| Author | Affiliation |
|---|---|
| M. Kit Delgado, MD, MS | Stanford University, Division of Emergency Medicine, Stanford, California |
| Lesley J. Meng, HBA, BMSc | Columbia University, Mailman School of Public Health, New York City, New York |
| Mary P. Mercer, MD, MPH | University of California San Francisco, San Francisco General Hospital, San Francisco, California |
| Jesse M. Pines, MD, MBA, MSCE | George Washington University, Department of Emergency Medicine and Health Policy, Washington, DC |
| Douglas K. Owens, MD, MS | Stanford University, Center for Health Policy/Center for Primary Care and Outcomes Research, Stanford, California |
| Gregory S. Zaric, PhD | University of Western Ontario, Department of Epidemiology and Biostatistics and the Richard Ivey School of Business, London, Ontario, Canada |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Abstract
Introduction:
Optimal solutions for reducing diversion without worsening emergency department (ED) crowding are unclear. We performed a systematic review of published simulation studies to identify: 1) the tradeoff between ambulance diversion and ED wait times; 2) the predicted impact of patient flow interventions on reducing diversion; and 3) the optimal regional strategy for reducing diversion.
Methods:
Data Sources: Systematic review of articles using MEDLINE, Inspec, Scopus. Additional studies identified through bibliography review, Google Scholar, and scientific conference proceedings. Study Selection: Only simulations modeling ambulance diversion as a result of ED crowding or inpatient capacity problems were included. Data extraction: Independent extraction by two authors using predefined data fields.
Results:
We identified 5,116 potentially relevant records; 10 studies met inclusion criteria. In models that quantified the relationship between ED throughput times and diversion, diversion was found to only minimally improve ED waiting room times. Adding holding units for inpatient boarders and ED-based fast tracks, improving lab turnaround times, and smoothing elective surgery caseloads were found to reduce diversion considerably. While two models found a cooperative agreement between hospitals is necessary to prevent defensive diversion behavior by a hospital when a nearby hospital goes on diversion, one model found there may be more optimal solutions for reducing region wide wait times than a regional ban on diversion.
Conclusion:
Smoothing elective surgery caseloads, adding ED fast tracks as well as holding units for inpatient boarders, improving ED lab turnaround times, and implementing regional cooperative agreements among hospitals are promising avenues for reducing diversion.
INTRODUCTION
When emergency departments (ED) become crowded, incoming ambulances are sometimes diverted to other hospitals in an attempt to mitigate crowding. In 2003 45% of United States EDs reported being “on diversion” at some point within the year.1 Ambulance diversion has been used since the early 1990s.2,3 It has been linked to several negative consequences, such as prolonged transport times, delays in care, increased mortality, and lower hospital revenue.4–12 In response, several efforts have been enacted to reduce ambulation diversion.12–14 For hospitals, strategies to reduce diversion include implementing ED and hospital patient-flow improvements aimed at reducing ED crowding,15 the primary cause of ambulance diversion.16,17 These improvements include optimizing front end operations, such as patient triage, registration, and tracking.18 Additional improvement maneuvers include adopting hospital-wide full capacity protocols to expedite the transfer of admitted patients from the ED to inpatient units.19 At the regional level, strategies include policies to limit the time EDs are allowed to go on diversion13 and statewide bans on diversion, such as the one implemented in Massachusetts in 2009.20
Despite efforts to prevent hospitals from diverting ambulances or preventing crowding altogether, questions remain about how to best reduce diversion without increasing ED crowding and how best to coordinate regional efforts to reduce diversion.21 Observational data analyses are useful in quantifying the association between ED crowding measures, such as ED patient length of stay or ED occupancy. However, these models are not well equipped to test the impact of multiple strategies to improve ED throughput and increase the ability to receive incoming ambulances.22 Simulation models, typically employed by industrial engineers and operations researchers, are better suited for testing multiple strategies and understanding the interplay – at least theoretically – in a system with multiple moving parts. In particular, these models can simulate the dynamic and interdependent relationships between hospital inpatient flow, ED flow, and ambulance diversion.22 A joint report by the Institute of Medicine and National Academy Engineering in 2005 highlighted the knowledge/awareness divide separating healthcare providers from operations researchers. The report states that bridging this gap is key to improving the quality and efficiency of health care.23 Because simulation models are most often published in engineering journals, the useful knowledge gained may not be reaching the ED medical community.
