| Author | Affiliation |
|---|---|
| Joel T. Levis, MD, PhD | Kaiser Santa Clara Medical Center, Department of Emergency Medicine, Santa Clara, CA Stanford-Kaiser Emergency Medicine Residency Program, Stanford, CA |
| Mucio C. Delgado, MD | Stanford-Kaiser Emergency Medicine Residency Program, Stanford, CA |
ABSTRACT
This case report describes a 54-year-old male on warfarin for atrial fibrillation who presented to the emergency department (ED) following a syncopal episode with persistent hypotension. The patient’s International Normalized Ratio (INR) returned elevated at 6.0, and a rapid bedside cardiac ultrasound revealed a large pericardial effusion consistent with cardiac tamponade. The anticoagulation was reversed and the patient underwent successful pericardiocentesis with removal of 1,100 mL of blood.
INTRODUCTION
Cardiac tamponade is a life-threatening condition in which the accumulation of fluid within the pericardial sac causes compression on the heart chambers and impairs their filling.1 Pericardial effusions resulting in cardiac tamponade can occur from a number of causes, including pericarditis, malignancy, acute myocardial infarction, end-stage renal disease, congestive heart failure, collagen vascular disease, and both viral and bacterial infection.2 Hemopericardium and resulting tamponade can result from any form of chest trauma, free wall rupture following myocardial infarction, retrograde bleeding into the pericardial sac following a type A aortic dissection, and as a complication of any invasive cardiac procedure.3–5 In this report, we describe a rare case of cardiac tamponade as a result of hemopericardium in a patient with a markedly elevated International Normalized Ratio (INR), which was rapidly diagnosed using bedside emergency department (ED) ultrasound.
CASE REPORT
A 54-year-old male with a medical history significant for diabetes, hypertension, and atrial fibrillation on warfarin presented to the ED following a syncopal episode, while having his blood drawn in an outpatient laboratory located within the hospital. The patient reported feeling light-headed and dizzy during the procedure, followed by a witnessed loss of consciousness occurring while seated and lasting for one minute. The patient did not fall nor sustain any trauma. Upon regaining consciousness, he continued to feel lightheaded and weak. He denied chest pain, shortness of breath, or palpitations prior to the event. He was transported from the laboratory to the ED by wheelchair, arriving approximately 15 minutes after the syncopal episode.
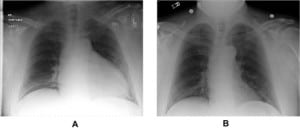
On physical examination, the patient appeared well-hydrated, awake and alert and in no acute distress. Vital signs revealed an oral temperature of 97.9° F, a pulse of 92 beats per minute, a blood pressure of 100/60 mm Hg, and respirations of 22 breaths per minute with an oxygen saturation of 97% on room air. Jugular venous distension was noted on neck examination. Examination of the chest did not reveal ecchymosis or evidence of trauma. The lungs were clear to auscultation, and cardiac exam revealed distant heart sounds. Peripheral pulses were palpable but weak. A peripheral intravenous line was placed and blood was sent for laboratory testing, which was significant for a creatinine of 2.1 mg/dL (normal range <1.3), lactic acid 2.7 mmol/L (normal range 0.7–2.1), hematocrit 36%, and INR 6.0 (therapeutic range 2.0–3.0). A 12-lead ECG demonstrated low-voltage most prominent in leads I, II, III, aVL, aVF, and V1 (Figure 1). A portable chest radiograph was remarkable for cardiomegaly (Figure 2, panel A), compared to a portable chest radiograph obtained from the same patient four months earlier during an ED evaluation for chest pain (Figure 2, panel B). The emergency physician (EP) performed a bedside cardiac ultrasound, which revealed a large pericardial effusion (Figure 3; echo-free space >20 mm, corresponding to >700 mL effusion).


