabling factors (family income, health insurance, burden of medical costs and having a primary care physician (PCP) are those that can either enhance or impede an individual’s inclination to use EMS services. Need factors (health status and symptoms) reflect whether the illness is self-perceived or evaluated by providers.
Study Design
This is a cross-sectional 1-year study based on a complex survey design.24 The survey was a monthly, state-based telephone survey carried out in 2009 and developed by the Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System (BRFSS). The complex design reflects a disproportionate, stratified sampling based on random-digit dialing sampling from listed and unlisted numbers using computer-assisted telephone interviewing systems.24
Selection of Participants
Of all non-institutionalized adults (age 18 or older) in households (N=432,607) in all 50 states of the U.S. and the 4 U.S. territories in the 2009 survey, the study’s participants (n=131,988 collected from 18 participating states and the District of Columbia) answered the following question: “If you thought someone was having a heart attack or a stroke, what is the first thing you would do?” They also answered questions about 5 stroke-warning symptoms. Respondents were asked about their knowledge of stroke symptoms, i.e., the 5 most evident stroke-warning symptoms according to the American Stroke Association (ASA).25 The questions were as follows:
- “Do you think sudden confusion or trouble speaking is a symptom of a stroke?”
- “Do you think sudden numbness or weakness of face, arm, or leg, especially on one side is a symptom of stroke?”
- “Do you think sudden trouble seeing in one or both eyes is a symptom of stroke?”
- “Do you think sudden trouble walking, dizziness, or loss of balance is a symptom of stroke?”
- “Do you think severe headache with no known cause is a symptom of stroke?”
Outcomes Measure
Answers to “If you thought someone was having a heart attack or a stroke, what is the first thing you would do?” included: “Take them to the hospital,” “Tell them to call their doctor,” “Call their spouse or a family member,” and “Do something else.” These were dichotomized as an outcome variable with “911 call” coded “1” and “no 911 call” coded “0.”
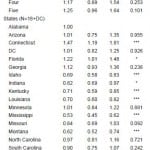
Data
In the CDC’s 2009 BRFSS dataset, 18 states and the District of Columbia (DC) participated in the optional stroke module, available only that particular year.26-28 The states included Alabama, Arizona, Connecticut, Florida, Georgia, Idaho, Indiana, Kentucky, Louisiana, Minnesota, Mississippi, Missouri, Montana, North Carolina, South Carolina, Virginia, West Virginia, and Wisconsin. These states are distributed geographically and represent more than 31% of the weighted population of the entire U.S. per the BRFSS sample. The median response rate for the 18 states and D.C. was 54.9%, ranging from 40.0% to 65.9%.29
The 2009 BRFSS data contained as predisposing factors age, sex, race/ethnicity, marital status, and education level. It contained as enabling characteristics family income, burden of medical costs, having a PCP, and health insurance status. It contained as need factors general health condition, previous history of stroke, and the number of stroke symptoms. The data also included, of course, the participating states. These variables form the basis for the study’s regression and variance analyses.
Analysis
This study employed several analytic strategies. The first was a bivariate statistical analysis to test relationships between all categorical variables using the chi-squared test. The second was a univariate logistic regression analysis to examine the size of the relationship of each factor with intent to call 911 without controlling for confounders. The third was a multivariate logistic regression to examine the factors significantly associated with intent to call 911 after controlling for confounders.
This analysis treated the answers “don’t know” and “refused” as missing values. All explanatory variables were grouped as follows:30 age group (18–44, 45–64, 65 or higher), sex (male or female), race and ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or others: Asian, native Hawaiian or other Pacific Islander, and American Indian or Alaska native), marital status (married or unmarried status that includes divorced, widowed, separated, never married, and a member of an unmarried couples), and education (≤high school, ≤2 yrs college, 4 yr college or higher), family incomes (<$25,000; $25,000 to <$50,000; $50,000 to <$75,000; $75,000 or higher), financial burden of medical care (yes or no), health insurance (yes or no), general health condition (good or better versus fair or poor), previous history of stroke (yes or no), number of stroke symptoms (one to five). In the multivariate model, this study added the state variable to adjust for geographical variation by state. The study tested the interaction between financial burden of medical care and family income (≤ or ≥$50,000). The study also dummy coded (in long format) each of the five stroke-warning symptoms that were questioned separately in the 2009 BRFSS. This was done to compare how each symptom influenced intent to call 911.
Final weights were assigned to each respondent to account for differences in the probability of their selections, non-coverage and non-response, and over-sampling of the age- and sex-specific or the race-, age-, and sex-specific population in each survey.24,26,28 For all analyses, this study used Stata statistical software version 11.1 (Stata Corp, College Station, TX) and determined the statistical significance to be at 0.05.
