| Author | Affiliation |
|---|---|
| Jonathan H. Shahbazian, BS | David Geffen School of Medicine at UCLA, Department of Orthopedic Surgery, Los Angeles, California |
| Tristan L. Hartzell, MD | David Geffen School of Medicine at UCLA, Department of Orthopedic Surgery, Los Angeles, California |
| Amit K. Pandey, BS | David Geffen School of Medicine at UCLA, Department of Orthopedic Surgery, Los Angeles, California |
| Kodi K. Azari, MD | David Geffen School of Medicine at UCLA, Department of Orthopedic Surgery, Los Angeles, California |
ABSTRACT
In this report we present a case of allergic dermatitis from chronic use of antibiotic ointment mistakenly diagnosed as a localized finger infection.
INTRODUCTION
Allergic/irritant dermatitis can commonly be mistaken by healthcare providers as an infection. Dermatologic reactions secondary to use of topical antibiotic ointment are commonly encountered yet scarcely reported. The purpose of this article is to present a case report of allergic dermatitis from chronic use of topical triple antibiotic ointment (neomycin-polymyxin-bacitracin) mistakenly diagnosed as a bacterial cellulitis despite evaluation by multiple physicians.
CASE REPORT
A 45-year-old right hand dominant male carpenter was referred to our hand center with the diagnosis of chronic and refractory infection of the right long finger (Figures 1 and 2). Six months prior to our evaluation he had removed a “large wood splinter” from his fingertip. He self-treated his wound with hydrogen peroxide soaks and topical antibiotic ointment (neomycin-polymyxin-bacitracin). Over the next month, he experienced progressively worsening erythema, edema, and pain in his digit. He sought medical treatment at an urgent care facility where he was diagnosed with localized cellulitis and was prescribed a 10-day oral course of cephalexin.

Several weeks later, concerned with the lack of symptom relief, the patient presented to an emergency department. A bedside incision and drainage of the volar fingertip was performed, and no gross purulence was expressed. However, with suspicion for infection, he was again discharged with an additional course of oral amoxicillin-clavulanate. Over the next 4 months, the patient was evaluated on 3 separate occasions for his persistent finger complaints, and each time was placed on a short course of oral antibiotics for presumed finger infection.
Upon presentation to our facility 6 months after his initial injury, the patient’s finger had fusiform edema distal to the metacarpal phalangeal joint. He had virtually no ability to actively flex at the interphalangeal joints secondary to edema and moderate pain. Proximally, the digit had some vesicular blistering with frank skin desquamation distally, giving the finger a beefy red appearance. There were no areas of fluctuance or suspected abscess (Figure 1). Radiographs of the hand revealed no undiagnosed fractures, dislocations, subcutaneous air, or retained foreign bodies. Additionally, there were no signs of bone reaction suggestive of osteomyelitis. Our working diagnosis was a chronic infection from atypical mycobacteria or fungus, herpetic whitlow with bacterial super infection, or contact dermatitis.
Our patient work-up revealed normal inflammatory markers including white blood cell count, erythrocyte sedimentation rate, C reactive protein, and a negative rapid herpes simplex test. In the operating room, routine topical tissue cultures were obtained and additional tissue biopsy specimen for culture and microscopic evaluation was sent to dermatopathology. The desquamated skin was removed and no retained foreign bodies were found within the soft tissues.
The results of the intraoperative Gram stains revealed no organisms and few white blood cells. The final fungal, acid-fast bacilli, varicella zoster virus, aerobic and anaerobic cultures were negative.
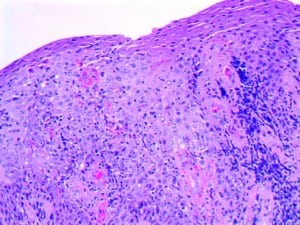
The dermatopathology findings were consistent with an allergic contact dermatitis with hematoxylin and eosin stain revealing epidermal hyperplasia with mild spongiosis, lymphocytic and eosinophilic exocytosis, degranulation of eosinophils at the dermoepidermal junction, and moderately dense superficial to deep perivascular lymphocytic infiltrate with scattered eosinophils (Figure 2). Additional immunostains for varicella zoster virus, herpes simplex virus, fungi, and bacteria were also negative.
Given these findings, administration of a topical steroid (clobetasol propionate 0.05%) was initiated in addition to cessation of the antibiotic ointment. With these treatment recommendations the patient experienced rapid improvement of his symptoms. At his 2-week follow-up appointment his range-of-motion, edema, pain, and erythema had dramatically improved (Figure 1). At final follow-up 4 weeks following our treatment recommendations, digit range of motion and appearance had completely normalized.