While in the ED, the patient was given one liter normal saline intravenously, vitamin K 10 mg subcutaneously and an infusion of 2 units of fresh frozen plasma were administered to reverse the coagulopathy. A portable echocardiogram was performed, which again demonstrated a pericardial effusion along with right ventricular collapse, indicative of cardiac tamponade. The patient was admitted to the Intensive Care Unit (ICU) and stabilized, and on the following day the cardiologist performed a pericardiocentesis in the cardiac catheterization laboratory. Pericardiocentesis resulted in the removal of a 1,100 mL of bloody fluid from the pericardium and marked improvement in the patient’s hemodynamic status. Pericardial fluid analysis showed no evidence of infection or malignancy. The patient was discharged home on hospital day #8, with instructions to discontinue warfarin therapy. Repeat echocardiograms at discharge and three weeks later both demonstrated a very small pericardial effusion without signs of tamponade.
DISCUSSION
In this report, we describe a rare case of cardiac tamponade caused by hemopericardium in a patient with a markedly elevated INR, presenting to the ED as syncope. Hong et al.6described the case of a 70-year-old male on warfarin for mitral valve replacement presenting to the ED with cardiac tamponade. The patient’s INR was 7.5, and urgent pericardiocentesis and pericardiotomy resulted in the drainage of 1,300 ml of pericardial blood. Katis7 reported a case of hemopericardium in a patient on warfarin therapy for pulmonary embolus, with the hemopericardium initially diagnosed by computed tomography of the thorax. In this case, the patient’s initial INR was 3.5, and the patient was hemodynamically stable on presentation (blood pressure 150/80 mm Hg) with a bedside echocardiogram later confirming presence of a large pericardial effusion and right atrial inversion with right ventricular diastolic collapse (suggestive of cardiac tamponade). Finally, Lee et al.8 described the case of a 67-year-old male receiving warfarin therapy for vertebral basilar insufficiency with hemopericardium, an elevated prothrombin time and transthoracic echocardiographic-evidence of cardiac tamponade. These cases demonstrate that over-anticoagulation with warfarin may contribute to certain complications, including hemopericardium. To our knowledge, our case is the first report of cardiac tamponade from hemopericardium in a patient on warfarin for atrial fibrillation without a history of cardiac surgery, with the resulting pericardial effusion initially diagnosed by bedside ED ultrasound.
Cardiac tamponade is a true emergency that occurs when accumulation of fluid within the pericardium causes intrapericardial pressure to exceed cardiac chamber diastolic pressure, preventing cardiac filling.9 Three factors determine the acuity of the clinical presentation: volume of fluid, rate at which the fluid accumulates, and pericardial compliance. If the fluid accumulates rapidly or if the pericardium is pathologically stiff, then relatively small amounts of fluid can result in marked elevations in pressure.9Rapidly evolving hemopericardium (200 to 300 ml) is more likely to cause death from cardiac tamponade than slowly evolving pericardial fluid accumulation (500 to 2000 ml), the latter allowing for accommodation of greater volumes due to gradual distension of the pericardial sac.10 The normal volume of pericardial fluid (30 to 50 ml) reflects a balance between production and reabsorption.10
Symptoms of tamponade include but are not limited to dyspnea, tachypnea, and fatigue, while common signs include tachycardia, jugular venous distension, a quiet precordium, hypotension, and pulsus paradoxus (inspiratory drop in systolic blood pressure of 10% or 10 mm Hg).9,11 Although a pericardial rub typically disappears when an effusion develops, a rub caused by pericardial-pleural friction may still be present and is typically heard best on inspiration.9 The Kussmal sign, a paradoxical rise in jugular venous pulse with inspiration, may also be seen but is not specific for tamponade, as it is also present in cases of constrictive pericarditis, restrictive cardiomyopathy, and right ventricular infarction.11 A relatively easy way to detect pulsus paradoxus at the bedside is to see if the pulse oximeter wave amplitude decreases with inspiration.12
Chest radiographs and ECGs cannot be relied upon to make the diagnosis of cardiac tamponade, as findings are not specific or may not even exist.13 Chest radiograph may demonstrate cardiomegaly or a cardiac silhouette in the shape of a water bottle. Electrocardiograms in cardiac tamponade may show low-amplitude QRS complexes signifying low voltage, or in up to 10–20% of cases may reveal the more specific finding of electrical alternans caused by “swinging” of the oscillating heart in the buoyant pericardial sac.13
Echocardiography is the primary diagnostic method for initial detection of pericardial effusion, and can be rapidly carried out at the bedside by EPs.14,15 Pericardial fluid first accumulates posterior to the heart, when the patient is examined in the supine position.13As the effusion increases, it extends laterally and with large effusions the echo-free space expands to surround the entire heart. The size of the effusion may be graded as small (echo-free space in diastole <10 mm, corresponding to approximately 300 ml), moderate (10–20 mm, corresponding to 500 ml), and large (>20 mm, corresponding to >700 ml).16 When the ability of the pericardium to stretch is exceeded by rapid or massive accumulation of fluid, any additional fluid causes the pressure within the pericardial sac to increase. When the increasing intrapericardial pressure exceeds the intracardiac pressure, the positive transmural pressure gradient compresses the adjacent cardiac chamber or chambers.14 Right atrial inversion (during ventricular systole, while the atrium is relaxed) is usually an early sign of compression, followed by diastolic compression of the right ventricular outflow tract.
