| Author | Affiliation |
|---|---|
| Jarrod Mosier, MD | University of Arizona, Departments of Emergency Medicine and Internal Medicine, Tucson, Arizona |
| Grant Roper, MD | University of Arizona, Department of Emergency Medicine, Tucson, Arizona |
| Daniel Hays, PharmD | University of Arizona, Department of Emergency Medicine, Tucson, Arizona |
| John Guisto, MD | University of Arizona, Department of Emergency Medicine, Tucson, Arizona |
Introduction
Case reports
Discussion
Conclusion
ABSTRACT
Introduction:
Migraine headaches requiring an emergency department visit due to failed outpatient rescue therapy present a significant challenge in terms of length of stay (LOS) and financial costs. Propofol therapy may be effective at pain reduction and reduce that length of stay given its pharmacokinetic properties as a short acting intravenous sedative anesthetic and pharmacodynamics on GABA mediated chloride flux.
Methods:
Case series of 4 patients presenting to an urban academic medical center with migraine headache failing outpatient therapy. Each patient was given a sedation dose (1 mg/kg) of propofol under standard procedural sedation precautions.
Results:
Each of the 4 patients experienced dramatic reductions or complete resolution of headache severity. LOS for 3 of the 4 patients was 50% less than the average LOS for patients with similar chief complaints to our emergency department. 1 patient required further treatment with standard therapy but had a significant reduction in pain and a shorter LOS. There were no episodes of hypotension, hypoxia, or apnea during the sedations.
Conclusion:
In this small case series, sedation dose propofol appears to be effective and safe for the treatment of refractory migraines, and may result in a reduced LOS.
INTRODUCTION
Acute migraine headache accounts for approximately 2.1 million emergency department (ED) visits and incurs over $600 million in annual healthcare costs.1,2 Common ED treatments for migraine headache include various pharmacologic agents, oxygen and/or rehydration.2 While these treatments are usually ultimately effective, they often have the patient occupying a treatment space for extended periods. This potentially slows patient flow in already burdened ED’s. A series of small studies and case reports have shown rapid relief of both chronic headache and acute migraine headache using propofol, a lipid soluble short-acting intravenous anesthetic.3–9 The majority reported occurred as outpatient procedures or in a monitored pre-anesthesia care unit.3,4 Only 1 small series was performed in adult ED patients at sub-sedation doses of 10 mg every 5 minutes.10 Propofol is an ultra short-acting anesthetic that increases GABA mediated chloride flux, exerting an inhibitory effect on synaptic transmission, cerebral blood flow and metabolic rate, and central serotonergic neurons in the raphe nuclei.11–16 We therefore postulated that propofol could safely be used in an ED setting not only with efficacy but also a substantial reduction in ED length of stay (LOS). Based upon the aforementioned studies, we used sedation dose propofol in a convenience sample of migraine patients presenting to the authors in the ED having failed their usual outpatient treatments. We report a case series of four patients safely and rapidly treated for migraine headache in the ED using sedative dosing of propofol, which we hope will form the basis for a research protocol to evaluate this therapy on a more rigorous basis.
CASE REPORTS
Patient 1
A 51-year-old male with past medical history of migraines, hypertension and depression presented with headache for the previous 24 hours. The pattern was typical of his migraine headaches. Initial vital signs were heart rate 97, blood pressure 135/93, respiratory rate 16 and pain scale of 9/10. His migraine had not responded to his home medications. Prior migraines requiring ED visits were treated with: prochlorperazine, diphenhydramine, acetaminophen, droperidol, ibuprofen, morphine, and normal saline. Physical exam was unremarkable for any focal neurologic findings other than photophobia.
The patient was consented for procedural sedation and treated with 1 mg/kg of propofol. Thirteen minutes after medication the patient was arousable. The patient was observed for an additional 1 hour and 9 minutes during which the headache decreased to 2/10 and then complete resolution with no further pharmacologic intervention. He was reassessed and discharged home with a total LOS of 2 hours. Discharge vital signs were heart rate 77, blood pressure 137/94, respiratory rate 16.
Patient 2
A 51-year-old woman with past medical history of hypertension and migraines presented with 12 hours of 9/10 headache typical of her past migraines. Repeated doses of her home sumatriptan (100 mg) had failed. Initial vital signs were heart rate 60, blood pressure 193/105, respiratory rate 14. A full neurologic examination found no focal deficits. Initial treatment with compazine 10 mg intravenous (IV) and IV hydration with 1 L of normal saline was attempted with a pain score remaining 9/10. The patient was then consented and treated with 1 mg/kg propofol. A complete resolution of symptoms was achieved with a LOS of 2.75 hours. Discharge vital signs were heart rate 48, blood pressure 134/97, respiratory rate 18.