The goal of this investigation was to perform a systematic review of published simulation model studies that: 1) quantify the tradeoff between ambulance diversion and ED throughput and wait times; 2) identify the predicted impact of patient flow interventions on reducing diversion; and 3) determine the optimal regional strategy for reducing diversion. Our overall goal was to use the results from multiple studies to provide insight in how to optimally reduce ambulance diversion at the hospital and regional level as well as to identify concomitant strategies that reduce the likelihood of increasing ED crowding.
METHODS
We conducted our systematic review and report our methods and results according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.24
Study Eligibility Criteria
We used an a priori defined protocol to search the medical, engineering, and operations research literature for studies using simulation modeling techniques to study ambulance diversion in relation to ED crowding and/or inpatient capacity problems published from 1966–2012. We defined simulation as the development of a mathematical or logical model of a system and the experimental manipulation of the model on a computer, based on the definition of Pritsker.25 The description of these methods to study ED crowding has been previously described in the literature.22 In brief, queuing theory is the formal mathematical study of waiting. Discrete event simulation is used to analyze complex queuing systems that cannot be analyzed algebraically. Discrete event simulation assesses the consequences of multiple individual (i.e. discrete) events occurring over time.
We only included simulation models in which ambulance diversion was a consequence, cause, or method of alleviating ED crowding, or models in which ambulance diversion was a result of upstream causes of ED crowding related to patient flow in the hospital. Hospital flow issues could include such cases as decreased inpatient capacity to accept admitted patients form the ED. Finally, we only included models that have been published either in peer-reviewed journals or in peer-reviewed conference proceedings.
Information Sources
We identified studies by searching electronic databases and scanning reference lists of articles. We applied the search to Medline (1966-Present) and adapted for Inspec, accessed via Web of Knowledge, and Scopus. We used Google Scholar to search for any additional studies that have cited, or were similar, to each of the studies identified through our primary database searches. The search was last updated on February 28, 2012. We also searched the table of contents and abstracts of the Winter Simulation Conference, the Institute for Operations Research and Management Sciences (INFORMS) journals and conference proceedings, as these are important venues for the peer-reviewed publication of simulation models. We also searched the table of contents of the conference proceedings of the Society for Academic Emergency Medicine and the American College of Emergency Physicians.
Search
We recognized from the outset that ambulance diversion is one of the many consequences of ED and hospital crowding. Therefore, we devised our search strategy to identify all simulation studies of ED crowding, as well as simulation studies of hospital patient flow that include the ED in order to maximize our chances of identifying studies that investigate ambulance diversion. We present the full search strings for each of the databases (including Medical Subject Headings [MeSH] terms for Medline) in the Appendix.
Study Selection
One author (MKD) performed the database searches, exported the citations into Endnote X5 (Thomson Reuters, New York, NY), excluded duplicate records, and excluded records that were clearly not relevant based on title and citation. Two reviewers (MKD, LJM) performed eligibility assessment of the potentially relevant remaining abstracts in an unblinded standardized manner. Disagreements between reviewers were resolved by consensus. If agreement could not be reached, it was planned a third author (GSZ) would decide.
Data Collection Process
We developed a data extraction form and pilot tested it on 5 randomly included studies, and refined it accordingly (See Appendix). One author (MKD) extracted the data items below from included studies and a second author (LJM) checked the extracted data. Disagreements were resolved by discussion, and if no agreement could be reached, a third author would decide.
Data Items
For each study, we summarized the study objective and setting. We then summarized the data from the studies into predefined evidence tables on: 1) the tradeoff between ambulance diversion and ED throughput and wait times; 2) the predicted impact of patient flow interventions on reducing diversion; and 3) optimal regional strategies for reducing diversion.