DISCUSSION
Allergic contact dermatitis is a common condition often confirmed by identification of the allergen on patch testing. Exposure to the allergenic substance leads to significant disruption of the skin barrier resulting in localized erythema, pruritus, pain, and edema. Repeated offenses by the causative agent or additional substances prevent the skin from healing and produce a cumulative contact dermatitis that further compromises the protective function of the skin. The incidence of hand involvement is estimated to be 4.1 cases per 10,000 persons.1
A number of causes of hand dermatitis have been identified. In 2007, the North American Contact Dermatitis Group performed a cross-sectional analysis of over 950 patients suffering from allergic contact dermatitis of the hand and found neomycin sulfate as well as bacitracin to be 2 of the top 12 causes of hand dermatitis (7.7% and 7.4% of all hand cases, respectively).2 Sensitization to neomycin may be associated with vehicle type3 and duration of use.4,5 Furthermore, simultaneous contact allergy to all 3 ingredients of triple antibiotic ointment has been reported in the literature.6
While allergic contact dermatitis is a common entity affecting the hand, it can be misdiagnosed as a hand infection due to several noteworthy factors. First, there is close proximity in time between the inciting trauma and the resulting application of antimicrobial ointment. Over-the-counter topical antibiotic preparations are frequently applied early in the clinical course by patients who are concerned of risk for infection due to skin breakage. Second, the physical signs and symptoms of allergic contact dermatitis, ie, erythema, pruritus, edema, pain, and vesicle formation, can mimic the signs and symptoms concerning for a severe hand infection. To further complicate matters, repeated exposure to an allergenic compound may compromise the barrier function of the epidermis leading to secondary infection of the hand or digits.
The efficacy of topical antibiotic preparations in treating and preventing various skin infections has been well demonstrated in the literature.7–10 A recent article proposes that triple antibiotic ointment may prove an attractive alternative to oral antibiotics in select cases of skin wound management because resistance does not develop readily.11 Then again, in a previous study by Smack et al,12 no clinically significant differences in postoperative infection rates or wound healing were found between those treated with white petrolatum and bacitracin ointment.
The debate about the role for topical antibiotic preparations is unlikely to diminish. Therefore, it is advantageous to outline strategies to avoid the misdiagnosis of allergic contact dermatitis. Especially in cases of chronic, repeat, or relapsing hand infection, it becomes incumbent upon the physician to invest the time necessary to obtain a thorough history detailing the initial event and all treatments, prescribed or otherwise, which the patient has since used. Barring complicating comorbidities, infections treated empirically with oral or parental antibiotics should begin to show clinical response within 48 to 72 hours of administration. In the event that clinical response to treatment is not evident or components of the clinical picture do not seem to fit, the physician should maintain a very low threshold for obtaining a biopsy and sending tissue specimen for pathologic diagnosis.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence
Jonathan H. Shahbazian, BS
David Geffen School of Medicine at UCLA, Department of Orthopedic Surgery, 10945 Le Conte Ave, Rm 33-55G PVUB, Los Angeles, CA 90095
E-mail: jshahbazian@gmail.com.
REFERENCES
1. Dickel H, Kuss O, Schmidt A, et al. Importance of irritant contact dermatitis in occupational skin disease. Am J Clin Dermatol. 2002;3:283–289. [PubMed]
2. Warshaw EM, Ahmed RL, Belsito DV, et al. North American Contact Dermatitis Group. Contact dermatitis of the hands: cross-sectional analyses of North American Contact Dermatitis Group Data, 1994–2004. J Am Acad Dermatol. 2007;57:301–314. [PubMed]
3. Bjarnason B, Flosadottir E. Patch testing with neomycin sulfate. Contact Dermatitis. 2000;43:295–302. [PubMed]
4. Leyden JJ, Kligman AM. Contact dermatitis to neomycin sulfate. JAMA. 1979;242:1276–1278.[PubMed]
5. Prystowksy SD, Allen AM, Smith RW, et al. Allergic contact hypersensitivity to nickel, neomycin, ethylenediamine, and benzocaine: relationships between age, sex, history of exposure, and reactivity to standard patch tests and use tests in a general population. Arch Dermatol. 1979;115:959–962. [PubMed]
6. Grandinetti PJ, Fowler JF. Simultaneous contact allergy to neomycin, bacitracin, and polymyxin. J Am Acad Dermatol. 1990;23:646–647. [PubMed]
7. Bass JW, Chan DS, Creamer KM, et al. Comparison of oral cephalexin, topical mupirocin and topical bacitracin for treatment of impetigo. Pediatr Infect Dis J. 1997;16:708–710. [PubMed]
8. Ealls LD, Mertz PM, Piovanetti Y, et al. Topical antibiotic treatment of impetigo with mupirocin. Arch Dermatol. 1986;122:1273–1276. [PubMed]
9. Davis S, Cazzaniga A, Eaglstein W, et al. Over-the-counter topical antimicrobials: effective treatments? Arch Dermatol Res. 2005;297:190–195. [PubMed]
10. Dire DJ, Coppola M, Dwyer DA, et al. Prospective evaluation of topical antibiotics for preventing infections in uncomplicated soft-tissue wounds repaired in the ED. Acad Emerg Med. 1995;2:4–10.[PubMed]
11. Bonomo RA, Van Zile PS, Li Q, et al. Topical triple-antibiotic ointment as a novel therapeutic choice in wound management and infection prevention: a practical perspective. Expert Rev Anti Infect Ther.2007;5:773–782. [PubMed]
12. Smack DP, Harrington AC, Dunn C, et al. Infection and allergy incidence in ambulatory surgery patients using white petrolatum vs bacitracin ointment. A randomized controlled trial. JAMA.1996;276:972–977. [PubMed]


