| Author | Affiliation |
|---|---|
| Robinson M. Ferre, MD | Vanderbilt University Medical Center, Department of Emergency Medicine, Nashville, Tennessee |
| Mark Mercier, MD | Palmetto Health Baptist, Department of Emergency Medicine, Columbia, South Carolina |
Introduction
Methods
Results
Discussion
Limitations
Conclusions
ABSTRACT
Introduction
Real-time ultrasound guidance is considered to be the standard of care for central venous access for non-emergent central lines. However, adoption has been slow, in part because of the technical challenges and time required to become proficient. The AxoTrack® system (Soma Access Systems, Greenville, SC) is a novel ultrasound guidance system recently cleared for human use by the United States Food and Drug Administration (FDA).
Methods
After FDA clearance, the AxoTrack® system was released to three hospitals in the United States. Physicians and nurse practitioners who work in the intensive care unit or emergency department and who place central venous catheters were trained to use the AxoTrack® system. De-identified data about central lines placed in living patients with the AxoTrack® system was prospectively gathered at each of the three hospitals for quality assurance purposes. After institutional review board approval, we consolidated the data for the first five months of use for retrospective review.
Results
The AxoTrack® system was used by 22 different health care providers in 50 consecutive patients undergoing central venous cannulation (CVC) from September 2012 to February 2013. All patients had successful CVC with the guidance of the AxoTrack® system. All but one patient (98%) had successful cannulation on the first site attempted. There were no reported complications, including pneumothorax, hemothorax, arterial puncture or arterial cannulation.
Conclusion
The AxoTrack® system was a safe and effective means of CVC that was used by a variety of health care practitioners.
INTRODUCTION
The use of catheters to access the central venous system is a well-established and important method for administering life-saving drugs and fluids as well as monitoring patient hemodynamics. Since 1984, research has shown that using ultrasound (US) to assist with central venous cannulation (CVC) improves success rates and lowers complications.1 Multiple studies have confirmed these findings and demonstrated that ultrasound guided CVC increases success rate, lowers complications and reduces costs.2–4 This evidence has led several large medical organizations and government agencies to recommend the use of ultrasound guidance for CVC.5–9 Despite the evidence and recommendations, surveys have found that the availability of ultrasound in community emergency departments (ED) is less than 50% 10–11 and in those hospitals where access to ultrasound in the ED is higher, almost half of physicians felt they had inadequate training and a quarter of physicians indicated that they felt “uncomfortable” or “very uncomfortable” using ultrasound for CVC.12
To make US guided CVC easier, many different ultrasound systems have been proposed. One such system, the AxoTrack® System, was developed by Soma Access Systems (Greenville, SC) to simplify ultrasound guided CVC. The AxoTrack® system is an ultrasound probe with a built-in needle guidance system that incorporates technology to give the operator real-time information not only on the direction of the needle but also actual knowledge of the needle location at all times throughout the procedure. The purpose of this study is to describe the safety and efficacy of the AxoTrack® system in the first 50 subjects following FDA clearance in February 2012.
