| Author | Affiliation |
|---|---|
| Mark E. Sutter, MD | University of California, Davis, Department of Emergency Medicine, Davis, CA |
| Michael F. Daily, MD | University of California, Davis, Department of Surgery, Davis, CA |
| Kelly P. Owen, MD | University of California, Davis, Department of Emergency Medicine, Davis, CA |
| G. Patrick Daubert, MD | University of California, Davis, Department of Emergency Medicine, Davis, CA |
| Timothy E. Albertson, MD, PhD | University of California, Davis, Department of Medicine, Davis, CA |
ABSTRACT
Emergency physicians (EP) and medical toxicologists are integral in identifying and treating patients with overdoses. Transplant centers are expanding acceptance criteria to consider those with poison-related deaths. We present a case of a simultaneous gunshot wound to the head and an acetaminophen overdose. This case highlights the importance of EPs and medical toxicologists in recognizing the medical complexity of suicides, optimizing treatment, and timing of organ procurement. Early antidote administration and aggressive supportive care allowed the patient to be evaluated as a potential donor. EPs and medical toxicologists have integral roles in overdose patients as organ donors.
INTRODUCTION
Emergency physicians (EP) often play important roles in the initial stabilization of patients who later become organ donors. They also play vital roles in the transplantation process through recognition of potential drug overdoses. As the list of patients awaiting transplantation grows, acceptance criteria by transplant centers have expanded to consider those who have died due to drug intoxication.1,2 Between 2004 and 2008, the Organ Procurement and Transplantation Network classified drug intoxication as cause of death in approximately 3% of all donors.3 (Table 1).

While the vast majority of drug intoxications manifest symptoms within the first few hours, delayed or “silent toxins” exist. The classic examples of poisonings with delayed manifestations include mushroom poisoning from the Amanita sp. and acetaminophen. Both are hepatotoxins that may not produce symptoms for the first 12–24 hours and usually do not manifest life- or organ-threatening toxicity until 72–96 hours after the ingestion.4
Delays in toxicity must be considered when evaluating an overdose patient as a potential transplant donor.
Acetaminophen-induced organ injury is known to cause renal failure with or without evidence of hepatotoxicity, further complicating the evaluation of such donors.5–8
We describe the case of a 17-year-old male with a simultaneous gunshot wound to the head in association with an acetaminophen overdose. This case demonstrates the importance of considering the complex medical issue of suicide and optimizing patient care with supportive care and early antidote administration.
CASE REPORT
A 17-year-old male with no significant past medical history was brought to the emergency department (ED) after a self-inflicted gunshot wound to the head. In the ED the mother was specifically asked about potential overdoses. She stated that there was a recently purchased bottle of acetaminophen in the garage where her son had been working. She had asked him to bring her the bottle; approximately five minutes later, he went into another room and she heard a gunshot.
Upon arrival in the ED, the patient was intubated without medication. He had a systolic blood pressure of 130 mm Hg, a pulse of 111 beats per minute, a respiratory rate of 16 via bag-assisted respirations and a temperature of 36.5°C. Physical exam was notable for a single penetrating wound to the right temporal bone. Pupils were fixed and dilated. There was no evidence of trauma anywhere else on his body. The computed tomography scan of his brain demonstrated a non-survivable head injury with multiple skull fractures, intraparenchymal, intraventricular, subarachnoid and subdural blood. Additionally, there was significant cerebral edema with evidence of tonsillar herniation. The remainder of the physical exam was consistent with brain death, with no additional signs of trauma. Initial laboratories returned with a hemoglobin, 11 gm/dL; platelets, 218 103/mm3; sodium, 138 mEq/L; potassium, 2.9 mEq/L; chloride, 104 mEq/L; bicarbonate, 22 mEq/L; blood urea nitrogen, 12 mg/dL; and creatinine, 0.96 mg/dL. His aspartate transaminase (AST) was mildly elevated at 50 IU/L and his alanine transferase was normal at 20 IU/L. Initial international normalized ratio was 1.26. His acetaminophen level drawn at arrival was markedly elevated at 134 mg/L. The EPs initiated N-acetylcysteine (NAC) therapy and requested a medical toxicology consultation. Family expressed their interest in organ and tissue donation. The intensive care service requested input from the toxicology team with regard to immediate treatment for the patient, as well as timing and toxicological issues that could affect organ donation and transplantation.
After conversations with the family, there was no further history available regarding potential ingestions or time of ingestion. An exact time of ingestion could not be determined. The family located the bottle and found approximately 20 grams of acetaminophen missing, an amount capable of producing fulminant hepatic failure. Given the lack of overdose information with evidence of a significant ingestion, intravenous NAC was continued indefinitely. Charcoal therapy was considered, but with the unknown time of ingestion and the duration of time elapsed from pre-hospital transportation through ED resuscitation, the patient was outside the window for likely therapeutic benefit.
