| Authors | Affiliation |
| Teresita M. Hogan, MD | University of Chicago, Section of Emergency Medicine, Chicago, IllinoisPresence Resurrection Medical Center, Department of Emergency Medicine, Chicago, Illinois |
| Bhakti Hansoti, MD | University of Chicago, Section of Emergency Medicine, Chicago, IllinoisJohns Hopkins University, Department of Emergency Medicine, Baltimore, Maryland |
| Shu B. Chan, MD, MSc | Presence Resurrection Medical Center, Department of Emergency Medicine, Chicago, Illinois |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Emergency care of older adults requires specialized knowledge of their unique physiology, atypical presentations, and care transitions. Older adults often require distinctive assessment, treatment and disposition. Emergency medicine (EM) residents should develop expertise and efficiency in geriatric care. Older adults represent over 25% of most emergency department (ED) volumes. Yet many EM residencies lack curricula or assessment tools for competent geriatric care. Fully educating residents in emergency geriatric care can demand large amounts of limited conference time. The Geriatric Emergency Medicine Competencies (GEMC) are high-impact geriatric topics developed to help residencies efficiently and effectively meet this training demand. This study examines if a 2-hour didactic intervention can significantly improve resident knowledge in 7 key domains as identified by the GEMC across multiple programs.
Methods
A validated 29-question didactic test was administered at six EM residencies before and after a GEMC-focused lecture delivered in summer and fall of 2009. We analyzed scores as individual questions and in defined topic domains using a paired student t test.
Results
A total of 301 exams were administered; 86 to PGY1, 88 to PGY2, 86 to PGY3, and 41 to PGY4 residents. The testing of didactic knowledge before and after the GEMC educational intervention had high internal reliability (87.9%). The intervention significantly improved scores in all 7 GEMC domains (improvement 13.5% to 34.6%; p<0.001). For all questions, the improvement was 23% (37.8% pre, 60.8% post; P<0.001) Graded increase in geriatric knowledge occurred by PGY year with the greatest improvement post intervention seen at the PGY 3 level (PGY1 19.1% versus PGY3 27.1%).
Conclusion
A brief GEMC intervention had a significant impact on EM resident knowledge of critical geriatric topics. Lectures based on the GEMC can be a high-yield tool to enhance resident knowledge of geriatric emergency care. Formal GEMC curriculum should be considered in training EM residents for the demands of an aging population.
INTRODUCTION
The field of emergency medicine (EM) is constantly generating new knowledge, and a rapidly shifting world presents ever additional demands on emergency care. This creates a drive to cram more breadth and depth of topics into a crowded residency conference schedule. The EM management of older adults is the perfect example of this pressure. Emergency older adult care is more time-consuming, difficult, and resource intensive than the care of younger adults.1 Emergency physicians believe insufficient time is spent on geriatric issues in EM residency training.2
A large volume of geriatric-specific knowledge essential to emergency care exists. Additionally because aging increases both risk of disease and overall mortality, physicians should generally treat the elderly more aggressively than younger patients.3 Still, multiple studies show age-related treatment bias with rates of life-saving therapies lower in older patients.4-7
In response to the imperatives above, specific geriatric curricula for EM residency training have been developed.8-11 Some programs have created fellowship training in the new subspecialty of geriatric EM.12,13 Emergency departments (ED) nationwide are developing geriatric EDs or geriatric treatment areas.14-16 These have improved healthcare delivery to older adults with fewer adverse drug reactions, higher patient satisfaction and decreased hospital admission rates.17
However, the adoption of geriatric curricula is left to the discretion of individual programs. Time constraints and multiple demands to teach new technologies and topics hinder the insertion of geriatric curricula into overcrowded lecture schedules. The American College of Emergency Physicians (ACEP) has called for members to “prioritize and provide support for the development of an enhanced geriatric core curriculum for resident training.”18 However, despite national efforts by groups such ACEP, as well as the American Geriatrics Society, the John Hartford Foundation, and the American Medical Association, the lone geriatric-specific training requirement by the RRC-EM in 2012 addresses only the very limited topic of elder abuse.19
Educators question how we can optimize geriatric training in limited time. We know learning experiences based on objective practice-needs assessment or knowledge testing alter aspects of physician performance.20,21 Similar to the principal core competencies of the ACGME, the Geriatric Emergency Medicine Competencies (GEMC)8 are the core competencies of geriatric emergency care. Core competencies address the imperative to fit pivotal components into full residency curricula. The GEMC was developed to focus on high-yield pivotal content areas most substantive to practice. The purpose of this study was to see if a 2-hour educational intervention based on the GEMC could significantly improve didactic knowledge in the core domains representing the spectrum of geriatric emergency care.