METHODS
The AxoTrack® System
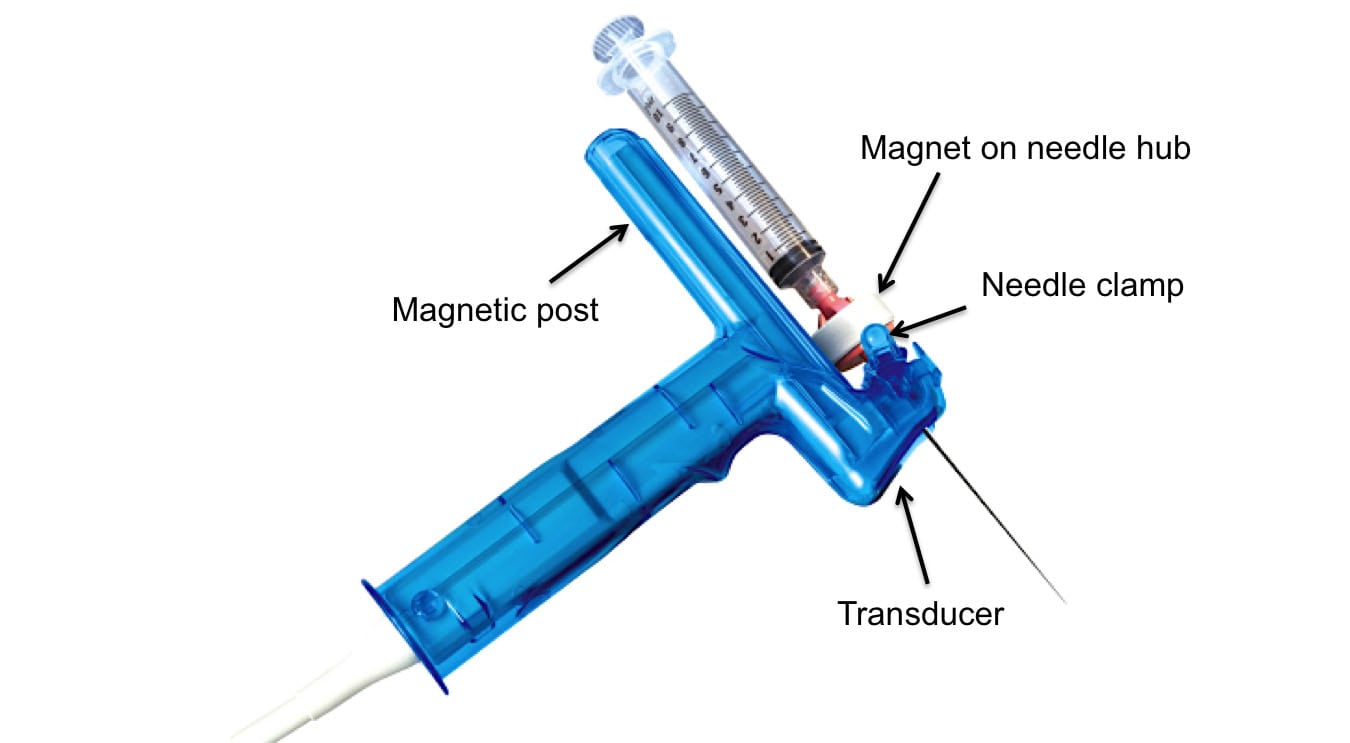
The AxoTrack® system includes an ultrasound probe with a needle guide that extends through the body of the ultrasound probe making the path of the needle coincident and coplanar within the ultrasound beam (see Figure 1). Additionally, the probe houses a separate set of magnetic sensors that monitor the depth of the needle and projects on the ultrasound system monitor a real-time, virtual image of the needle as it moves toward the intended central vein. The procedure is performed by first aligning the on-screen target line (which corresponds with the path the needle will take when inserted) with the intended central vein that is displayed on the monitor. Once the target line and intended central vein are aligned, the needle is inserted through the needle guide in the probe and advanced while observing its progress until the needle enters the intended central vein. The AxoTrack®system also incorporates a needle clamping mechanism that can be used to stabilize the needle once it has reached the intended central vein. This mechanism allows the operator to leave the probe on the body and continue scanning during guide-wire passage, allowing for real-time confirmation of guide-wire positioning.