RESULTS
Descriptive Statistics
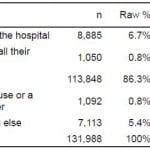
The 2009 BRFSS surveyed a total of 131,988 respondents out of 73,684,464 adult citizens (from 18 states and the District of Columbia). Respondents answered this question: “If you thought someone was having a heart attack or a stroke, what is the first thing you would do?” A majority of them (87.9% [95% CI = 87.5 to 88.2]) chose “call 911” over “take them to the hospital,” “tell them to call their doctor,” “call their spouse or a family member,” or “do something else” (Table 1).
Table 1. First response for a heart attack and a stroke. Q: If you thought someone was (sic) having a heart attack or a stroke, what is the first thing you would do?
Note: 2009 Behavioral Risk Factor Surveillance System data regarding the recognition of stroke symptoms and 911 call were collected from the following 18 states: Alabama, Arizona, Connecticut, Florida, Georgia, Idaho, Indiana, Kentucky, Louisiana, Minnesota, Mississippi, Missouri, Montana, North Carolina, South Carolina, Virginia, West Virginia, and Wisconsin.
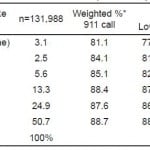
As Table 2 shows, if respondents recognized the symptom of “sudden confusion or trouble speaking,” 88.4% would call 911 (this was the symptom that generated the highest “call 911” response rate). For those who recognized not a single symptom, still 81.1% would call 911. And as Table 3 shows, if respondents recognized multiple symptoms, 88.7% would first call 911 (versus 81.1% for none). If they had to respond to any of the 5 stroke symptoms, 88.1% would first call 911.
Table 2. Proportion of the intent to call 911 per stroke symptom and the size of recognition per stroke sign in response to 911 call.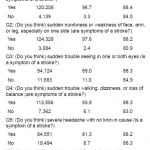
*p<0.001 by chi-squared test.
Table 3. The intent to call 911 for multiple stroke symptoms.
*p<0.0001 by chi-squared test.
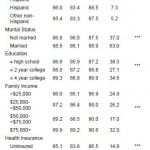
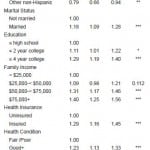
As Table 4 shows, the majority of those who would call 911 were insured (85.1%), had good health (84.1%), no stroke history (97.3%), and a PCP (81.4%); and a financial burden of medical care (84.9%). The proportion of those who would call 911 was lower in the following subgroups: those 65 years and over, men, other race, unmarried, education of a high school diploma or less, family income of less than $25,000, uninsured, no PCP, financial burden of medical care, fair/poor health, history of stroke, and interaction between financial burden of medical care and family income of less than $50,000 (p<0.0001 by X2 tests).
Table 4. Proportion of the intent to call 911 per behavioral model factors.
Odds ratio, 95% confidence interval (95% CI) and p-value were weighted estimates. P-value was calculated by chi-squared test to show the relationship between categorical variables.
*All p-values are based on Pearson chi-squared test.
***p-value<0.0001. PCP, primary care physician.
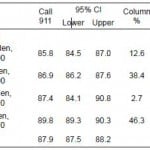
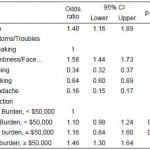
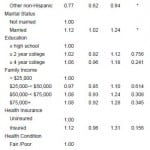
The p-value of all factors was statistically significant in X2 tests (Table 4) and the univariate model (Table 5). In the multivariate model; however, the only factors that were significant (p<0.05) were age, sex, race/ethnicity, marital status, and history of stroke. Groups that were particularly less likely to call 911 as a response to stroke symptoms were: respondents 65 years or older (OR=0.75, p<0.0001), other race (OR=0.77, p<0.05), history of stroke (OR=0.80, p<0.01), men (OR=0.74, p<0.0001) and unmarried (OR=0.89, p<0.05; Table 6).
Table 5. Findings from univariate logistic analysis.
Odds ratio, 95% confidence interval (CI) and p-value were weighted estimates. ***p-value<0.0001. **p-value<0.01. *p-value<0.05. Interaction is between medical cost burden and level of family income ($50,000). PCP, primary care physician.
Table 6. Findings from multivariate logistic analysis.
***p-value<0.0001. **p-value<0.01. *p-value<0.05. Odds ratio, 95% confidence interval (CI) and p-value were weighted estimates. Interaction effects of medical cost burden and family income on call 911 were not included because serious multicolinearity was detected. Symptoms/troubles were also not included because the variable format was not consistent with other variables’ format.
