| Author | Affiliation |
|---|---|
| Coral Bays-Muchmore, BS | University of Washington School of Medicine, Seattle, Washington |
| Deion T. Sims, BS | University of Washington School of Medicine, Seattle, Washington |
| Joel A. Gross, MD, MS | University of Washington School of Medicine, Department of Radiology, Seattle, Washington |
| Jonathan S. Ilgen, MD, MCR | University of Washington School of Medicine, Department of Emergency Medicine, Seattle, Washington |
ABSTRACT
Case Presentation
A 35-year-old woman presented to the emergency department with severe right inguinal pain. Her medical history was non-contributory and there was no known trauma or injury to the region. Amid concern for an incarcerated inguinal hernia, a computed tomography was obtained revealing a linear foreign body (FB) lateral to the femoral vessels. The FB was removed without complication at bedside and found to be a beading needle likely occultly lodged three days prior.
Discussion
Occult inguinal FBs are rare but can lead to deep venous thrombosis or pulmonary embolism if in or near vessels. By nature of being occult, an absence of ingestion, insertion, or penetrative history should not preclude consideration of a FB etiology. Computed tomography imaging is crucial in determining the urgency of, and approach to, inguinal foreign body removal.
CASE PRESENTATION
A 35-year-old woman presented to the emergency department with severe right inguinal pain that began while pushing a grocery cart. Physical examination revealed tenderness and fullness in the right inguinal crease without erythema, warmth, or skin trauma. Amid concern for an incarcerated inguinal hernia, a computed tomography (CT) was obtained (Image 1).
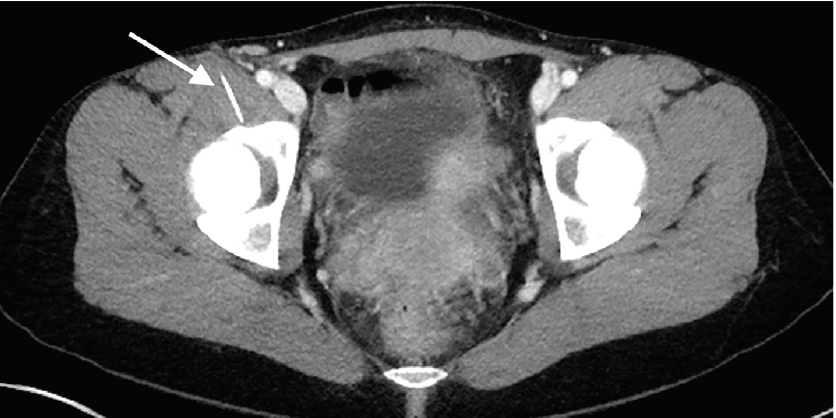
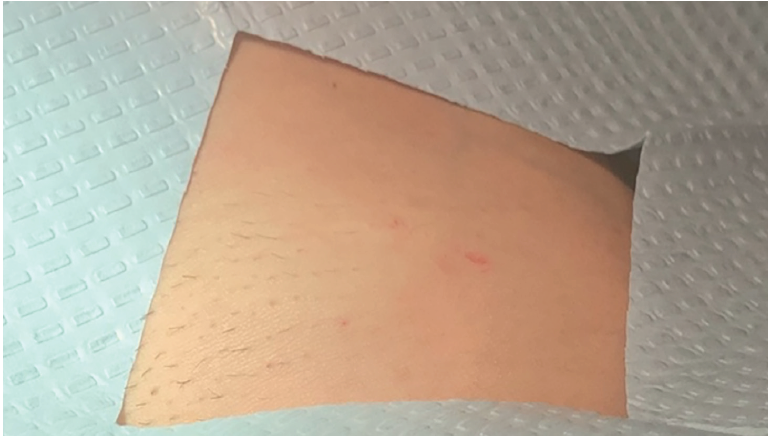
The CT demonstrated a linear 3.8-centimeter (cm) foreign body (FB) extending from the skin into the right iliopsoas muscle (Image 1) without gas or fluid along its length and without vessel involvement. Upon re-interview and re-examination, the patient did not report any preceding history that would explain this finding and there was no visible point of entry on her skin (Image 2).
The CT imaging confirmed this FB to be lateral to the femoral vessels in a location amenable to bedside removal in the ED. The skin was incised, and a 4-cm metallic FB was removed (Image 3).

Upon removal, the patient identified the FB as a beading needle and presumed that it had become lodged three days prior when she had fallen asleep adjacent to her beading materials. Following the FB removal, the incision was closed, and the patient was discharged without complication.
DISCUSSION
Occult FBs are rare, although needles are common culprits due to their ease of entering tissue with minimal pain and inflammation.1 Inguinal needle FBs are uncommon but can generally be grouped into those associated with intravenous drug use,2 acupuncture needle retention,3 and accidental/inexplicable cases.4,5 Deep venous thrombosis may be the initial clinical manifestation of occult inguinal FBs in or near vessels.5 As illustrated by this case and others,4,5 FBs remain an important consideration even without known history of ingestion, insertion, or penetrative injury. Computed tomography imaging is crucial in determining the urgency of, and approach to, inguinal FB removal.
CPC-EM Capsule
What do we already know about this clinical entity?
Foreign body (FB) injuries are typically apparent from clinical history and have exam findings compatible with tissue injury and inflammation.
What is the major impact of the image(s)?
These images demonstrate that a FB can be present without any corresponding history or external exam findings, with the potential for serious downstream sequelae.
How might this improve emergency medicine practice?
Although rare, occult FBs must be considered by emergency providers as a source of pain despite an absence of clinical history.
Footnotes
Section Editor: Scott Goldstein, MD
Full text available through open access at http://escholarship.org/uc/uciem_cpcem
Patient consent has been obtained and filed for the publication of this image in emergency medicine.
Address for Correspondence: Jonathan Ilgen, MD, MCR, University of Washington School of Medicine, Department of Emergency Medicine, 325 9th Avenue, Box 359702, Seattle, WA 98104-2499. Email: ilgen@uw.edu. 5:129 – 130
Submission history: Revision received October 13, 2020; Submitted December 11, 2020; Accepted December 18, 2020
Conflicts of Interest: By the CPC-EM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Al-Jasmi F, Al-Khenaizan S. Cutaneous foreign bodies: elusive presentation. Case report and review of the literature. Int J Dermatol. 2002;41(5):293-5.
2. Gladman J. Pins and needles in the groin: an incidental finding of retained needle fragments in an intravenous drug user. BMJ Case Rep. 2019;12(2):e226220.
3. Hollander JE, Dewitz A, Bowers S. Permanently imbedded subcutaneous acupuncture needles: radiographic appearance. Ann Emerg Med. 1991;20(9):1025-6.
4. Lloyd RF, Feeney C. Adolescent hip pain: the needle in the haystack. A case report. Physiotherapy. 2011;97(4):354-6.
5. Lebon M, Ancedy Y, Boccara F, et al. Foreign body causing superficial venous thrombosis and subsequent pulmonary embolism: a case report. Eur Heart J Case Rep. 2018;2(4):yty125.