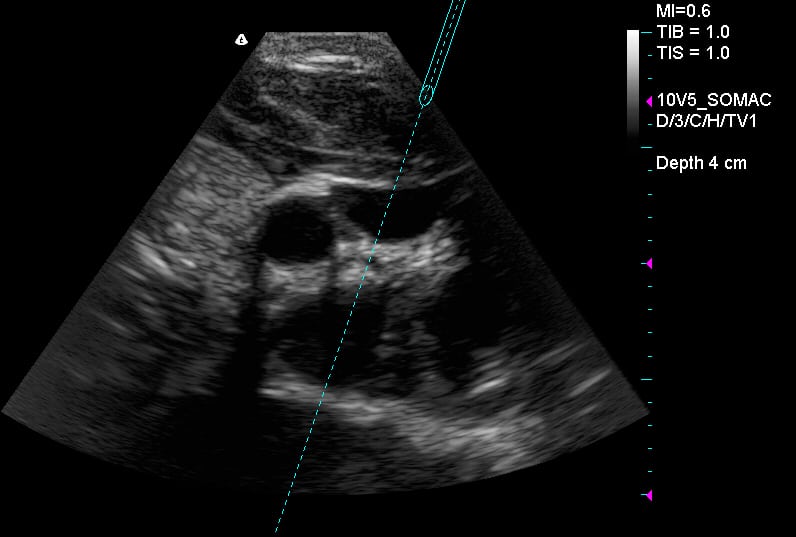
Figure 1
Screenshot of AxoTrack® System during internal jugular vein cannulation.
CA, carotid artery; IJV, internal jugular vein
The AxoTrack® system is incorporated onto the FUJIFILM SonoSite M-turbo (Bothell, WA) and Terason t3000 (Burlington, MA) platforms. Both machines were used in this study at each study location.
Training
The AxoTrack® system was cleared by the FDA for human use in February, 2012. Since that time, three systems were made available for clinical use by Soma Access Systems. These systems were placed at Vanderbilt University Medical Center, Nashville, TN, Palmetto Health Richland, Columbia, SC and Palmetto Health Baptist, Columbia, SC. Resident and attending physicians as well as nurse practitioners who worked in the intensive care unit (ICU) or ED and who routinely placed central lines were trained how to use the system. Training included a standard 20-minute lecture and orientation to the system. Following this lecture, trainees were given hands-on instruction with the use of a Blue Phantom (Bothell, WA) head and neck ultrasound phantom that featured simulated anatomy of the Internal Jugular, Subclavian and Axillary veins. They were required to successfully place the needle in at least the Internal Jugular or Subclavian vein of the phantom during the hands on training.
Patient Selection
Patients in whom the AxoTrack® system was used for CVC were selected on a convenience basis. Inclusion criteria included patients at least 18 years of age who needed CVC and where no clinical contraindications existed, as determined by the treating physician or nurse practitioner. There were no explicit exclusion criteria for the study.
The study author (RMF) and one other emergency physician placed their first CVC with the AxoTrack® system without supervision. For the remaining proceduralists, their first CVC with the AxoTrack® system occurred when a physician or nurse practitioner who had previously been through the didactic and hands-on training process contacted an attending physician who had previously performed CVC with the AxoTrack® system. That attending physician then supervised this first line placed by the novice user. After the first successful CVC, subsequent CVCs did not require supervision by an experienced AxoTrack® system user. Because the ultrasound machine with the dedicated AxoTrack® system was in a secure location, that could only be accessed by one designated physician for each of the three locations, standardized data was collected by each of these designated physicians with access to the machine immediately following the procedure. This data was recorded in a Microsoft Excel worksheet (Redmond, WA). The anatomic site of CVC was according to the preference of the physician or nurse practitioner performing the procedure.
Study Definitions
Prior to data analysis, we defined a priori procedural success and procedural complication. We defined “procedural success” as the successful insertion of a central venous catheter in the desired central vein using the AxoTrack® system. We defined “procedural complication” as any complication entered into the database that was immediately known to have occurred during the procedure or detected by chest radiography following the procedure. Specifically, we determined if any of the following complications occurred: pneumothorax, hemothorax, arterial cannulation, hematoma formation at the insertion site, and location of the distal catheter tip in a location other than the distal superior vena cava or right atrium of the heart. We did not record any complications that occurred beyond the performance of chest radiography such as infections or skin irritation.