Patient 3
A 62-year-old woman with a history of complex migraine presents with 5 days of 9/10 headache, with no relief from her home regimen of ibuprofen and rizatriptan. Past medical history was significant for irritable bowel syndrome, hepatitis C, and arthritis. She also complained of photophobia, left-sided facial paresthesias, and nausea, all of which were consistent with past migraine episodes. Initial vital signs were heart rate 73, blood pressure 151/84, and respiratory rate 18. Physical exam was remarkable only for decreased sensation on the left side of the face, in all 3 dermatomes. The patient was consented and treated with 1 mg/kg propofol. After five minutes she reported marked improvement with her pain score reduced to 3/10. On repeat evaluation she requested further treatment and was given intravenous compazine 10 mg IV, diphenhydramine 50 mg IV, and ketorolac 30 mg IV with 2 L intravenous saline. At discharge she reported full resolution of headache symptoms. Her total LOS was 4.8 hours. Discharge vital signs were heart rate 61, blood pressure 137/71, and respiratory rate 18.
Patient 4
A 59 year old man with past medical history significant for migraines, insomnia, and hypothyroidism presented with four hours of 8/10 right-sided headache and photophobia. Symptoms were consistent with his typical migraine. Home treatment with naproxen and gabapentin had failed to improve his symptoms. Previous migraines requiring ED admission were treated with prochlorperazine 10 mg IV, diphenhydramine 50 mg IV, ketorolac 30 mg IV, morphine 6 mg IV, and promethazine 12.5 mg IV. Initial vital signs were heart rate 79, blood pressure 116/78, and respiratory rate 18. Neurologic examination revealed no focal deficits. The patient was then consented and treated with 1 mg/kg propofol. After 5 minutes the patient reported near complete resolution of symptoms with a pain score of 1/10. He was able to ambulate, tolerate oral intake, and was discharged shortly thereafter. His ED LOS was 2.8 hours. Discharge vital signs were heart rate 80, blood pressure 104/66, and respiratory rate 16.
DISCUSSION
All 4 reported patients carried a prior diagnosis of migraine headache and had failed their standard home rescue therapy. Due to the unconventional nature of the off-label use of propofol therapy for migraines in the ED, patients were only considered a candidate by 1 of the authors if they carried a diagnosis of migraines as documented in the patient record, no suspicion of alternate diagnosis, and had unsuccessfully tried the outpatient rescue medication. Patients were not considered if they had fever, altered mental status, history of trauma or suspicion of alternate diagnosis. If the physician felt the patient was a good candidate, they were offered the therapy and all patients were consented for procedural sedation after careful explanation of the risks and benefits of this unconventional therapy. For comparison purposes, we obtained LOS for all 465 patients who were treated and released with a primary diagnosis code for migraine (ICD-9 codes 346–346.9) in fiscal year 2011 (July 1, 2010–June 30, 2011). The mean length of stay at this urban academic emergency department for these patients was 6.5 hours (standard deviation [SD] 3.76 hours, 95% confidence interval [CI] 6.16–6.84). Patients in the case series were seen and treated during this same time interval. LOS for patients included in the case series was verified using nursing documentation of the time the patient was placed in an examination room and the time of discharge from the Emergency Department. When available, we also calculated an average LOS for these patients with previous ED visits for migraine headache. Patients receiving propofol therapy were placed on a cardiac monitor, supplemental oxygen by nasal cannula, end-tidal CO2 monitor, and had one:one nursing care during the sedation, as is standard practice for all procedural sedations performed in our emergency department. The drug was administered as a slow infusion over 1 minute through a peripheral IV with a 10 mL syringe until the patient fell asleep without a rise in end-tidal CO2 or a decrease in respiratory rate or oxygen saturation. The maximum dose of propofol allowed was 1 mg/kg and was stopped short if the desired effect was achieved with a smaller dose. The patient was allowed to sleep until they woke up on his or her own. See table for summary of dose given, length of stay, and pain score of each patient.
The patients reported in this series had an average LOS of 3.1 hours (SD 1.2 hours, 95% CI 1.92–4.28). All patients reported a substantial decrease in symptoms. Two of the patients were also treated with standard migraine therapy, 1 after propofol treatment and 1 before. These patients still had shorter LOS than the average patient with migraine headache in our urban academic medical center. There were no periods of apnea or hypotension with the propofol administration, and there were no other complications reported. One patient in this series was discharged with a short course of hydrocodone/APAP while the other three did not receive narcotics in the emergency department nor were they given prescriptions for outpatient use.
Two patients had been seen multiple times in the previous 12 months with similar presentations. The most recent 3 visits were analyzed. For both patients the LOS was markedly reduced when they were treated with propofol (Table).