There is no effective medical therapy for cardiac tamponade; however, intravenous fluids may be of transient benefit if the patient is hypovolemic.9 Inotropic agents do not add to the intense endogenous adrenergic stimulation since the heart rate and cardiac contractility will already be at a maximum.9 If the patient is unstable, immediate relief of tamponade by percutaneous subxiphoid aspiration is required. This procedure, which has been studied using a percutaneous pericardial catheter drainage (PCD) technique in the ED for patients with nontraumatic hemopericardium,17 uses an 8-cm, 18-gauge needle inserted between the xiphoid process and the left costal margin, aimed toward the left shoulder under ultrasound guidance. When the pericardial sac is entered a guide wire is advanced through the needle, followed by an 8.5 French pericardial catheter.17 In hemodynamically-stable patients, echocardiography-guided pericardiocentesis or pericardiocentesis performed in the cardiac catheterization lab under fluoroscopy is the treatment of choice.9,11 A catheter is usually left in the pericardium to continue draining any recurrent effusion. Surgical drainage employing either a subxiphoid window or an open thoracotomy is also an option.
Vitamin K and fresh frozen plasma are useful agents in achieving reversal of a supratherapeutic INR in patients who have active bleeding or require invasive procedures. The use of vitamin K in patients with warfarin over-anticoagulation lowers excessively elevated INR faster than withholding warfarin alone. As vitamin K administration via the intravenous route may be complicated by anaphylactoid reactions, and via the subcutaneous route by cutaneous reactions, oral administration is preferred.18 A dose of 1–2.5 mg of oral vitamin K reduces the range of INR from 5.0–9.0 to 2.0–5.0 within 24–48 hours, while for an INR>10.0, a dose of 5 mg may be more appropriate.18 The usual dose of fresh frozen plasma for reversal of an elevated INR is 15 mL/kg (approximately 3–4 units of plasma in the average-sized adult).19 Potential drawbacks to the use of fresh-frozen plasma include prolonged period of time to thaw and administer, increased risk of volume overload, and a potential carrier of infective agents.19
One complicated facet of the management of cardiac tamponade involves the timing of pericardiocentesis.20 In our case, the patient was stable enough to allow for reversal of the coagulopathy with fresh frozen plasma and vitamin K prior to pericardiocentesis. But if the patient had decompensated more quickly in the ED, an emergent pericardiocentesis may have been necessary, with the associated bleeding risk due to the markedly elevated INR. Although only anecdotal reports exist regarding the use of recombinant factor VII and prothrombin complex concentrates (PCC) to rapidly reverse coagulopathy in the setting of life-threatening hemorrhage, the use of these novel agents could have been considered in the scenario described above.21,22
Footnotes
Supervising Section Editor: David E. Slattery, MD
Submission history: Submitted May 09, 2008; Revision Received July19, 2008; Accepted July 28, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Joel T. Levis, MD, PhD, Department of Emergency Medicine, Kaiser Santa Clara Medical Center, 700 Lawrence Expressway, Santa Clara, CA 95051
Email: joel.levis@kp.org.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Spodick DH. Current concepts: Acute cardiac tamponade. N Engl J Med.2003;349:684–90. [PubMed]
2. Roy CL, Minor MA, Brookhart MA, et al. Does this patient with a pericardial effusion have cardiac tamponade? JAMA. 2007;297:1810–18. [PubMed]
3. Krejci CS, Blackmore CC, Nathens A. Hemopericardium: An emergent finding in a case of blunt cardiac injury. Amer J Roentgen. 2000;175:250.