Data Collection
Following local institutional review committee approval at each of the participating institutions, a unique database was created using REDCap electronic data capture tools hosted at VUMC.13 REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing: 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.13 One physician (RMF) consolidated the data that had been collected from each institution into a REDCap database form. Data included the following: the type of practitioner and their current level of training, if the procedure was the first time they had used the device clinically, success or failure of the procedure, procedural site, and complications at the time of the procedure or detected by chest radiography following CVC.
RESULTS
The AxoTrack® system was used by 22 different health practitioners at all 3 institutions to obtain central venous access in fifty subjects from September 2012 to February 2013. Subjects included 37 (74%) patients in the ED and 13 (26%) patients in the ICU. There were no lines placed during cardiac arrest, however, all lines were placed on an urgent or semi-emergent basis. The most common indications for central venous catheter insertion were: sepsis, gastrointestinal bleeding, respiratory failure and end-stage renal disease with need for emergent dialysis.
System users included 4 attending physicians, 16 resident physicians, 1 nurse practitioner and one surgical/critical care fellow. All 4 attending physicians were emergency physicians. Of the 16 residents, all were emergency medicine residents and included two interns, five in their second year of residency training and nine in their third year of residency training. The 1 fellow was a surgeon in a surgical/critical care fellowship. The nurse practitioner worked in the medical ICU. All proceduralists had inserted more than five CVCs prior to using the AxoTrack® system. Of the 50 lines placed, 20 (40%) were the very first lines placed by the operator using the system. All 50 subjects had successful CVC using the AxoTrack® System. Forty-nine (98%) subjects had successful CVC at the first anatomic site attempted. There were no procedural complications recorded at the time of the procedure or detected by chest radiography immediately following the procedure. The table lists the number of successful CVC by anatomic site.
One patient had failure at the first site attempted (infraclavicular approach to the Subclavian vein). The Internal Jugular vein in this patient was completely collapsed when visualized with ultrasound and no attempt was made at this site. The second site attempted (a supraclavicular approach to the Subclavian vein) was successful after the first attempt.
DISCUSSION
With the introduction of ultrasound guided CVC, there has been a marked improvement in the first-pass success rate and an overall decrease in the rate of complications.1–4 Despite this improvement, complications still occur, although at a much lower rate than the traditional landmark-only based approach.1–4, 14 Despite these studies and the endorsement of many professional organizations, the widespread use and adoption of ultrasound guided CVC insertion is low,15–18,25 with one recent study reporting as few as 13% of anesthesiologists routinely performing CVC with US guidance.15 The routine utilization of ultrasound for central venous access by emergency physicians is unknown since ultrasound guided CVC training has become mandatory in residency, however, two small regional surveys have shown acceptance rates as high as 97% among residents currently in training and 78% for those beyond residency.26–27
Several different ultrasound systems have been proposed or designed to improve needle tip localization, improve the human interface and simplify the insertion process in an attempt to continue to improve CVC, reduce insertion errors, and make it easier for new users. In addition to lack of appropriate ultrasound training, one possible reason for the lack of use of ultrasound for CVC is that complications, while reduced, continue to occur even when ultrasound is used.19–21 A video review of accidental carotid artery cannulations during real-time US guidance found that a short axis approach, where it is difficult to precisely identify the location of the tip of the needle during cannulation, was a common factor identified in all cases of accidental arterial cannulation.21
The AxoTrack® system offers 2 unique advantages that potentially can help improve the process of CVC. First, like many needle guidance systems, it overlays information about the potential path (trajectory) of the needle on top of the ultrasound image. Second, unique to the AxoTrack® system, it uses Hall effect technology that supplies real-time information about the location of the needle tip in relation to the probe (Figure 1 and 2). When using the system, the operator not only knows the trajectory of the needle, but also knows where the tip of the needle is at all times without having to move or adjust the needle or probe. In theory, these two properties of the AxoTrack® system should improve successful insertion rates, reduce complications even further and make it easier for novice users of ultrasound technology to incorporate ultrasound guided CVC into their practice. While small, our retrospective review of QA data provides support for the theoretical basis behind the technologic advances of the AxoTrack® system.
