| Author | Affiliation |
|---|---|
| Angela M. Mills, MD | University of Pennsylvania, Department of Emergency Medicine, Philadelphia, PA |
| J. Matthew Edwards, MD | University of Pennsylvania, Department of Emergency Medicine, Philadelphia, PA |
| Frances S. Shofer, PhD | University of North Carolina, Department of Emergency Medicine, Chapel Hill, NC |
| Daniel N. Holena, MD | University of Pennsylvania, Department of Surgery, Division of Traumatology and Surgical Critical Care, Philadelphia, PA |
| Stephanie B. Abbuhl, MD | University of Pennsylvania, Department of Emergency Medicine, Philadelphia, PA |
ABSTRACT
Introduction:
To determine the association between age and analgesia for emergency department (ED) patients with abdominal or back pain.
Methods:
Using a fully electronic medical record, we performed a retrospective cohort study of adults presenting with abdominal or back pain to two urban EDs. To assess differences in analgesia administration and time to analgesia between age groups, we used chi-square and Kruskal-Wallis test respectively. To adjust for potential confounders, we used a generalized linear model with log link and Gaussian error.
Results:
Of 24,752 subjects (mean age 42 years, 65% female, 69% black, mean triage pain score 7.5), the majority (76%) had abdominal pain and 61% received analgesia. The ≥80 years group (n=722; 3%), compared to the 65–79 years group (n=2,080; 8%) and to the <65 years group (n=21,950; 89%), was more often female (71 vs. 61 vs. 65%), black (72 vs. 65 vs. 69%), and had a lower mean pain score (6.6 vs. 7.1 vs. 7.6). Both older groups were less likely to receive any analgesia (48 vs. 59 vs. 62%, p<0.0001) and the oldest group less likely to receive opiates (35 vs. 47 vs. 44%, p<0.0001). Of those who received analgesia, both older groups waited longer for their medication (123 vs. 113 vs. 94 minutes; p<0.0001). After controlling for potential confounders, patients ≥80 years were 17% less likely than the <65 years group to receive analgesia (95% CI 14–20%).
Conclusion:
Older adults who present to the ED for abdominal or back pain are less likely to receive analgesia and wait significantly longer for pain medication compared to younger adults.
INTRODUCTION
Acute pain is one of the most common reasons for presenting to an emergency department (ED).1Oligoanalgesia, or the undertreatment of pain, has been studied in the emergency setting and is well documented in the emergency medicine (EM) literature.2–4 Disparities in pain management have been attributed to a variety of patient factors, including gender, race, insurance status and extremes of age.5–14 Pain management has been identified as a specific issue for quality-of-care improvement in older adults.15,16 In emergency care, quality indicators that include effective analgesia have been developed for pain management in older adults as they are less likely to receive analgesia than younger adults with similar conditions.17 A study of 231 ED patients with isolated long-bone fractures showed that older adults were less likely to receive analgesia when compared with younger adults with similar injuries. Additionally, those older adults who received analgesia waited longer for their medication and were less likely to receive an opioid analgesic.12
Oligoanalgesia in older adults may be related to both provider and systems factors. In a survey of emergency physicians, almost half of providers reported discomfort with their degree of training in geriatric EM and in the practice of prescribing analgesia to older adults.18 Recently, an expert consensus process has identified geriatric pain management as a minimal core competency for EM residents.19 Factors affecting the ED as a whole may also contribute to oligoanalgesia; Hwang et al.20found that increased crowding in the ED led to underassessment and undertreatment of pain, delays in analgesia and treatment with inappropriate pain medications in older ED patients with hip fractures.