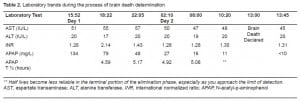
The process of brain death evaluation was initiated. Our institutional policy for pediatric patients (defined as <18 years of age) is to have two separate brain death exams on separate calendar days. During this period, a multidisciplinary group of pediatric intensive care physicians and medical toxicologists participated in supportive care. Initial plans for heart, lung, and pancreas donation were decided, but the viability of the kidneys and liver were unknown. The next 24 hours of laboratory evaluation is summarized in Table 2.
After the patient was declared brain dead, organs were recovered and transplanted into six different recipients. The heart, lung, pancreas and one of the kidneys were successfully transplanted, and at three months post transplant all organs were functioning well. The liver was split, with one recipient also receiving a kidney. The patient who received the right hemi-liver alone did not experience complications and had excellent allograft function at three months. The patient who received both the left hemi-liver and a kidney had a prolonged intensive care hospitalization for two months post transplant for infectious complications; however, the transplanted organs were functioning normally during the intensive care stay and at three months post transplantation.
DISCUSSION
This unique case highlights the importance of considering the complex medical issues related to suicide, recognition of a potential ingestion and early antidote administration. Additionally, this case demonstrates many toxicological issues in both potential donor and transplant recipients. There is limited data on organ recovery and transplant in donors with overdoses. The possibility of delayed manifestation of toxicity becomes more complicated when the immediate cause of death was not due to the ingestion.
There were no identified contraindications to transplant the heart, lungs, pancreas, and intestines. Several issues needed to be addressed regarding the kidneys and liver. One of these was the timing of organ recovery. No specific criteria exist for the timing of liver transplantation using a donor with acetaminophen overdose and elevated AST. While delay in recovery may be reassuring to the centers accepting the liver and kidneys, the possibility existed that the traumatic brain injury itself could trigger many pathologic processes, such as diffuse intravascular coagulation, which could affect the viability of the other organs.
Acetaminophen has been known to induce renal insufficiency in approximately 2% of overdoses.9There have been case reports describing kidney donation after acetaminophen overdose 10. In some of these cases, the donors had elevated creatinine, and in one case the patient was oligoanuric for three hours prior to harvesting organs. However, the cause of death in these cases was liver failure from acetaminophen overdose. Therefore it is hard to extrapolate these results to prospectively predict if a kidney will be viable when the cause of death is unrelated.
Predicting which patients with acetaminophen overdose will develop renal failure has been difficult to elucidate beyond general risk factors for hepatic failure. A prospective study evaluating proteinuria found it was not an early marker that would progress to renal failure in acetaminophen overdoses.11 Additionally, the onset of renal failure typically occurred between day two and day five after the overdose with peak creatinine levels on day seven.6, 12 This was concerning given the fact that our patient was declared brain dead on day two. The majority of case reports demonstrated creatinine that had returned to baseline within one month, suggesting that renal failure is likely reversible. 12
While information regarding acetaminophen-induced renal failure is limited, hepatotoxicity from acetaminophen is well studied. In significant acetaminophen overdoses, transaminases typically begin to rise between 18 and 30 hours, followed by signs of multi-organ involvement typically manifesting between 72 and 96 hours post-ingestion. 4 Additionally, the initiation of NAC prior to eight hours post ingestion has been shown to prevent liver failure regardless of initial acetaminophen level.13 This patient had an unknown time of ingestion, making it impossible to determine the risk of hepatotoxicty with his first level of 134 mg/L.
Our literature search returned no published reports of liver donation after acetaminophen overdose. This is not surprising, as most patients with acetaminophen overdose either have full recovery, or death due to complications of hepatic failure. Given this lack of data, it was unclear at what time liver donation could be considered safe. Typically, in treatment of an acetaminophen overdose, therapy with NAC is initiated and transaminase levels are followed in conjunction with confirmation that the acetaminophen level becomes undetectable. However, the timing of the recovery of other organs prohibited this delay to follow the liver function.
The institutional policy regarding pediatric brain death provided the opportunity to check serial acetaminophen levels prior to declaring the patient brain dead. The half-lives listed in Table 2 range from 4.59 to 5.17 hours. As oxidative damage to the liver occurs, the ability to eliminate the drug decreases and thus prolongs the calculated half-life. Two previous studies evaluating acetaminophen half-life determinations to predict toxicity have found that half-lives less than 2.5 hours and 3 hours respectively make toxicity unlikely.14,15 Studies have also shown that half-lives of greater than four hours put the patient at increased risk of hepatotoxicity and demonstrate the longer the half-life, the higher the rate of hepatotoxicity. 16, 17 Typically, the use of acetaminophen half-lives to predict toxicity is not recommended due to lack of specificity and multiple confounders such as ongoing gastrointestinal absorption, or co-ingestions. Given the half-lives of this patient were greater than four hours, transplantation of the liver was considered high risk.