4. Pretre R, Chilcott M. Current concepts: Blunt trauma to the heart and great vessels. N Engl J Med. 1997;336:626–32. [PubMed]
5. LeWinter MM. Chapter 70 – Pericardial disease. In: Libby P, Bonow RO, Mann DL, editors. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 8th ed. Philadelphia PA: Saunders Elsevier; 2008. p. 1851.
6. Hong YC, Chen YG, Hsiao CT, et al. Cardiac tamponade secondary to haemopericardium in a patient on warfarin. Emerg Med J. 2007;24:679–80.[PMC free article] [PubMed]
7. Katis PG. Atraumatic hemopericardium in a patient receiving warfarin therapy for a pulmonary embolus. Can J Emerg Med. 2005;7:168–70.
8. Lee KS, Marwick T. Hemopericardium and cardiac tamponade associated with warfarin therapy. Cleve Clin J Med. 1993;60:336–8. [PubMed]
9. Shiber JR. Purulent pericarditis: Acute infections and chronic complications. Hosp Physician. 2008;44:9–18.
10. Swaminathan A, Kandaswamy K, Powari M, et al. Dying from cardiac tamponade.World J Emerg Surg. 2007;2:22. [PMC free article] [PubMed]
11. Force T. Chapter 85 – The cancer patient and cardiovascular disease. In: Libby P, Bonow RO, Mann DL, editors. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 8th ed. Philadelphia PA: Saunders Elsevier; 2008. p. 2105.
12. Tamburro R, Ring J, Womback K. Detection of pulsus paradoxus associated with large pericardial effusions in pediatric patients by analysis of the pulse-oximetry waveform.Pediatrics. 2002;109:673–77. [PubMed]
13. Ariyarajah V, Spodick DH. Cardiac tamponade revisited: A postmortem look at a cautionary case. Tex Heart Inst J. 2007;34:347–51. [PMC free article] [PubMed]
14. Wann S, Passen E. Echocardiography in pericardial disease. J Am Soc Echocardiogr.2007;21:7–13. [PubMed]
15. Mandavia DP, Hoffner RJ, Mahaney K, et al. Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001;38:377–82. [PubMed]
16. Pepi M, Muratori M. Echocardiography in the diagnosis and management of pericardial disease. J Cardiovasc Med. 2006;7:533–44.
17. Wang R-F, Chao C-C, Wang T-L, et al. The effect of different relieving methods on the outcome of out-of-hospital cardiac arrest patients with nontraumatic hemopericardium in the ED. Am J Emerg Med. 2008;26:425–32. [PubMed]
18. Hanslik T, Prinseau J. The use of vitamin K in patients on anticoagulation therapy: a practical guide. Am J Cardiovasc Drugs. 2004;4:43–55. [PubMed]
19. Dentali F, Ageno W, Crowther M. Treatment of coumarin-associated coagulopathy: a systemic review and proposed treatment algorithms. J Thromb Haemost. 2006;4:1853–63. [PubMed]
20. Cooper JP, Oliver RM, Currie P, et al. How do the clinical findings in patients with pericardial effusion influence the success of aspiration? Heart. 1995;73:351–54.
21. Leissinger CA, Blatt PM, Hoots WK, et al. Role of prothrombin complex concentrates in reversing warfarin anticoagulation: A review of the literature. Amer J Hematol.2007;83:137–43. [PubMed]
22. Ingerslev J, Vanek T, Culic S. Use of recombinant factor VIIa for emergency reversal of anticoagulation. J Postgrad Med. 2007;53:17–22. [PubMed]