In 2006 adults age 65 and older accounted for over 17.3 million ED visits, or approximately 15% of all visits.1 However, based on predicted demographic changes, older patients will increase to as much as one-third of all ED visits in the next 30 years.21, 22 Older adults use emergency services at much higher rates and have longer stays in the ED than younger adults.23 Older adults are also a vulnerable population in the emergency care setting,24 with data demonstrating inferior quality of care leading to poor clinical outcomes.25–29 Specifically, oligoanalgesia in older patients may also lead to negative consequences such as delirium, depression, and increased hospital length of stay.30–32
Abdominal pain and back pain are two of the most common specific reasons for seeking emergency care, with abdominal pain as the leading reason to visit the ED accounting for eight million visits annually.1 While historically the early use of analgesia in ED patients with abdominal pain was thought to mask signs of peritonitis and potentially delay care, multiple well-designed randomized controlled trials have conclusively shown that this practice does not lead to adverse outcomes.33–41 The Joint Commission’s 2001 pain management standards state that every patient has a right to have his or her pain assessed and treated.42 Therefore, the timely use of analgesia in patients who have been assessed appropriately and request symptom control should be a standard of care in EM practice. Analgesics, specifically opiate analgesics, have been shown to be safe for older adults when understood and used correctly.43–45 To our knowledge, there have been no large studies examining the effect of age on the administration of analgesia for acute pain in an emergency setting. We sought to study the affect of age on a large cohort of more than 24,000 patients presenting to the ED with abdominal or back pain. We hypothesized that older adults would be less likely to receive analgesia for the treatment of these complaints.
METHODS
Study Design and Setting
We performed a retrospective cohort study of adult ED patients who presented with a chief complaint of abdominal pain or back pain. The study was performed at the Hospital of the University of Pennsylvania (HUP) and Presbyterian Medical Center (PMC), two urban EDs with 57,000 and 35,000 annual visits respectively. The Institutional Committee on Research Involving Human Subjects at the University of Pennsylvania approved the study.
Selection of Participants
We identified patients using an electronic medical record search of EMTRAC (University of Pennsylvania, Philadelphia, PA), a comprehensive computerized charting system. We included all adult ED patients, 18 and older, who presented between July 2003 and February 2007 to triage with a chief complaint of abdominal pain or back pain. Specific chief complaint variants of abdominal pain (e.g., gastroesophageal reflux disease, urinary tract infection, etc) or back pain complaints (e.g., sciatica, muscle spasm, etc) were not included. Patients were excluded who left the ED without being seen, who were pregnant, or who had no documented pain score or a pain score of “0.” Patients were categorized into one of three groups: adults ≥80 years of age, adults between the ages of 65 and 79, and adults <65 years of age.
Methods of Measurement
We created a database from EMTRAC, a fully electronic emergency medical record, where each entry, order, or activity is automatically time-stamped for pre–specified ED events (e.g., when a patient is first seen by a nurse in triage; is placed in an ED room; orders are entered by a physician; completion of medication orders by a nurse). The database included patient demographics (age, sex, race), triage classification (4-point scale [1–4] from emergent [1] to nonemergent [4]), triage pain score, pain medication type and time of administration and final ED disposition. Triage pain scores were documented using an 11-point scale (0–10), from “no pain” (0) to “worst pain of my life” (10). For this study we excluded patients with a pain score of “0.” Reassessments for pain were not available for this analysis. We obtained the type and time of the first analgesic administration directly from the electronic medical record. We defined time to analgesia as time from patient placement in the treatment area (ED room or hallway) to time of analgesia administration, as documented in the electronic record. Analgesics were defined as any pain medication administered in the ED including “to go” medications, which almost always consisted of four tablets of acetaminophen with oxycodone handed to patients about the time of discharge. We defined opiate analgesia as any oral, intramuscular or intravenous medication administered in the ED as documented in the electronic record (e.g., acetaminophen with oxycodone, acetaminophen with codeine, morphine, hydromorphone). Non-opiate analgesia included any oral, intramuscular or intravenous non-narcotic medication (e.g., acetaminophen, ibuprofen, ketorolac). The main outcome measures were analgesic administration and time to analgesic treatment.
Data Analysis
Descriptive data are presented as means with standard deviations (SD) for continuous data, medians with interquartile ranges (IQR) for time variables, and frequencies and percents for categorical data. Patients were divided into three groups: age ≥80, age 65–79, and age <65. To assess differences in analgesia administration between age groups, we used the Fisher’s exact test. We used the Kruskal-Wallis test to assess differences in time to analgesic administration between the groups. Times from room placement to analgesia are presented as medians with interquartile ranges (IQR). Potential confounding variables include gender, race, triage classification, severe pain, disposition status and presenting complaint of abdominal or back pain. We defined severe pain as a pain score of eight to ten. We determined this list of confounders a priori, and there were no stepwise techniques used to select variables. To calculate the likelihood of receiving analgesia or an opiate, while adjusting for the above confounders and clustering on physician, we used a generalized linear model with a log link, Gaussian error, and robust estimates of the standard errors of the model coefficients.46 Data for these analyses are presented as relative risks (RR) with 95% confidence intervals (CI). We performed the generalized linear models using Stata statistical software (Version 11, Stata Corporation, College Station, TX). All other analyses were performed using SAS statistical software (Version 9.2, SAS Institute, Cary, NC). A probability of <0.05 was considered statistically significant.