The patient’s transaminases failed to change over the 24 hours of observation prior to the declaration of brain death. Besides the possibility that not enough time had elapsed to see the transaminases rise, two additional explanations are possible. First, given our lack of knowledge regarding the time of ingestion, the initial level of 134 mg/L could have been less than a four- hour level and reflected significant continued absorption. With serial levels decreasing, this would make his ingestion low probability for hepatotoxicity. The second explanation for his lack of hepatotoxicity may be the result of the early initiation of NAC stopping hepatotoxicity from occurring.
In summary, early recognition of a potential overdose and NAC administration in the ED optimized the patient as a potential donor. The use of overdose patients as organ donors may serve as an increasing source of organs to meet the growing needs of patients awaiting transplant. It is vital that EPs and medical toxicologists play integral roles in overdose patients as organ donors.
Footnotes
We would like to thank Golden State Donor Services for their effort and contribution to this manuscript.
Supervising Section Editor: Brandon K. Wills, DO, MS
Submission history: Submitted March 26, 2010; Accepted May 10, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Mark Sutter, MD, Department of Emergency Medicine, University of California, Davis 2315 Stockton Blvd, Sacramento CA, 95817
Email: mark.sutter@ucdmc.ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Komokata T, Nishida S, Ganz S, et al. The impact of donor chemical overdose on the outcome of liver transplantation. Transplantation. 2003 Aug 27;76(4):705–8. [PubMed]
2. Gok MA, Gupta A, Olschewski P, et al. Renal transplants from non-heart beating paracetamol overdose donors. Clin Transplant. 2004;18(5):541–6. [PubMed]
3. Organ Procurement and Transplantation Network (OPTN) [Accessed on May 27, 2009]. Available at: http://optn.transplant.hrsa.gov/latestdata/rpt.data.asp.
4. Rumack BH, Peterson RG, Koch GG, et al. Acetaminophen overdose. 662 Cases with evaluation of oral acetylcysteine treatment. Arch Intern Med. 1981;141:380–385. [PubMed]
5. Jones AF, Vale JA. Paracetamol poisoning and the kidney. J Clin Pharm Ther. 1993;18(1):5–8.[PubMed]
6. Mazer M, Perrone J. Acetaminophen-induced nephrotoxicity: pathophysiology, clinical manifestations, and management. J Med Toxicol. 2008;4(1):2–6. [PMC free article] [PubMed]
7. Davenport A, Finn R. Paracetamol (acetaminophen) poisoning resulting in acute renal failure without hepatic coma. Nephron. 1988;50(1):55–6. [PubMed]
8. Boutis K, Shannon M. Nephrotoxicity after acute severe acetaminophen poisoning in adolescents.J Toxicol Clin Toxicol. 2001;39:441–445. [PubMed]
9. Prescott LF. Paracetamol overdosage: Pharmacological considerations and clinical management.Drugs. 1983;25:290–314. [PubMed]
10. Andrews PA, Koffmann CG. Kidney donation after paracetamol overdose. BMJ. 1993;306:1129.[PMC free article] [PubMed]
11. Benhalim S, Leggett GE, Jamie H, et al. Proteinuria is unrelated to the extent of acute acetaminophen overdose: a prospective clinical study. J Med Toxicol. 2008;4(4):232–7.[PMC free article] [PubMed]
12. Von Mach MA, Hermanns-Clausen M, Koch I, et al. Experiences of a poison center network with renal insufficiency in acetaminophen overdose: an analysis of 17 cases. Clin Toxicol (Phila)2005;43(1):31–7. [PubMed]
13. Smilkstein MJ, Knapp GL, Kulig KW, et al. Efficacy of oral N-acetylcysteine in the treatment of acetaminophen overdose: Analysis of a national multicenter study (1976–1985) N Engl J Med.1988;3190:1557–1562. [PubMed]
14. Smilkstein MJ, Rumack BH. Elimination half-life as a predictor of acetaminophen-induced hepatotoxicity [abstract] Vet Hum Toxicol. 1994;36:337.
15. Dawson AH, Whyte IM. Therapeutic drug monitoring in drug overdose. Br J Clin Pharmacol.2001;52 (Suppl 1):97S–102S. [PMC free article] [PubMed]
16. Prescott LF, Roscoe P, Wright N, et al. Plasmaparacetamol half-life and hepatic necrosis in patients with paracetamol overdosage. Lancet. 1971;1:519–22. [PubMed]
17. Schiødt FV, Ott P, Christensen E, et al. The value of plasma acetaminophen half-life in antidote-treated acetaminophen overdosage. Clin Pharmacol Ther. 2002;71(4):221–5. [PubMed]