METHODS
The GEMC are high impact geriatric topics developed by Hogan et al and identified through expert consensus as most important in the emergency care of older adults.22,23 The GEMCs were used as a basis for development of an educational intervention, and multiple choice assessment tool. The intervention consisted of a 1-hour didactic lecture delineating the clinical relevance of the 7 GEMC domains. This was followed by a 1-hour workshop using 4 geriatric cases, each based on 2 domain topics presented in small group discussion format. The assessment tool was a multiple-choice test also based on the GEMC.24
The test was developed by an expert panel consisting of 8 emergency physicians from 5 institutions, and led by a National Board of Medical Examiners (NBME) item writer trainer. All members were trained in NBME item writing and were focused in geriatric EM resident teaching. This panel created 42 questions covering 7 key domains of geriatric knowledge. The test was piloted and validated on a sample of 48 graduating EM residents from 3 separate programs. Starting with 42 items and using an iterative process with Cronbach’s Alpha as the measure of internal validity, individual question items were removed until an optimal balance of questions and validity remained in each of the 7 domains.
Then this validated 29-question didactic test was administered at 6 EM residencies. IRB approval was obtained at all 6 programs. Individual resident participation was voluntary, and consent was obtained as the first step in test administration. The 6 EM residencies varied by geographic location, clinical settings, educational curricula and numbers of years in existence. The same test was administered via email one week before and the week after the above educational intervention in the summer and fall of 2009. A single educator delivered the educational intervention at all sites and directed the small group format delivered by the educator and 3 members of volunteer faculty from each program. The educator is an EM-trained former EM program director, who completed the Brookdale Leadership in Aging Fellowship. We analyzed test scores as individual questions and in the 7 defined topic domains using a paired student t test. Overall internal reliability of the didactic test was measured using Cronbach’s Alpha. We determined that a sample size of 300 exams had 80% power to find at least 15% difference before and after the educational intervention.
RESULTS
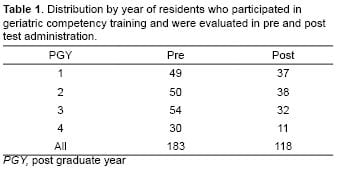
A total of 301 exams were administered, as illustrated in Table 1. There was equal distribution by postgraduate year (PGY). A total of 29 questions were asked. The testing of didactic knowledge before and after the GEMC educational intervention had high internal reliability (87.9%). The results indicate that the test is indeed reflective of EM resident knowledge in this area.
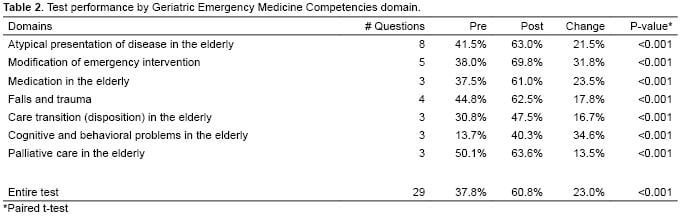
For analysis questions were grouped into 7 individual domains as shown in Table 2.
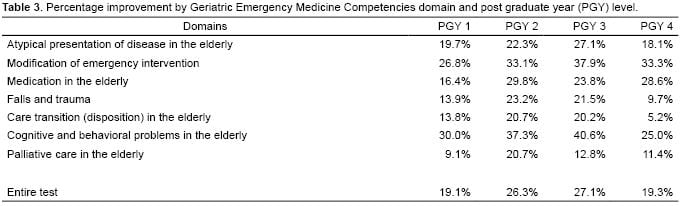
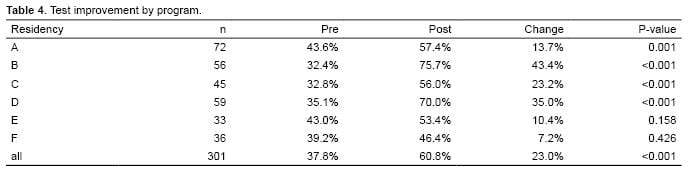
The educational intervention using the geriatric competencies for EM residents significantly improved test scores in all domains at every resident training level, as shown in Table 3. Graded increase in geriatric knowledge occurred by PGY year with the greatest improvement seen at the PGY 3 Level. All of the 6 programs showed improvement in test scores after the brief education intervention. Four of the six residencies had a significant improvement as shown in Table 4.