RESULTS
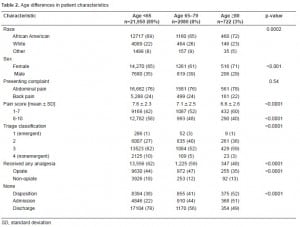
We identified 24,752 patients with abdominal pain or back pain during the study period. See Table 1for general patient characteristics. Overall, the group was young (mean age 42), more often female (65%) and black (69%), with a majority of patients presenting with abdominal pain (76%). The mean triage pain score for the group was 7.5. Overall, 15,128 patients (61%) received any analgesia, and 10,857 (44%) received an opiate analgesic.

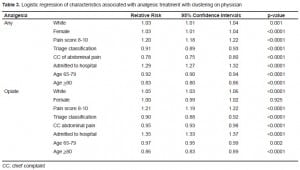
The ≥80 years group (N=722; 3%), compared to the 65–79 years group (N=2,080; 8%) and to the <65 years group (N=21,950; 89%), was more often female (71 vs. 61 vs. 65%), black (72 vs. 65 vs. 69%), and had a lower mean pain score (6.6 vs. 7.1 vs. 7.6). Table 2 describes the age differences in patient characteristics. Both older groups were less likely to receive any analgesia (48 vs. 59 vs. 62%, p<0.0001), and the ≥80 years group less likely to receive opiates (35 vs. 47 vs. 44%, p<0.0001). Of those patients who received analgesia, both older groups waited significantly longer for their medication (median time 123 vs. 113 vs. 94 minutes; p<0.0001). After controlling for gender, race, triage classification, severe pain, disposition status, and presenting complaint, patients 65–79 were 8% less likely (95% CI: 6–10%) and patients ≥80 years were 17% less likely (95% CI: 14–20%) than the <65 years group to receive analgesia (Table 3).
DISCUSSION
The United States (U.S.) population aged 65 and over is expected to double in the next 25 years.47As the number of older persons continues to rise, emergency medical care will be increasingly affected. Oligoanalgesia, or the undertreatment of pain, is well documented in the EM literature and may disproportionately affect older adults.2–4 Impairment in mental status has been shown to be highly prevalent among older ED patients with a lack of recognition of this impairment by emergency physicians.48–51 Since 2000, The Joint Commission on Accreditation of Healthcare Organizations has made the assessment and management of pain a national quality standard and priority in the hospital accreditation process.52 In addition, the EM community has also identified effective pain control as a quality metric.17 Despite the significantly aging population, there is a paucity of data on the effect of age on analgesia use in the ED. We conducted this study to assess whether age affects the treatment of two of the most common chief complaints of patients seeking emergency care, abdominal pain and back pain.
Our study demonstrated older adults were significantly less likely to receive analgesia in a large cohort of more than 24,000 patients with abdominal or back pain. Our results are similar to prior studies of ED patients presenting with long bone fractures12, 20 and in acute trauma.35 As cognitive impairment is prevalent among older ED patients, this patient population may be at particularly high risk for oligoanalgesia. Older adults may present with significant pain and may not be able to advocate for their own care. We also found that of those patients who received analgesia, older patients waited significantly longer for their medication. Moreover, we found that this disparity was magnified in our oldest group of patients ≥80 years of age.
We identified several potential confounders in analgesia administration: gender, race, triage classification, severe pain, disposition status and presenting complaint of abdominal or back pain. In our study older adults were more likely to be female. A prior study of ED patients with acute abdominal pain demonstrated female sex was independently associated with being less likely to receive analgesic treatment.5 However, older adults were still less likely to receive analgesia even after potential confounders, including gender, were adjusted for in our study. In our study, patients <65 years had a statistically significantly higher mean triage pain score (7.6) as compared to the older groups (7.1 in the 65 – 79 group and 6.5 in age ≥80 group). While this difference was statistically significant, we suggest that it is likely not clinically significant as providers should be motivated to relieve any degree of pain when pain is a component of the patient’s reason for seeking emergency care. Most importantly, in our regression model, we adjusted for severe pain (a pain score of eight to ten) and older adults were still less likely to receive analgesia.