PCP, primary care physician; DC, District of Columbia
DISCUSSION
Compared to previous BRFSS studies, the 2009 data revealed considerable improvement in the number of respondents for stroke-warning symptoms, states participating, response rate, and respondents recognizing all 5 symptoms.26,28 The percentage of those that would call 911 increased by about 2%.26,28
Notably, the proportion of those who would call 911 (88.1%) seems exaggerated compared to earlier studies: in the 2004 Michigan BRFSS between 20.41% and 51.5.0% would call according to different stroke sign;18 in a 2006 survey of upstate New York, between 33% and 72% would call in response to a specific stroke symptom; and in 2006–2007 Missoula County (Montana) survey, overall 74% for a baseline, 76% for a follow up, and between 41% and 51% for a specific stroke symptom. 16,31 These studies, however, are in line with studies using a single state or small-area population survey. In fact, this study’s approximately 88% is quite consistent with previous results from multi-state BRFSS studies, e.g., 86% in 2001 (17 states and the U.S. Virgin Islands) and 86% in 2005 (13 states and DC) BRFSS.26,28
Furthermore, compared with estimates from the design-based population survey, the actual number of times 911 was called for stroke could be lower when patients are in a panic or unable to call on their own.26,28 For example, the data from the Paul Coverdell National Acute Stroke Registry (PCNASR), CDC-funded national project, reported that only 48% of patients were transported by EMS from the scene of symptom onset of a stroke.12 Similarly, the data from the Greater Cincinnati/Northern Kentucky Stroke Study (GCNKSS), a population-based epidemiology study of stroke, reported a rate of only 40.5% of EMS activation for emergency transport to the emergency department.15 As mentioned above, the finding from the TLL Project, an acute stroke surveillance and intervention project, revealed a much lower rate, only 38% of EMS 911 activation.13 More seriously, the rate of 911 EMS calls by patients themselves was a great deal lower, 4.3%,13 6%,32 and 7.1%.33
Nevertheless, this study could estimate, without selecting biased samples, the proportion of “would call 911” as intention of general population responding to recognition of stroke symptoms. That 88% would call 911 can also be partially explained by behavioral theories, such as the theory of planned behavior, which suggests that individual’s “intentions” are often quite remarkably different from their actual “behaviors.” 34 While individuals might recognize stroke symptoms and have every intention of calling 911, once the real acute event occurs, they might behave quite differently. The embarrassment or unwanted attention generated from an ambulance arriving at a patient’s house is just one reason why intent differs from actual behavior.18
Barriers and Disparities in 911 Calling
To overcome the low, real-world 911 EMS activation, experts should identify and eventually eliminate factors that discourage people from making the call and thereby benefit the chain of survival. Although several studies have done this in limited fashion, no large-scale study targeting the general population has been conducted on the comprehensive inclusion of factors that impede EMS 911 use.2,13-18
After controlling for other factors, this study found few significant factors associated with the intent to call 911 in response to recognizing stroke symptoms. However, in univariate or bivariate results from chi-squared tests, all factors showed significant association with intent to call 911.2, 13-17 That is to say, in multivariate regression results no significant relationship was discovered between the intent to call 911 and any of the financial or enabling factors, such as family income, health insurance, having a PCP or a financial burden of medical care, although they are all independent factors influencing socio-economically or financially vulnerable populations.18,21-23 Nevertheless, this study is consistent with earlier ones that found a significant association between intent to call 911 and the factors of age, sex, and race/ethnicity.2,14,16
Neither were need factors significant with the exception of “had a stroke.” This is inconsistent with one study and consistent with another, i.e., when people were reminded of a previous bad experience with physicians or hospitals.2,17 Future BRFSS surveys need to categorize “caller of 911,” which is not included in the current survey, to further investigate the insignificant association of enabling factors with intent to call 911.
This study hypothesized that individually, socio-economically, or financially vulnerable populations might encounter more barriers to calling 911 for EMS services. It found, based on results from multivariate logistic regression, that the would-be disadvantaged populations least likely to call 911 for a stroke were: seniors (65 years or older); men; non-Hispanic others (not white nor black), i.e., Asians, Native Hawaiians or other Pacific Islanders, American Indians, Alaska natives; unmarried (divorced, widowed, separated, never married, or a member of unmarried couples); and people who had already had a stroke.