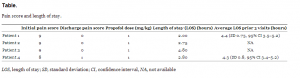
Pain score and length of stay.
This series shows a promising reduction in headache symptoms using sedative dosing of propofol. Reducing emergency department LOS while safely assessing and treating patients is one of the greatest challenges facing emergency physicians today. Headache is a common presenting complaint that can often be treated symptomatically without extensive diagnostic testing. Alleviating headache symptoms rapidly could improve ED patient flow and have a possible positive effect on patient satisfaction with treatment. One concern, however, is developing a propofol dependency17,18 much like the widespread narcotic dependence that is seen widely by EDs throughout the country. Schneider and colleagues have reported the only known case of lay-person propofol dependence17, and despite the high abuse potential18, no other data exists regarding this phenomenon. None of the patients reported in this series have returned for repeat therapy.
CONCLUSION
Based upon this limited experience, propofol shows promise for the treatment of ED patients who present with migraine symptoms refractory to their outpatient rescue therapy. Future research should more formally evaluate the safety, effectiveness, and cost effectiveness of sedation dosing of propofol for refractory migraines.
Footnotes
Address for Correspondence: Jarrod Mosier, MD, University of Arizona, Departments of Emergency Medicine and Internal Medicine, address. Email: jmosier@aemrc.arizona.edu. 11 / 2013; 14:646 – 649
Submission history: Revision received May 2, 2013; Submitted June 23, 2013; Accepted July 22, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none
REFERENCES
1. Barron R, Carlsen J, Duff SB Estimating the cost of an emergency room visit for migraine headache. J Med Econ. 2003; 6:43-53
2. Edlow JA, Panagos PD, Godwin SA Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med. 2008; 52:407-436
3. Krusz JC, Scott V, Belanger J Intravenous propofol: unique effectiveness in treating intractable migraine. Headache. 2000; 40:224-230
4. Roffey P, Thangathurai D Propofol in the treatment of presurgical headache and nausea. Headache. 2002; 42:327
5. Drummond-Lewis J, Scher C Propofol: a new treatment strategy for refractory migraine headache. Pain Med. 2002; 3:366-369
6. Mendes PM, Silberstein SD, Young WB Intravenous propofol in the treatment of refractory headache. Headache. 2002; 42:638-641
7. Bloomstone JA Propofol: a novel treatment for breaking migraine headache. Anesthesiology. 2007; 106:405-406
8. Simmonds MK, Rashiq S, Sobolev IA The effect of single-dose propofol injection on pain and quality of life in chronic daily headache: a randomized, double-blind, controlled trial. Anesth Analg. 2009; 109:1972-1980
9. Sheridian D, Spiro D, Nguyen T Low-Dose Propofol for the Abortive Treatment of Pediatric Migraine in the Emergency Department. Pediatr Emerg Care. 2012; 28:1293-1296
10. Soleimanpour H, Taheraghdam A, Rajaei Ghafouri R Improvement of refractory migraine headache by Propofol: Case series. Int J Emerg Med. 2012; 5:19
11. Nishikawa T, Scatton B Inhibitory influence of GABA on central serotonergic transmission. Involvement of the habenuloraphe pathways in the GABAergic inhibition of ascending cerebral serotonergic neurons. Brain Res. 1985; 331:81-90
12. Vandesteene A, Trempont V, Engelman E Effect of propofol on cerebral blood flow and metabolism in man. Anaesthesia. 1988; 43:42-43
13. Hara M, Kai Y, Ikemoto Y Enhancement by propofol of the gamma-aminobutyric acidA response in dissociated hippocampal pyramidal neurons of the rat. Anesthesiology. 1994; 81:988-994
14. Alkire MT, Haier RJ, Barker SJ Cerebral metabolism during propofol anesthesia in humans studied with positron emission tomography. Anesthesiology. 1995; 82:393-403
15. Orser BA, Bertlik M, Wang LY Inhibition by propofol (2,6 di-isopropylphenol) of the N-methyl-D-aspartate subtype of glutamate receptor in cultured hippocampal neurones. Br J Pharmacol. 1995; 116:1761-1768
16. Sanna E, Garau F, Harris RA Novel properties of homomeric beta 1 gamma-aminobutyric acid type A receptors: actions of the anesthetics propofol and pentobarbital. Mol Pharmacol. 1995; 47:213-217
17. Schneider U, Rada D, Rollnik JD Propofol dependency after treatment of tension headache. Addict Biol. 2001; 6:263-265
18. Wilson C, Canning P, Caravati EM The abuse potential of propofol. Clin Toxicol (Phila)f. 2010; 48:165-170