The literature on pain management in older adults suggests a variety of factors that may be obstacles to good pain control in this group. Patient-related factors include reluctance to report pain, fears of addiction with opiates, false belief that pain is a normal part of aging, and fear of being labeled a “bad” patient.53–55 The patients in our study, however, not only reported their pain, but in fact rated it with a number on a pain score. Thus, it is more likely that the barriers in our study were health-provider related. The reasons cited for poor performance at the clinician level include lack of effort to obtain an appropriate assessment, disbelief in patient’s report of pain, exaggerated risk of adverse side effects, misinformation regarding addiction, and lack of training in treating elderly patients with pain.18,56–59 Each one of these possible explanations deserves further attention clinically and more investigation. In addition to unnecessary pain and suffering, negative implications of oligoanalgesia in this patient population include depression and prolonged hospital length of stay.31,32
In older adults, an additional obstacle to effective analgesia is delirium, which can be exacerbated by both oligoanalgesia and overzealous analgesia.30 The literature shows approximately 10% of older ED patients have delirium and an additional 16–22% suffer from cognitive impairment.48, 50, 51Patients who are cognitively impaired may not be able to advocate for their own care in the same way as other patients, which may include a decreased ability to communicate about pain or to request analgesia for painful conditions. While multiple tools exist to assess pain in cognitively impaired older adults,60–63 most of these have not been studied in an emergency care setting.
Our study demonstrates a significant association between older age and decreased and delayed analgesia treatment in abdominal pain and back pain patients who presented to two urban EDs. These findings persisted after controlling for potential risk factors for oligoanalgesia. As the number of older adults continues to rise in the U.S. in the coming decades in the face of increasing use of emergency care, further research is critical to better understand and ameliorate this disparity, with the goal of providing the best possible pain management to older adults. The New Frontiers in Geriatric Research Task Force, in conjunction with the American Geriatrics Society, has previously defined a research agenda in geriatric care covering multiple specialties including EM.64 The Task Force has advocated for improved residency training in the appropriate management of geriatric patients. A category Level B recommendation was assigned in support of prospective studies to assess the use of standardized protocols and educational models for improving the quality of care for older ED patients. We believe our findings support a need for further prospective investigations using standardized protocols to establish whether these interventions improve pain management in the geriatric ED population.
LIMITATIONS
Because this was a retrospective study we are limited in our ability to identify potential reasons (e.g. altered mental status, patient allergy) for delays or failures to initiate analgesic treatment in our population. Additionally, patient desire for pain medication, reassessment of pain scores, and discharge prescriptions for analgesia are unavailable for this analysis. As pain is a dynamic process, we are unable to measure if the evolution of pain influenced clinicians’ willingness to prescribe analgesia. We did not assess other potential agents used for analgesia in abdominal pain (e.g., viscous lidocaine, aluminum/magnesium hydroxide) or low back pain patients (e.g., muscle relaxants). As a nurse manually enters the time of medication administration into the electronic record, there may be a discrepancy between the recorded time and the actual time of administration. For the delay in analgesia, we defined time to analgesia as time from patient placement in the treatment area to time of analgesia, and thus it is unclear whether the delay was due to the ordering or administering of the analgesia, or both. Regardless, we found a delay in analgesia administration among older adults that requires further investigation with future research. We conducted our study in two urban academic centers, and thus our results may not be generalizable to other practice settings. In addition, we used a non-validated 4-point triage classification scale in this study. Other potential confounding variables in analgesia administration that were not available for our analyses include: hemodynamic instability, ED crowding, language barriers, health literacy, medication allergies, mental status or cognitive impairment impeding accurate assessment of pain, and physician bias.