LIMITATIONS
This study has several important limitations. First, between these BRFSS survey data and actual data from hospitals considerable differences existed in magnitude of intention to call 911 in response to stroke recognition. However, inconsistencies between them might be ascribed to different characteristics of samples from design-based and clinical-based study design, or different regions.2, 13-18 For example, Schroeder’s study on the clinical basis found that older individuals would more likely call 911; however, people under 60, in Schroeder’s study, accounted for only 30%, much lower than this study’s 82%.2 Incompatible with this study’s findings, Schroeder’s study found no significant association between EMS use and either race or sex; the proportion of female (55%) and white (71%) were similar to this study’s (53% and 74%). Wein’s study using other clinical patients also found no significant association between intent to call 911 and any of the following factors: age, sex, race/ethnicity, education, health insurance, and living alone. The study did find that those employed were 19% more likely to call 911.13 In contrast, other design-based survey studies similar to this one found significant associations between calling 911 and age as well as race/ethnicity.14, 16
Second, there are limitations related to the BRFSS survey itself, limitations found in other similar studies.26,28,14,16,18 For example, the following could be limitations in our study as well: under-/over-reporting of real facts due to self-reporting, underrepresentation of some populations due to not having home phones or to the proliferation of cell phone use, and generalizability to all U.S. population due to limited number of participating states.
Third, this study’s multivariate logistic model had to exclude some confounders so as to control for stroke severity scales, comorbidities, and other important clinical risk factors. These include as known risk factors diabetes, hypertension, cholesterol, and obesity14; as health behaviors, they include smoking, physical activity, and diet.14,16 They also include type of stroke and stroke severity scale or stroke symptoms.15 Despite these limitations, this study’s adjusted point and interval estimates are correct in so far as reflecting the U.S. general population’s intention to call 911 owing to the improved quality and response rate of 2009 BRFSS data along with controlling for geographical variation due to different characteristics of states, and multiple symptoms as proxy of stroke symptom severity or urgency.
CONCLUSION
The aim of this study was to examine which factors could hinder people from calling 911 in an emergency of stroke onsets; however, the study offers no answer as to why people hesitate in calling 911. Such an answer may be in the purview of qualitative research.
To improve the chain of survival, experts recommend that people experiencing stroke symptoms should call 911. Indeed, time lost is brain lost. Nevertheless, a low proportion of people, less than a half (47.6%) actually call 911. If researchers cannot identify factors that discourage patients or people from calling 911 or those populations most vulnerable, then the benefits from EMS activation may be easily eroded. Researchers must identify those subpopulations that may be individually, socio-economically, or financially disadvantaged (e.g., the elderly, men, more minor groups of minorities, and those unmarried). Effective promotion that raises awareness of the importance of calling 911 should include hospital-based patient education programs or community-based education campaigns. These would do well to target Asian populations who were not educated in the U.S. Other promotion possibilities include multi-media campaigns or any other organized effort that concerns a chain of survival or management system for acute stroke care.35
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jami L DelliFraine PhD, Management, Policy and Community Health Division, University of Texas Health Science Center, Houston, TX. Email: jami.l.dellifraine@uth.tmc.edu. 3 / 2014; 15:251 – 259
Submission history: Revision received June 16, 2013; Submitted September 9, 2013; Accepted September 9, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Mayron R, Long RS, Ruiz E. The 911 emergency telephone number: impact on emergency medical systems access in a metropolitan area. Am J Emerg Med. 1984;2(6):491-493.
2. Schroeder EB, Rosamond WD, Morris DL, et al. Determinants of use of emergency medical services in a population with stroke symptoms: the Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000;31:2591-2596.
3. Morris DL, Rosamond W, Madden K, et al. Pre-hospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke. 2000;31:2585-2590.
4. Curran C, Henry C, O’Connor KA, et al. Predictors of early arrival at the emergency department in acute ischaemic stroke. Ir J Med Sci. 2011;180(2):401-405.
5. Williams LS, Bruno A, Rouch D, et al. Stroke patients’ knowledge of stroke. Influence on time to presentation. Stroke. 1997;28:912-915.
6. Morris DL, Rosamond WD, Hinn AR, et al. Time delays in accessing stroke care in the emergency department. Acad Emerg Med. 1999;6:218-223.
7. Lacy CR, Suh DC, Bueno M, et al. Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (S.T.R.O.K.E.). Stroke. 2001;32:63- 69.
8. Rossnagel K, Jungehulsing GJ, Nolte CH, et al. Out-of-hospital delays in patients with acute stroke. Ann Emerg Med. 2004;44:476-483.
9. Adams HP, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atheros. Circulation. 2007;115(20):e478-534.
10. California Acute Stroke Pilot Registry (CASPR) Investigators. Prioritizing interventions to improve rates of thrombolysis for ischemic stroke. Neurology. 2005;64(4):654–659.