During our study, we also found that the Subclavian vein was commonly used for CVC with the AxoTrack® system. While ultrasound guided Femoral and Internal Jugular venous access has relatively straightforward landmarks, ultrasound-guided Subclavian venous access is much more difficult due to the clavicle that directly overlies the Subclavian vein making it difficult to both visualize with ultrasound and guide the needle into the vein. Several studies have shown ultrasound guided CVC of the Subclavian vein to be a plausible technique.22–24 Fragou et al,22 performed a study comparing an ultrasound guided infraclavicular approach to the Subclavian vein with the standard landmark technique and showed ultrasound guidance to be superior in procedural success and complication rates. However, while there was greater success with ultrasound guidance, the proceduralists involved in the study rated this approach an 8 on a 10-point Lickert scale for difficulty, where 0 was “simple” and 10 was “complex.” Interestingly, we found that the small footprint of the AxoTrack® probe makes an infraclavicular or supraclavicular approach to the Subclavian vein relatively straightforward. While we did not ask the proceduralists to rate how difficult they thought the procedure was from a given approach, it is interesting to note that 40% of all lines placed in our study were Subclavian lines, with the supraclavicular approach being used almost twice as much as the infraclavicular approach.
LIMITATIONS
This retrospective review has several limitations. It is important to note that first-time users received direct instruction during the procedure by a more experienced operator. While this may occur in residency training, it is difficult to replicate with physicians who are beyond residency training. In addition, all operators in the study had at least some prior experience with ultrasound guided CVC. A practicing physician without experience using ultrasound may have a more difficult time using the system.
Our data was limited to only a few data points. This was because the original QA data set was limited in scope and did not include any protected health information. This limited our ability to describe the subjects who received CVC using the AxoTrack®system. Furthermore, the retrospective nature from data collected during a very short and finite time frame limited our ability to assess for other complications that may have been a direct result of the procedure but delayed in their presentation such as infection, pain or hematoma at the insertion site. To our knowledge, this did not occur, but it is important to note nonetheless. An ongoing prospective observational study is currently taking place that will better describe any delayed complications and more details about the CVC procedure.
CONCLUSIONS
The AxoTrack® system is a safe and effective means of guiding CVC in patients in the ICU or ED. Furthermore, several different health care practitioners, with limited training, used the AxoTrack® system effectively for CVC.
Study Support
The ultrasound machines and probe covers for this study were provided at no cost by Soma Access Systems and FUJIFILM SonoSite to the study sites. No additional funding or support was provided. The company had no role in design, data analysis or drawing conclusions for the study.
Table. Number and percentage of successful central venous catheterizations by anatomic site and approach.
| Anatomic site | Successful line placement |
|---|---|
| Right internal jugular vein | 20 (40%) |
| Right subclavian (supraclavicular approach) | 12 (24%) |
| Right femoral vein | 6 (12%) |
| Left internal jugular vein | 4 (8%) |
| Left subclavian vein (infraclavicular approach) | 4 (8%) |
| Right subclavian vein (infraclavicular approach) | 3 (6%) |
| Left subclavian vein (supraclavicular approach) | 1 (2%) |
| Left femoral vein | 0 |
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Robinson M. Ferre, MD. Vanderbilt University, Department of Emergency Medicine, 13133 21st Ave South, 703, Titles, Address. Email: robinson.ferre@vanderbilt.edu. 7 / 2014; 15:536 – 540
Submission history: Revision received April 1, 2013; Submitted October 15, 2013; Accepted January 27, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The device used in this project was provided by AxoTrack®, along with an unrestricted education grant. The device manufacturer had no role in study design, data analysis, preparation or review of the manuscript.