Finally, it is possible that some of the decreased use of opiate medication in the older patients was due to appropriate caution taken by the prescribing physicians concerned about the changing pharmacodynamics of opiates in this population, making them more sensitive to both the analgesic and the adverse effects.65 We would argue, however, that while this concern might have decreased the ordering of an opiate as a first pain medication, it should not have interfered with the use of any pain medication, especially the use of acetaminophen, which we included in our measure of analgesia. We also would have expected this concern to affect the dose of an opiate rather than the choice of an opiate. Furthermore, the delay in prescribing any pain medication in the older groups suggests that there may be other factors that either consciously or unconsciously result in less treatment of pain in older patients.
CONCLUSION
After controlling for potential confounders, older adults who presented to the ED for abdominal pain or back pain were less likely than younger adults to receive analgesia and waited longer for their medication.
Footnotes
Supervising Section Editor: Rick McPheeters, DO
Submission history: Submitted May 10, 2010; Revision received August 3, 2010; Accepted October 22, 2010
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Angela M. Mills, MD, Department of Emergency Medicine, Ground Floor, Ravdin Building, Hospital of the University of Pennsylvania, 3400 Spruce Street, Philadelphia, PA 19104-4283
Email: millsa@uphs.upenn.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008 Aug 6;(7):1–38. [PubMed]
2. Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department.[see comment] American Journal of Emergency Medicine. 1989 Nov;7(6):620–3. [PubMed]
3. Rupp T, Delaney KA. Inadequate analgesia in emergency medicine. Ann Emerg Med. 2004 Apr;43(4):494–503. [PubMed]
4. Stalnikowicz R, Mahamid R, Kaspi S, et al. Undertreatment of acute pain in the emergency department: a challenge. Int J Qual Health Care. 2005 Apr;17(2):173–6. [PubMed]
5. Chen EH, Shofer FS, Dean AJ, et al. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med. 2008 May;15(5):414–8. [PubMed]
6. Raftery KA, Smith-Coggins R, Chen AH. Gender-associated differences in emergency department pain management. Ann Emerg Med. 1995 Oct;26(4):414–21. [PubMed]
7. Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia.[see comment] JAMA. 1993 Mar 24–31;269(12):1537–9. [PubMed]
8. Todd KH, Deaton C, D’Adamo AP, et al. Ethnicity and analgesic practice.[see comment] Annals of Emergency Medicine. 2000 Jan;35(1):11–6. [PubMed]
9. Heins A, Grammas M, Heins JK, et al. Determinants of variation in analgesic and opioid prescribing practice in an emergency department. J Opioid Manag. 2006 Nov–Dec;2(6):335–40. [PubMed]
10. Hostetler MA, Auinger P, Szilagyi PG. Parenteral analgesic and sedative use among ED patients in the United States: combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992–1997. Am J Emerg Med. 2002 May;20(3):139–43. [PubMed]
11. Miner J, Biros MH, Trainor A, et al. Patient and physician perceptions as risk factors for oligoanalgesia: a prospective observational study of the relief of pain in the emergency department.[see comment] Academic Emergency Medicine. 2006 Feb;13(2):140–6. [PubMed]
12. Jones JS, Johnson K, McNinch M. Age as a risk factor for inadequate emergency department analgesia. Am J Emerg Med. 1996 Mar;14(2):157–60. [PubMed]
13. Friedland LR, Pancioli AM, Duncan KM. Pediatric emergency department analgesic practice.Pediatr Emerg Care. 1997 Apr;13(2):103–6. [PubMed]
14. Alexander J, Manno M. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Ann Emerg Med. 2003 May;41(5):617–22. [PubMed]
15. Etzioni S, Chodosh J, Ferrell BA, et al. Quality indicators for pain management in vulnerable elders. J Am Geriatr Soc. 2007 Oct;55(Suppl 2):S403–8. [PubMed]
16. Sloss EM, Solomon DH, Shekelle PG, et al. Selecting target conditions for quality of care improvement in vulnerable older adults. J Am Geriatr Soc. 2000 Apr;48(4):363–9. [PubMed]