RESULTS
Study Selection
We identified 10 studies for inclusion in the review (Table 1).26–34,38 The search of Medline, Inspec (Web of Knowledge), and Scopus produced 5,115 citations (Figure). After removing duplicates, we reviewed 4,776 unique citations. Of these, we discarded 4,614 records for not meeting inclusion criteria based on review of the title and citation, leaving 162 records for full abstract review. After abstract review, 47 citations possibly met criteria for inclusion and went on to full text review, of which we identified 10 meeting inclusion criteria. The most common reason for exclusion after full-text review was that the simulation model of ED flow did not specifically evaluate ambulance diversion (n=27). Three simulation studies of ED flow that examined ambulance diversion were excluded because they did not answer any of our 3 specific research questions.35–37 We found one additional study meeting inclusion criteria from reviewing the most recent proceedings of the Winter Simulation Conference.31 We did not find any additional studies after cross-referencing the identified studies in Google Scholar, or by searching the conference proceedings of INFORMS, the Society of Academic Emergency Medicine, or the American College of Emergency Physicians.
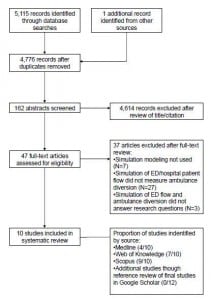
Flowchart of search.
Study Characteristics
An overview of the characteristics and design of the studies included for review is presented in Table 1. All but 2 studies simulated patient flow and ambulance diversion in single hospital settings. The other 2 studies evaluated ambulance diversion between 2–3 neighboring hospitals.27,31
Studies Quantifying the Tradeoff between Ambulance Diversion and ED Throughput/Wait Times
Three studies quantified the relationship between increases in boarding time in the ED or ED length of stay and increases in ambulance diversion rates (Table 2). One study found that triggering ambulance diversion based on number of patients boarding or number of patients in the waiting room rather than based on inpatient bed availability offered the best balance between accessibility and wait times.30 However, the projected magnitude of reduced wait times from activating ambulance diversion was relatively small. This study found that for every percentage point increase in diversion status, average waiting room time was reduced by only 2 minutes if the decision to divert was based on number of patients in waiting room or the number of patients boarding. If the decision to go on diversion is instead based on number of available inpatient beds (without regard to ED census), for every percentage point increase in diversion status, average waiting room time was only reduced by 0.5 minutes.30
All studies found that reducing boarding time and ED length of stay was expected to reduce ambulance diversion. For example, one study found that a 1-hour reduction of mean boarding hours in a trauma center was expected to reduce medical ambulance diversion by 1.2 hours/day and trauma diversion by 0.7 hours/day in an urban tertiary care hospital.32 One study identified various combinations ED throughput benchmarks by whether patients are admitted or discharged that would minimize time on ambulance diversion to less than 3%.28
Studies Evaluating Effect of Patient Flow Interventions on Reducing Ambulance Diversion
Two studies examined ED-based patient flow interventions and their predicted effects on ambulance diversion, which would be triggered based on the ED reaching full capacity and the number of waiting room patients reaching a critical threshold (Table 3). Adding a fast track unit for low acuity patients33 and adding a holding area to remove boarding patients from ED treatment spaces as well as discharge lounge for patient awaiting a ride home or to skilled nursing facilities38 were predicted to each reducing diversion time by between 4–14%. Adding both a holding area and discharge lounge was expected to reduce diversion time by 18–24%.38 Adding an ED observation unit was predicted to have little to no effect on reducing diversion time.38 Finally, one study found that decreasing the average lab turnaround time from 120 minutes to 60 minutes would reduce the time the ED spent on diversion by at least 2 hours per day.34
Three different studies evaluated the effect of dynamic bed management interventions on reducing ambulance diversion (Table 4). Two studies found cancellation of some elective admissions would reduce ambulance diversion.29,32 A simulation study of a tertiary care hospital found that smoothing of the elective surgery schedule to no more than 5 admissions per day expected to result in intensive care unit admission would reduce ambulance diversion.29 A study of a university trauma center found that adopting a strategy that cancels 2–4 elective admissions as the hospital census reaches 5 beds short of capacity would reduce ambulance diversion and could actually increase hospital revenue by $2.7 million per year.32 Another study found that using a simulation model to predict when the ED and hospital are soon to be over capacity in order to activate a “surge unit” could reduce diversion and increase hospital profits (by approximately $600,000 per year).26
Studies Evaluating Optimal Diversion Policy among Multiple Hospitals
Only 2 studies examined cooperative strategies between hospitals compared with no cooperative agreements to reduce ambulance diversion (Table 5). Both studies found that cooperative strategies among hospitals to reduce diversion were more effective than not having a cooperative strategy. One study provided quantitative evidence that without cooperative diversion strategies, hospitals are likely to go on “pre-emptive” or “defensive” diversion.27 The other study found that a cooperative strategy that allows some hospitals to go on ambulance diversion based on number of patients in waiting room and that diverted patients to go to the least crowded hospital would optimally reduce “non-value added wait times” more than a simple ban on diversion across hospitals.31 However, these findings only apply to urban areas where the distance between hospitals is small.