REFERENCES
1 Legler D, Nugent M Doppler localization of the internal jugular vein facilitates central venous cannulation. Anesthesiology. 1984; 60:481-482
2 Hind D, Calvert N, McWilliams R Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003; 16;327:361
3 Randolph AG, Cook DJ, Gonzales CA Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996; 24:2053-2058
4 Keenan Sean P Use of ultrasound to place central lines. J Crit Care. 2002; 17:126-137
5 American College of Emergency Physicians policy statement: emergency ultrasound guidelines. American College of Emergency Physicians Web site. ;
6 Shojania K, Duncan B, McDonald K Making healthcare safer: a critical analysis of patient safety practices. Agency for Healthcare Research and Quality Web site. ;
7 Final appraisal determination: ultrasound locating devices for placing central venous catheters. National Institute for Health and Clinical Excellence Web site. ;
8 Statement on recommendations for uniform use of real-time ultrasound guidance for placement of central venous catheters. American College of Surgeons Web site. ;
9 Rothschild JM Ultrasound guidance of central vein catheterization. On Making Health Care Safer: A Critical Analysis of Patient Safety Practices. 2001; Chapter 21:245-255
10 Stein JC, River G, Kalika I A survey of bedside ultrasound use by emergency physicians in California. J Ultrasound Med. 2009; 28:757-763
11 Moore C, Molina A, Lin H Ultrasonography in community emergency departments in the United States: access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006; 47:147-153
12 Barklund B, Hopkins E, Kendall J Ultrasound Guidance for Central Venous Access by Emergency Physicians in Colorado. West J Emerg Med. 2012; 13:320-325
13 Paul AH, Robert T, Robert T Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377-381
14 Blaivas M Video analysis of accidental arterial cannulation with dynamic ultrasound guidance for central venous access. J Ultrasound Med. 2009; 28:1239-1244
15 Schummer W, Sakka SG, Huttemann E Ultrasound guidance for placement control of central venous catheterization. Survey of 802 anesthesia departments for 2007 in Germany. Anaesthetist. 2009; 58:677-685
16 Tovey G, Stokes M A survey of the use of 2D ultrasound guidance for insertion of central venous catheters by UK consultant paediatric anaesthetists. Eur. J. Anaesth. 2007; 24:71-75
17 Bailey PL, Glance LG, Eaton MP A survey of the use of ultrasound during central venous catheterization. Anesth. Analg. 2007; 104:491-497
18 McGratten T, Duffty J, Green JS A survey of the use of ultrasound guidance in internal jugular venous cannulation. Anaesthesia. 2008; 63:1222-1225
19 Parsons AJ, Alfa J Carotid dissection: a complication of internal jugular vein cannulation with the use of ultrasound. Anesth Analg. 2009; 109:135-136
20 Ezaru CS, Manglione MP, Oravitz TM Eliminating arterial injury during central venous catheterization using manometry. Anesth Analg. 2009; 109:130-134
21 Blaivas M Video analysis of accidental arterial cannulation with dynamic ultrasound guidance for central venous access. J Ultrasound Med. 2009; 28:1239-1244
22 Fragou M, Gravvanis A, Dimitriou V Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: A prospective randomized study. Crit Care Med. 2011; 39:1607-1612
23 Shah A, Smith A, Panchatsharam S Ultrasound-guided subclavian venous catheterisation – is this the way forward? A narrative review. Int J Clin Pract. 2013; 67:726-732
24 Byon HJ, Lee GW, Lee JH Comparison between ultrasound-guided supraclavicular and infraclavicular approaches for subclavian venous catheterization in children–a randomized trial. Br J Anaesth. 2013; 111:788-792
25 Sheridan RL, Neely AN, Castillo MA A survey of invasive catheter practices in U.S. burn centers. J Burn Care Res. 2012; 33:741-746
26 Nomura JT, Sierzenski PR, Nace JE Cross sectional survey of ultrasound use for central venous catheter insertion among resident physicians. Del Med J. 2008; 80:255-259
27 Backlund BH, Hopkins E, Kendall JL Ultrasound guidance for central venous access by emergency physicians in Colorado. West J Emerg Med. 2012; 13:320-325