17. Terrell KM, Hustey FM, Hwang U, et al. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009 May;16(5):441–9. [PubMed]
18. McNamara RM, Rousseau E, Sanders AB. Geriatric emergency medicine: a survey of practicing emergency physicians. Ann Emerg Med. 1992 Jul;21(7):796–801. [PubMed]
19. Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010 Mar;17(3):316–24. [PMC free article] [PubMed]
20. Hwang U, Richardson LD, Sonuyi TO, et al. The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc. 2006 Feb;54(2):270–5.[PubMed]
21. Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med. 2008 Jun;51(6):769–74. [PubMed]
22. Berger E. Geriatrics and the IOM: did report forget the elderly? Ann Emerg Med. 2006 Dec;48(6):723–5. [PubMed]
23. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002 Mar;39(3):238–47. [PubMed]
24. Sanders AB. Quality in emergency medicine: an introduction. Acad Emerg Med. 2002 Nov;9(11):1064–6. [PubMed]
25. Chin MH, Jin L, Karrison TG, et al. Older patients’ health-related quality of life around an episode of emergency illness. Ann Emerg Med. 1999 Nov;34(5):595–603. [PubMed]
26. Denman SJ, Ettinger WH, Zarkin BA, et al. Short-term outcomes of elderly patients discharged from an emergency department. J Am Geriatr Soc. 1989 Oct;37(10):937–43. [PubMed]
27. Krumholz HM, Radford MJ, Wang Y, et al. Early beta-blocker therapy for acute myocardial infarction in elderly patients. Ann Intern Med. 1999 Nov 2;131(9):648–54. [PubMed]
28. Magid DJ, Masoudi FA, Vinson DR, et al. Older emergency department patients with acute myocardial infarction receive lower quality of care than younger patients. Ann Emerg Med. 2005 Jul;46(1):14–21. [PubMed]
29. Friedmann PD, Jin L, Karrison TG, et al. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med. 2001 Mar;19(2):125–9. [PubMed]
30. Lynch EP, Lazor MA, Gellis JE, et al. The impact of postoperative pain on the development of postoperative delirium. Anesth Analg. 1998 Apr;86(4):781–5. [PubMed]
31. Williamson GM, Schulz R. Pain, activity restriction, and symptoms of depression among community-residing elderly adults. J Gerontol. 1992 Nov;47(6):P367–72. [PubMed]
32. Ferrell BR, Schaffner M. Pharmacoeconomics and medical outcomes in pain management. Semin Anesth. 1997;16(2):152–9.
33. Attard AR, Corlett MJ, Kidner NJ, et al. Safety of early pain relief for acute abdominal pain. BMJ.1992 Sep 5;305(6853):554–6. [PMC free article] [PubMed]
34. LoVecchio F, Oster N, Sturmann K, et al. The use of analgesics in patients with acute abdominal pain. J Emerg Med. 1997 Nov–Dec;15(6):775–9. [PubMed]
35. Neighbor ML, Honner S, Kohn MA. Factors affecting emergency department opioid administration to severely injured patients. Acad Emerg Med. 2004 Dec;11(12):1290–6. [PubMed]
36. Pace S, Burke TF. Intravenous morphine for early pain relief in patients with acute abdominal pain. Acad Emerg Med. 1996 Dec;3(12):1086–92. [PubMed]
37. Ranji SR, Goldman LE, Simel DL, et al. Do opiates affect the clinical evaluation of patients with acute abdominal pain? JAMA. 2006 Oct 11;296(14):1764–74. [PubMed]
38. Thomas SH, Silen W, Cheema F, et al. Effects of morphine analgesia on diagnostic accuracy in Emergency Department patients with abdominal pain: a prospective, randomized trial. J Am Coll Surg. 2003 Jan;196(1):18–31. [PubMed]
39. Zoltie N, Cust MP. Analgesia in the acute abdomen. Ann R Coll Surg Engl. 1986 Jul;68(4):209–10.[PMC free article] [PubMed]
40. Gallagher EJ, Esses D, Lee C, et al. Randomized clinical trial of morphine in acute abdominal pain.Ann Emerg Med. 2006 Aug;48(2):150–160. 160 e151–14. [PubMed]
41. Manterola C, Astudillo P, Losada H, et al. Analgesia in patients with acute abdominal pain.Cochrane Database Syst Rev. 2007;(3):CD005660. [PubMed]
42. The Joint Commission: Pain management Available at:http://www.jointcommission.org/JointCommission/Templates/GeneralInformation.aspx?NRMODE=Published&NRNODEGUID=%7bA08FCD4F-CB99-4B32-B309-1FF1F51CC6C6%7d&NRORIGINALURL=%2fNewsRoom%2fhealth_care_issues%2ehtm&NRCACHEHINT=Guest#9. Accessed July 21, 2010.