DISCUSSION
In this review of the medical, engineering, and operations research literature, we identified 10 simulation studies that advance the current understanding of the optimal strategies to reduce ambulance diversion. Overall, most simulations involved single EDs, which limits the generalizability of the predicted consequences of various scenarios and the outcome of ambulance diversion. However, there are a number of insights on reducing ambulance diversion that had not been elucidated in previous non-simulation studies on ambulance diversion that could be the starting point for future intervention and policy studies. The insights included: 1) the desired effect of reducing ED waiting room times by diverting ambulances is likely to be very small; 2) if diversion is used, making the decision to divert should be based on number of patients in the waiting room or number of ED boarders instead of just a lack of inpatient beds; 3) adding fast track units and holding units for ED boarders are likely to reduce ambulance diversion; and 4) some dynamic bed management strategies such as smoothing elective surgical admission caseloads could both reduce ambulance diversion and increase hospital revenue. The identified studies also confirm that cooperative strategies among the hospitals may be helpful in preventing “defensive” or “pre-emptive” diversion.12,39 “Defensive” diversion occurs when a hospital goes on diversion right after a neighboring hospital goes on diversion in order to ward off excessive ED demand from the patients that are being diverted from the neighboring hospital.39
This is the first study to systematically review existing literature on simulation models of ambulance diversion with the goal of identifying insights into reducing diversion. One previous study published in the engineering literature examined simulation models on EDs in general.40 However, this study focused on modeling techniques, data sources and collection methods, and patient classification and flows, and did not summarize the findings of these studies with regards to our focused research questions.40 Previous reviews of ED crowding and ambulance diversion have been published in the medical literature, but these studies did not capture the contributions of simulation model studies.6,17
These studies provide a starting point for testing various strategies at reducing diversion “in-vitro” while allowing for the predicted effect on patient flow and in some cases, hospital revenue. Because of the dynamic and inter-related nature of hospital and ED capacity on patient flow, these types of predictions cannot readily be made with traditional observational and biomedical research methods.22 For example, a systematic review of the medical literature on ambulance diversion identified that there is no quantitative evidence that ambulance diversion actually relieves ED crowding or improves ED throughput times.6 We identified a simulation study of a community hospital ED which found that the effect of diversion on waiting room times is quite small (2 minute reduction for every percentage point increase of time on diversion).30 If this finding can be confirmed in other simulation and observational studies, it is unlikely that the small decrease in waiting room times from ambulance diversion could outweigh the unintended consequences of prolonged transport times and possibly worse outcomes of diverted patients.6,7,10
While it has been known that expanding hospital capacity by adding more inpatient beds could reduce diversion,41 it may not be easy for many hospitals to add new beds due to space and financial limitations and the hurdles of licensing newly added beds. On the other hand, we identified simulation models that evaluated various strategies to optimize currently available inpatient resources. Two studies found that dynamic management of elective admissions could reduce ambulance diversion,29,32 and one study found that this could be done in a way that increases hospital revenue.32
These models also provide novel experimental insight into alternative methods for networks of hospitals to reduce ambulance diversion. One model found that a coordinated approach that allowed ambulance diversion to be triggered by the number of patients in the waiting room and that rerouted diverted patients to the least crowded ED would lead to the greatest improvement in patient throughput across all EDs.31 Although this makes intuitive sense, this arrangement would be difficult to implement in practice. It would require all participating EDs to share a common electronic dashboard displaying wait times and ED census. It would also require a central authority available at all times to coordinate the re-routing of ambulances to the least crowded hospitals. Furthermore, implementation of such a program would not put as much pressure on hospital administrators to address root causes of ambulance diversion, such as inpatient throughput and ED boarding, as would implementing a total ban on ambulance diversion. However, this optimized coordinated approach may appeal to regions that have implemented an ambulance diversion ban and are noticing that wait times are increasing despite best efforts to improve inpatient throughput.