DISCUSSION
This study highlights that a 2-hour educational intervention based on the GEMC had a significant impact on resident knowledge of geriatric emergencies. These findings are consistent with those of Beise at al,22 demonstrating that a geriatric curriculum improved knowledge among the 25 residents. However, the Beise curriculum required more time and used a non-validated 35-question author- designed multiple-choice test, at a single institution. Our study used an exam with pilot testing and internal validation, in content specific areas, and demonstrated positive impact on resident knowledge at all PGY levels and across multiple institutions.
In the teaching of EM, myriad topics vie for time in overcrowded conference schedules. For this reason, the GEMC were designed to be a high-impact series of topics important to the practice of EM to create maximal educational impact in minimal time. Our findings support that a 2-hour didactic and case-based session when focused on proven GEMC topics result in significant improvement of resident test performance.
The concept of curricula tailored to teach broad topics in a short time through concentration on high- impact areas has not been extensively studied. The GEMC were developed through expert consensus. The goal was to identify areas most relevant to EM practice and design a sharply focused curriculum with maximum ability to enhance knowledge in this topic.
The success of this intervention spanned PGY level. Residents at all levels showed significant improvements in their knowledge. Interestingly, our study found that the percentage improvement increased by PGY year, with the highest improvement in PGY 3 participants. We had anticipated that the greatest improvement would in PGY 1 residents with the least knowledge and the most to gain from every educational exposure. This finding demonstrates that focused didactics are important irrespective of residency level. Perhaps those with greatest levels of knowledge are best able to capitalize and assimilate more intensive and rapid-fire concepts, as were delivered in our intervention.
Additionally this educational intervention improved scores across varied programs, each with diverse geriatric learning opportunities. Thus it can be hypothesized that the strength of our positive results across varied programs may be a product of this specific curriculum. This curriculum could possibly be used across multiple sites with expectation of improving resident knowledge.
The Model of the Clinical Practice of Emergency Medicine23 (EM Model) serves as the basis for the content specifications for all American Board of Emergency Medicine (ABEM) examinations.24 The knowledge required to practice competent EM increases daily. Perhaps the EM Model could adapt the GEMC high-impact focus based on expert consensus, to other topic areas with the goal of improving knowledge delivery and maximizing teaching time while enhancing didactic mastery of other EM core topics.
As a result of the demographic imperative of elders in our EDs, and the known failures of EM to provide elders with optimal care, time for geriatric specific teaching must be made. The GEMC were designed to provide optimal high-yield focus for the teaching of geriatric emergency care. The GEMC curricula can be used to maximize EM knowledge of geriatric emergency care in minimal time.
LIMITATIONS
The geriatric education product used in this study is one of many products available to EM resident education. The programs involved in this study all have faculty sympathetic to the teaching of geriatric topics. This may skew resident learning positively toward geriatric care.
Although a single educator presented the didactic lecture and directed the small group sessions, faculty from each site administered individual cases. Although they were provided identical clearly written oral boards-style cases, common stimuli, and scripted discussion points, variable teaching points inevitably occurred. Group specific variation in teaching, learning and test scores could have occurred as a result.
Tests were administered electronically, and delivered to resident emails the week prior to and the week following the conference attendance. A linked survey tool was used so that each resident could only respond once. Only residents that completed the pretest and then attended the educational session were able to complete the post test. This accounts for the attrition of residents from pre to post intervention.
There are many other confounding factors that contribute to gain in medical knowledge. Beyond lectured didactic sessions, residents can improve upon their knowledge base through reading assignments, journal club, clinical lessons and practice-based improvement. The multi-site nature of this study and short time frame between pre and post testing is intended to minimize the effect of these confounding forces.
CONCLUSION
A brief geriatric EM competency-based intervention had a significant impact on EM resident knowledge of critical geriatric topics. Lectures based on the GEMC can be a high yield tool to enhance resident knowledge of geriatric emergency care. A formal GEMC curriculum should be considered in training EM residents for the demands of an ageing population.
ACKNOWLEDGEMENTS
Footnotes
If interested in using the tool, please contact corresponding authors. The survey has not been published here because it is still being used as an education tool.
Supervising Section Editor: David T. Williams, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Teresita M. Hogan, MD. Department of Emergency Medicine, The University of Chicago, 5841 S. Maryland Ave., MC 5068, Chicago, IL 60637. Email: thogan@medicine.bsd.uchicago.edu.