11. Deng YZ, Reeves MJ, Jacobs BS, et al. IV tissue plasminogen activator use in acute stroke: experience from a statewide registry. Neurology. 2006;66:306-312.
12. George MG, Tong X, McGruder H, et al. Paul Coverdell National Acute Stroke Registry Surveillance – four states, 2005–2007. MMWR Surveill Summ. 2009;58(7):1-23.
13. Wein TH, Staub L, Felberg R, et al. Activation of emergency medical services for acute stroke in a nonurban population: the T.L.L. Temple Foundation Stroke Project. Stroke. 2000;31:1925-1928.
14. DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among U.S. Hispanics. Am J Prev Med. 2006;30(3):189-196.
15. Kleindorfer D, Lindsell CJ, Moomaw CJ, et al. Which stroke symptoms prompt a 911 call? A population-based study. Am J Emerg Med. 2010;28(5):607-612.
16. Jurkowski JM, Maniccia DM, Dennison BA, et al. Awareness of necessity to call 911 for stroke symptoms, upstate New York. Prev Chronic Dis. 2008;5(2):A41.
17. Mosley I, Nicol M, Donnan G, et al. Stroke symptoms and the decision to call for an ambulance. Stroke. 2007;38(2):361-366.
18. Fussman C, Rafferty AP, Lyon-Callo S, et al. Lack of association between stroke symptom knowledge and intent to call 911: a population-based survey. Stroke. 2010;41(7):1501-1507.
19. Ritter MA, Brach S, Rogalewski A, et al. Discrepancy between theoretical knowledge and real action in acute stroke: self-assessment as an important predictor of time to admission. Neurol Res. 2007;29(5):476-479.
20. Andersen R, Aday LA. Access to medical care in the U.S.: realized and potential. Med Care. 1978;16(7):533-546.
21. Aday LA. Economic and noneconomic barriers to the use of needed medical services. Med Care. 1975;13(6):447-456.
22. Shi L, Stevens GD. Vulnerability and unmet health care needs. The influence of multiple risk factors. J Gen Intern Med. 2005;20(2):148-154.
23. Shi L, Stevens GD, Lebrun LA. Enhancing the measurement of health disparities for vulnerable populations. J Public Health Manag Pract. 2008;14(Suppl):S45-52.
24. CDC BRFSS. 2009. Available at: http://www.cdc.gov/brfss/technical_infodata/surveydata/2009.htm Accessed December 24, 2010.
25. American Stroke Association. Learn to Recognize a Stroke. Available at: www.strokeassociation.org. Accessed December 28, 2010.
26. Centers for Disease Control and Prevention (CDC). Awareness of stroke warning signs–17 states and the U.S. Virgin Islands, 2001. MMWR Morb Mortal Wkly Rep. 2004;53(17):359-362.
27. Lutfiyya MN, Bardales R, Bales R, et al. Awareness of heart attack and stroke symptoms among Hispanic male adults living in the United States. J Immigr Minor Health. 2010;12(5):761-768.
28. Centers for Disease Control and Prevention (CDC).Awareness of stroke warning signs–13 states and the District of Columbia, 2005. MMWR Morb Mortal Wkly Rep. 2008;57(18):481-485.
29. CDC BRFSS 2009 Summary Data Quality Reports. Available at: http://www.cdc.gov/brfss/technical_infodata/quality.htm Accessed June 2010.
30. Begley CE, Behan P, Seo m. Who uses hospital emergency rooms?: evidence from Houston/Harris County Texas. J Health Care Poor Underserved. 2010;21(2):606-616.
31. Fogle CC, Oser CS, Troutman TP, et al. Public education strategies to increase awareness of stroke warning signs and the need to call 911. J Public Health Manag Pract. 2008;14(3):e17-22.
32. Rosamond W, Evenson K, Schroder E, et al. Calling emergency medical services for stroke: A study of 911 tapes. Prehospital Emergency Care. 2005;9:19-23.
33. Handschu R, Poppe R, Rauss J, et al. Emergency calls in acute stroke. Stroke. 2003;34:1005-1009.
34. Ajzen I. The theory of planned behavior. Org Behav Hum Decis Process. 1991;50:179-211.
35. Tadros A, Crocco T, Davis SM, et al. Emergency medical services-based community stroke education: pilot results from a novel approach. Stroke. 2009;40(6):2134-2142.
36. Jurkowski JM, Maniccia DM, Spicer DA, et al. Impact of a multimedia campaign to increase intention to call 911 for stroke symptoms, upstate New York, 2006–2007. Prev Chronic Dis. 2010;7(2):A35.