43. Gloth FM., 3rd Pain management in older adults: prevention and treatment. J Am Geriatr Soc.2001 Feb;49(2):188–99. [PubMed]
44. Deane G, Smith HS. Overview of pain management in older persons. Clin Geriatr Med. 2008 May;24(2):185–201. [PubMed]
45. The management of chronic pain in older persons: AGS Panel on Chronic Pain in Older Persons. American Geriatrics Society. J Am Geriatr Soc. 1998 May;46(5):635–51. [PubMed]
46. Lumley T, Kronmal R, Ma S. Relative Risk Regression in Medical Research: Models, Contrasts, Estimators, and Algorithms. UW Biostatistics Working Paper Series Working Paper 293. 2006 Jul 19;
47. US Bureau of the Census Current population survey US Government Printing Office. Available at:http://www.census.gov/.
48. Naughton BJ, Moran MB, Kadah H, et al. Delirium and other cognitive impairment in older adults in an emergency department. Ann Emerg Med. 1995 Jun;25(6):751–5. [PubMed]
49. Hustey FM, Meldon S, Palmer R. Prevalence and documentation of impaired mental status in elderly emergency department patients. Acad Emerg Med. 2000 Oct;7(10):1166. [PubMed]
50. Hustey FM, Meldon SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002 Mar;39(3):248–53. [PubMed]
51. Hustey FM, Meldon SW, Smith MD, et al. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med. 2003 May;41(5):678–84. [PubMed]
52. The Joint Commission 2006 Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations; 2006.
53. Brockopp D, Warden S, Colclough G, et al. Elderly people’s knowledge of and attitudes to pain management. Br J Nurs. 1996 May 9–22;5(9):556–558. 560–52. [PubMed]
54. Yates P, Dewar A, Fentiman B. Pain: the views of elderly people living in long-term residential care settings. J Adv Nurs. 1995 Apr;21(4):667–74. [PubMed]
55. Weiner DK, Rudy TE. Attitudinal barriers to effective treatment of persistent pain in nursing home residents. J Am Geriatr Soc. 2002 Dec;50(12):2035–40. [PubMed]
56. Titler MG, Herr K, Schilling ML, et al. Acute pain treatment for older adults hospitalized with hip fracture: current nursing practices and perceived barriers. Appl Nurs Res. 2003 Nov;16(4):211–27.[PubMed]
57. Morley-Forster PK, Clark AJ, Speechley M, et al. Attitudes toward opioid use for chronic pain: a Canadian physician survey. Pain Res Manag. 2003;8(4):189–94. [PubMed]
58. Schumacher JG, Deimling GT, Meldon S, et al. Older adults in the Emergency Department: predicting physicians’ burden levels. J Emerg Med. 2006 May;30(4):455–60. [PubMed]
59. Herr K, Titler MG, Schilling ML, et al. Evidence-based assessment of acute pain in older adults: current nursing practices and perceived barriers. Clin J Pain. 2004 Sep–Oct;20(5):331–40.[PubMed]
60. Hurley AC, Volicer BJ, Hanrahan PA, et al. Assessment of discomfort in advanced Alzheimer patients. Res Nurs Health. 1992 Oct;15(5):369–77. [PubMed]
61. Pautex S, Herrmann F, Le Lous P, et al. Feasibility and reliability of four pain self-assessment scales and correlation with an observational rating scale in hospitalized elderly demented patients. J Gerontol A Biol Sci Med Sci. 2005 Apr;60(4):524–9. [PubMed]
62. Pautex S, Herrmann FR, Le Lous P, et al. Improving pain management in elderly patients with dementia: validation of the Doloshort observational pain assessment scale. Age Ageing. 2009 Nov;38(6):754–7. [PubMed]
63. Pesonen A, Kauppila T, Tarkkila P, et al. Evaluation of easily applicable pain measurement tools for the assessment of pain in demented patients. Acta Anaesthesiol Scand. 2009 May;53(5):657–64.[PubMed]
64. New Frontiers in Geriatrics Research: Geriatric Emergency Medicine. Available at:http://newfrontiers.americangeriatrics.org/chapters/pdf/rasp_16.pdf. Accessed July 21, 2010.
65. Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med. 1997 Jul 28;157(14):1531–6. [PubMed]