LIMITATIONS
Our study has a number of limitations. First, the main limitation with this systematic review, as with any overview, is that study settings, patient populations, scenarios tested, and measurement of the outcome (ambulance diversion) varied across studies. Second, there are no published or validated tools to assess the quality of simulation model studies as compared to the numerous tools available for observational and randomized control studies.42, 43 Therefore, it is difficult to assess the quality of the studies included for our analysis. Third, one reviewer, as opposed to two or more, did the initial database search and exclusions. However, given the clear primary exclusion criteria, there is little reason to believe that this may have led to bias in the selection of studies. Fourth, 6 out of 10 studies included in our analysis were published in peer reviewed conference proceedings and not in the peer review literature.26, 27, 30, 31, 33, 38 However, the Proceedings of the Winter Simulation Conference is considered a top-tier publication venue in the field, and studies published in the proceedings are usually not submitted to peer review journals. We felt that excluding these studies would exclude a significant body of work related to this topic. Future publication of simulation models in the medical literature would likely increase the perceived reliability of these results among the ED medical community. Finally, the studies included in this review are all simulation studies. The results of these simulation models need to be confirmed in real world settings.
CONCLUSION
In summary, smoothing elective surgery caseloads, adding ED fast tracks as well as holding units for inpatient boarders, improving ED lab turnaround times, and implementing regional cooperative agreements among hospitals are promising avenues for reducing diversion. Using ambulance diversion to alleviate ED crowding is expected to only have a minimal effect on reducing ED wait times. However, if diversion is used to try to temporarily alleviate ED crowding, this decision should be based on the number of patients in the waiting room or number of admitted patients boarding rather than a lack of available inpatients beds alone. More simulation research is especially needed to project the effects of implementing ambulance diversion bans on ED throughput times and hospital revenues.
Footnotes
Address for Correspondence: M. Kit Delgado, MD, MS. Department of Surgery, Division of Emergency Medicine, Stanford University School of Medicine, M121 Alway Bldg. 300 Pasteur Drive, Stanford, CA 94305. Email: kdelgado@stanford.edu.
Submission history: Revision received June 11, 2012; Submitted December 22, 2012; Accepted March 25, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Burt CW, McCaig LF Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003–04. Adv Data. 2006; :1-23
2 Lagoe RJ, Jastremski MS Relieving overcrowded emergency departments through ambulance diversion. Hospital Topics. 1990; 68:23
3 Redelmeier DA, Blair PJ, Collins WE No place to unload: a preliminary analysis of the prevalence, risk factors, and consequences of ambulance diversion. Ann Emerg Med. 1994; 23:43-47
4 Trzeciak S, Rivers E Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003; 20:402
5 Begley CE, Chang YC, Wood RC Emergency department diversion and trauma mortality: evidence from Houston, Texas. J Trauma. 2004; 57:1260
6 Pham JC, Patel R, Millin MG The effects of ambulance diversion: a comprehensive review. Acad Emerg Med. 2006; 13:1220-1227
7 Shen YC, Hsia RY Association between ambulance diversion and survival among patients with acute myocardial infarction. JAMA. 2011; 305:2440-2447
8 Soremekun OA, Brown DF, Pines JM Ambulance diversion and survival among patients with acute myocardial infarction. JAMA. 2011; 306:1324-1325
9 Handel DA, John McConnell K The financial impact of ambulance diversion on inpatient hospital revenues and profits. Acad Emerg Med. 2009; 16:29-33
10 Yankovic N, Glied S, Green LV The Impact of Ambulance Diversion on Heart Attack Deaths. Inquiry. 2010; 47:81-91
11 McConnell KJ, Richards CF, Daya M Ambulance diversion and lost hospital revenues. Ann Emerg Med. 2006; 48:702-710
