| Author | Affiliation |
|---|---|
| Jeremy N. Johnson, DO | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis, WA |
| Robert Jones, MD | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis, WA |
| Brandon K. Wills, DO, MS | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis, WA |
A 23-year-old male presented to the emergency department (ED) with sore throat, chest pain and shortness of breath that started two days prior to his arrival and gradually increased in severity. Other symptoms included pleuritic chest pain, back pain, dysphagia, odynophagia and general air hunger. The patient denied any history of trauma or similar symptoms.
Spontaneous pneumomediastinum (SPM) is an uncommon condition presenting in approximately one in 1,000 to one in 40,000 ED referrals.1,2,3 Young patients with SPM typically present with a history of asthma or recent inhalation of cocaine, methamphetamine, ecstasy, marijuana or hydrocarbons.4,5,6,7 Other causes include barotrauma in asthmatics and COPD patients, rapid ascent in scuba divers, valsalva maneuvers, vomiting, infections, blast injuries and iatrogenic injuries from endoscopy or surgery.8 The most common presentation is nonspecific pleuritic chest pain with dyspnea. Potential life-threatening etiologies include esophageal rupture and tension pneumothorax, but these are historically evident at presentation.9–12 Because a subset of patients with this finding have significant pathology, extensive workups are often necessary. Treatment is generally limited to observation, with the SPM typically reabsorbing over a period of one to two weeks without intervention and only rare recurrence.13

Lateral soft tissue neck illustrating retropharyngeal free air.
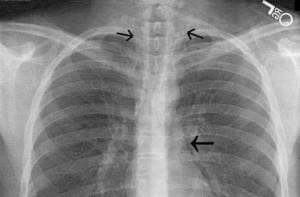
PA CXR showing pneumopericardium and free air in cervical soft tissues

CT upper thorax with pneumomediastinum
Footnotes
Supervising Section Editor: Jeffrey Sankoff, MD
Submission history: Submitted October 13, 2007; Revision Received March 25, 2008; Accepted March 27, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jeremy N. Johnson, DO. Department of Emergency Medicine, Madigan Army Medical Center, Fort Lewis, WA
Email: jeremy.n.johnson@amedd.army.mil
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Newcomb AE. Chest. 2005;128:3298–3302. [PubMed]
2. McMahon DJ. Spontaneous pneumomediastinum. Am J Surg. 1976;131:550–551.[PubMed]
3. Bodey GP. Medical Mediastinal Emphysema. Ann Intern Med. 1961;54:46–56.
4. Harris R, Joseph A. Spontaneous pneumomediastinum: ecstasy; a hard pill to swallow.Aust N Z J Med. 2000;30:401–403. [PubMed]
5. Mir B, Galvete V, Plaza V, et al. Spontaneous pneumomediastinum after cocaine inhalation. Respiration. 1986;50:230–232. [PubMed]
6. Millar N, Spiakeman P, Hepper N. Pneumomediastinum resulting from performing valsalva maneuvers during marijuana smoking. Chest. 1972;62:233–234. [PubMed]
7. Badaoui R, El Kettani C, Fikri M, et al. Spontaneous cervical and mediastinal air emphysema after ecstasy abuse. Anesth Analg. 2002;95:1123. [PubMed]
8. Bartelmaos T, Blanc R, Claviere GD, Benhamou D. Delayed pneumomediastinum and pneumothorax complicating laparoscopic extraperitoneal inguinal hernia repair. J Clin Anesth. 2005;17:209–212. [PubMed]
9. Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp.1939;64:1–21.
10. McMahon DJ. Spontaneous pneumomediastinum. Am J Surg. 1976;131:550–551.[PubMed]
11. Henderson JAM, Peloquin AJM. Boerhaave revisited: spontaneous esophageal perforation as a diagnostic masquerader. Am J Med. 1989;86:559–567. [PubMed]
12. Munsell WP. Pneumomediastinum: a report of 28 cases and review of the literature.JAMA. 1967;202:129–133. [PubMed]
13. Lee CC, Chen TJ, Wu YH, Tsai KC, Yuan A. Spontaneous retropharyngeal emphysema and pneumomediastinum presented with signs of acute upper airway obstruction. Am J Emerg Med. 2005;23:402–404. [PubMed]