Submission history: Submitted July 9, 2013; Revision received January 17, 2014; Accepted February 3, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Sanders A. Care of the Elderly in the Emergency Department Conclusions and Recommendations. Ann Emerg Med. 1992;21:830-834.
- Wilber S, Gerson L. A Research Agenda for Geriatric Emergency Medicine. Acad Emerg Med. 2003;10:3.
- Alter DA, Manuel DG, Gunraj N, et al. Age, Risk-Benefit Trade-offs, and the Projected Effects of Evidence-Based Therapies. Am J Med. 2004;116:541-545.
- Krumholz HM, Radford MJ, Wang Y. Early beta-blocker therapy for acute myocardial infarction in elderly patients. Ann Intern Med. 1999;131:648–654.
- Rochon PA, Anderson GM, Tu JV, et al. Use of beta-blocker therapy in older patients after acute myocardial infarction in Ontario. CMAJ.1999;161(11):1403–1408.
- Rathore SS, Mehta RH, Wang Y, et al. Effects of age on the quality of care provided to older patients with acute myocardial infarction. Am J Med. 2003;114:307–315.
- McAlister FA, Taylor L, Teo KK, et al. The treatment and prevention of coronary heart disease in Canada: do older patients receive efficacious therapies? The Clinical Quality Improvement Network (CQIN) Investigators. J Am Geriatr Soc. 1999;47:811–818.
- Hogan T, Losman E, Carpenter CR, et al. Development of Geriatric Competencies for Emergency Medicine Residents Using an Expert Consensus Process. Acad Emerg Med. 2010;17(3):316-324.
- Prendergast HM, Jurivich D, Edison M, et al. Preparing the front line for the increase in the aging population: geriatric curriculum development for an emergency medicine residency program. J Emerg Med. 2010;38(3):386-392.
- Biese KJ, Roberts E, LaMantia M, et al. Effect of a geriatric curriculum on emergency medicine resident attitudes, knowledge, and decision-making. Acad Emerg Med. 2011;8(2):92-96.
- Wadman MC, Lyons WL, Hoffman LH, et al. Assessment of a chief complaint-based curriculum for resident education in geriatric emergency medicine. West J Emerg Med. 2012;12(4):484-488.
- Flomenbaum NE, Elder ER. First geriatric emergency medicine fellowship launched. Modern Healthcare 2005;25:58.
- Department of Emergency Medicine at SUNY Downstate / Kings County Hospital Center Sub-Division of Geriatric Emergency Medicine. Available at: http://www.downstate.edu/emergency_medicine/geriatrics.html. Last accessed July 9th 2013.
- Maaravi Y, Stessman J. The geriatric emergency department. J Am Geriatr Soc. 2008;56(8):1579.
- Thomas K. Emergency department: Emergency departments for seniors tackle future challenges of geriatric care. Hosp Health Netw. 2011;85(1):13.
- Hwang U, Morrison RS. The geriatric emergency department. J Am Geriatr Soc. 2007;55(11):1873-1876.
- George C. Seniors emergency departments” yield health improvements, advocates say. CMAJ. 2011;183(10):613-614.
- Fitzgerald RT. Report on: The Future of Geriatric Care in our Nation’s Emergency Departments: Impact and Implications. ACEP, October, 2008.
- Accreditation Council for Graduate Medical Education. Residency review committee’s common program requirements. Available at: http://www.acgme.org Last accessed 6th February 2012.
- Jennett PA, Laxdal OE, Hayton RC, et al. The effects of continuing medical education on family doctor performance in office practice: a randomized control study. Med Educ. 1988;22:139-145.
- White CW, Albanese MA, Brown DD, et al. The effectiveness of continuing medical education in changing the behaviour of physicians caring for patients with acute myocardial infarction. Ann Intern Med. 1985;102:689-692.
- Biese K, Roberts E, LaMantia M, et al. Effect of a Geriatric Curriculum on Emergency Medicine Resident Attitudes, Knowledge, and Decision-Making. Acad Emerg Med. 2011;18 Suppl 2:S92-96.
- 2011 EM Model Review Task Force, Perina DG, Brunett CP, et al. The 2011 model of the clinical practice of emergency medicine. Acad Emerg Med. 2012;19(7):19-40.
- American Board of Emergency Medicine (ABEM): EM Model. Available at: http://www.abem.org Last accessed 10th February 2012.