12 Vilke GM, Castillo EM, Metz MA Community trial to decrease ambulance diversion hours: the San Diego county patient destination trial. Ann Emerg Med. 2004; 44:295-303
13 Patel PB, Derlet RW, Vinson DR Ambulance diversion reduction: the Sacramento solution. Am J Emerg Med. 2006; 24:206-213
14 Castillo EM, Vilke GM, Williams M Collaborative to decrease ambulance diversion: the California Emergency Department Diversion Project. J Emerg Med. 2011; 40:300-307
15 McClelland MS, Lazar D, Sears V The past, present, and future of urgent matters: lessons learned from a decade of emergency department flow improvement. Acad Emerg Med. 2011; 18:1392-1399
16 Schull MJ, Lazier K, Vermeulen M Emergency department contributors to ambulance diversion: a quantitative analysis. Ann Emerg Med. 2003; 41:467-476
17 Hoot NR, Aronsky D Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008; 52:126-136
18 Wiler JL, Gentle C, Halfpenny JM Optimizing emergency department front-end operations. Ann Emerg Med. 2010; 55:142-160
19 Villa-Roel C, Guo X, Holroyd BR The role of full capacity protocols on mitigating overcrowding in EDs. Am J Emerg Med. ;
20 Friedman FD, Rathlev NK, White L Trial to end ambulance diversion in Boston: report from the conference of the Boston teaching hospitals consortium. Prehosp Disaster Med. 2011; 26:122-126
21 Olshaker JS, Rathlev NK Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the emergency department. J Emerg Med. 2006; 30:351-356
22 Wiler JL, Griffey RT, Olsen T Review of modeling approaches for emergency department patient flow and crowding research. Acad Emerg Med. 2011; 18:1371-1379
23 Reid PP, Compton WD, Grossman JH . Building a Better Delivery System: A New Engineering/Health Care Partnership. 2005;
24 Liberati A, Altman DG, Tetzlaff J The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009; 62:e1-e34
25 Pritsker A . Introduction to Simulation and SLAM II. 1986;
26 Chockalingam A, Jayakumar K, Lawley M A stochastic control approach to avoiding emergency department overcrowding. . ;
27 Hagtvedt R, Ferguson M, Griffin P Cooperative strategies to reduce ambulance diversion. . ;
28 Kolker A Process modeling of emergency department patient flow: Effect of patient length of stay on ED diversion. J Medical Syst. 2008; 32:389-401
29 Kolker A Process modeling of ICU patient flow: effect of daily load leveling of elective surgeries on ICU diversion. J Med Syst. 2009; 33:27-40
30 Nafarette A, Fowler J, Wu T Bi-criteria analysis of ambulance diversion policies. . ;
31 Nafarrate AR, Fowler JW, Wu T Design of centralized ambulance diversion policies using simulation-optimization. . ;
32 Pines JM, Batt RJ, Hilton JA The financial consequences of lost demand and reducing boarding in hospital emergency departments. Ann Emerg Med. 2011; 58:331-340
33 Ramirez A, Fowler J, Wu T Analysis of ambulance diversion policies for a large-size hospital. . ;
34 Storrow AB, Zhou C, Gaddis G Decreasing lab turnaround time improves emergency department throughput and decreases emergency medical services diversion: a simulation model. Acad Emerg Med. 2008; 15:1130-1135
35 Hoot NR, LeBlanc LJ, Jones I Forecasting emergency department crowding: a discrete event simulation. Ann Emerg Med. 2008; 52:116-125
36 Hoot NR, Leblanc LJ, Jones I Forecasting emergency department crowding: a prospective, real-time evaluation. J Am Med Inform Assoc. 2009; 16:338-345
37 Criswell M, Hasan I, Kopach R Emergency Department divert avoidance using Petri nets. . ;
38 Kolb EMW, Schoening S, Peck J Reducing emergency department overcrowding: five patient buffer concepts in comparison. . ;
39 Vilke GM, Brown L, Skogland P Approach to decreasing emergency department ambulance diversion hours. J Emerg Med. 2004; 26:189-192
40 Paul SA, Reddy MC, DeFlitch CJ A systematic review of simulation studies investigating emergency department overcrowding. Simulation. 2010; 86:559-571
41 McConnell KJ, Richards CF, Daya M Effect of increased ICU capacity on emergency department length of stay and ambulance diversion. Ann Emerg Med. 2005; 45:471-478
42 Von Elm E, Altman DG, Egger M The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bulletin of the World Health Organization. 2007; 85:867-872
43 Moher D, Jadad AR, Nichol G Assessing the quality of randomized controlled trials: an annotated bibliography of scales and checklists. Controlled Clin Trials. 1995; 16:62-73


