| Author | Affiliation |
|---|---|
| Michael D. Menchine, MD, MPH | Keck School of Medicine of the University of Southern California, Department of Emergency Medicine, Los Angeles, CA |
| Anita Vishwanath, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Sanjay Arora, MD | Keck School of Medicine of the University of Southern California, Department of Emergency Medicine, Los Angeles, CA |
ABSTRACT
Introduction:
To determine the prevalence of diabetes in Southern California emergency department (ED) patients and describe the self-reported general health, demographic and social characteristics of these patients with diabetes.
Methods:
Between April 2008 and August 2008, non-critical patients at two Southern California EDs completed a 57-question survey about their chronic medical conditions, general health, social and demographic characteristics.
Results:
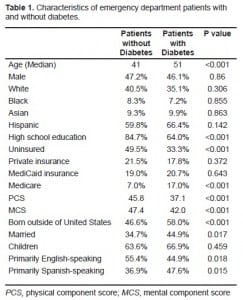
11.3% of the 1,303 patients surveyed had diabetes. Patients with diabetes were similar to ED patients without diabetes with respect to gender, ethnicity and race. However, patients with diabetes were older (51 vs. 41), less likely to have a high school education (64.0% vs. 84.7%), less likely to speak English (44.9% vs. 55.4%), and less likely to be uninsured (33.3% vs. 49.5%). Additionally, patients with diabetes had markedly lower self-reported physical health scores (37.1 vs. 45.8) and mental component score and mental health scores (42.0 vs. 47.4) compared with ED patients without diabetes.
Conclusion:
In this study of two Southern California EDs, 11.3% of surveyed patients had diabetes. These patients were often poorly educated, possessed limited English language skills and poor physical health. ED personnel and diabetes educators should be mindful of these findings when designing interventions for ED patients with diabetes.
INTRODUCTION
Each year millions of patients receive health services in emergency departments (EDs), and, regrettably, for many of them, this may be their primary source of care.1,2 A large portion of these ED patients have diabetes, and, alarmingly, previous research has demonstrated their mean HbA1c is over 9%.3 Although numerous innovative programs have been created to help high-risk, disadvantaged patients achieve adequate glycemic control, none are based out of the ED.4–7 To create such an ED-based program, we must first uncover some basic characteristics of ED patients with diabetes. As part of an ongoing needs assessment, we sought to determine the self-reported prevalence of diabetes in ED patients, their self-reported general health and associated demographic and social characteristics.
METHODS
We conducted an anonymous cross sectional survey of a convenience sample of patients presenting to the EDs at both the University of California, Irvine (UCI) and Los Angeles County Hospital at the University of Southern California (LAC+USC) from April –August 2008. The study sites were selected to evaluate a possible variance of diabetes prevalence across different types of Southern California EDs. UCI is a private academic hospital serving approximately 40,000 ED patients annually. LAC+USC is a county hospital in central Los Angeles and serves approximately 170,000 patients annually. Patients were eligible to complete the survey if they were 18 years or older, able to complete the survey in English or Spanish, and were not critically ill or injured. If necessary, the survey was read to the patient in their language of choice, although generally the subjects completed a written survey. The protocol was reviewed and approved by the institutional review boards of the two institutions. Trained research assistants screened patients for eligibility in the adult waiting areas at each institution, obtained informed consent and administered the survey. The survey included 57 questions and took ten minutes to administer. Patients were queried regarding their demographic characteristics, ethnicity, chronic medical conditions, health insurance status and reasons for which they were presenting to the ED. Subjects then completed the Short Form Health Survey version 2 (SF-12). This is a validated tool that yields a mental component score (MCS) and physical component score (PCS) that can be compared across populations. The MCS and PCS for the general United States adult population are 50 with standard deviation of ten. We transcribed data from paper surveys into Microsoft Excel (Microsoft Corp, Richmond Wa.) and analyzed it using Stata 10.0 (Statacorp, College Station, Tx). Means and 95% confidence limits are reported. We performed tests of significance using the Fisher Exact test for categorical variables and Mann-Whitney U for continuous variables (as the data was non-normally distributed). Finally, we conducted a multivariate logistic regression to determine which variables were independently associated with a self-reported history of diabetes.
RESULTS
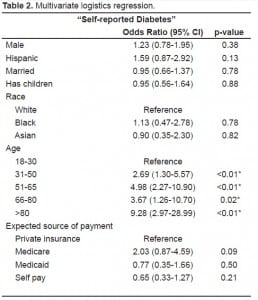
One thousand three-hundred three patients completed the survey, 802 at USC and 501 at UCI. Overall, 147 (11.3% 9.6–13.0%) reported a history of diabetes. Mean age of respondents was 42 years and 47% were male. The prevalence of disease did not vary significantly by site (11.6% at UCI vs. 11.1% at LAC+USC). Table 1 shows characteristics of patients with and without diabetes. ED patients with and without diabetes were similar in gender, ethnicity and race. However, ED patients with diabetes were older, less likely to have a high school education (64.0% vs. 84.7 %) or speak primarily English (44.9% vs. 55.4%) and more likely to be insured (49.5% vs. 33.3%) compared with ED patients without diabetes. Additionally, ED patients with diabetes had markedly lower self-reported PCS (37.1 [95% CI 35.7–40.3] vs. 45.8 [95% CI 44.0–46.5]) and MCS (42.0 [95% CI 39.4–43.6] vs. 47.4 [95% CI 46.8–48.0]) scores compared with ED patients without diabetes. On multivariate regression, older age and lack of a high school education continued to be independently associated with an increased odds of diabetes. (See Table 2 for results of the multivariate regression.)
DISCUSSION
This is the first study to document the prevalence of self-reported diabetes in ED patients. Two previous studies attempted to document the prevalence of undiagnosed diabetes in ED patients. Both, however, were undermined by poor follow up for confirmatory testing, leaving the results difficult to interpret. Our finding that one in nine sampled patients has diabetes and that their self-reported health is significantly lower than their ED counterparts without diabetes, coupled with prior research indicating ED patients with diabetes have HbA1c levels over 9%, suggest that the ED is an important area in which to plan and focus future interventions.3
Developing treatment interventions for ED populations with chronic diseases can be logistically difficult as these patients may lack the resources to optimize self-care. Our findings confirm some of these impressions. More than one-third of ED patients with diabetes had less than high school education, nearly half spoke primarily Spanish, and 33% were uninsured. In addition, their scores for physical and mental health were poor. Interventions aimed at helping this medically needed population must be mindful of these findings. Innovative strategies using nurse educators, case managers and community health workers have been successfully used in non-ED settings to help similarly disadvantaged people achieve improved glycemic control.4–7,10 Unfortunately, to date, there have been no reported trials of ED-based programs to improve glycemic control or quality of life in patients with diabetes. Undoubtedly, the acute, symptom-driven and episodic care provided in the ED is not well suited for the management of chronic diseases such as diabetes. However, previous ED-based efforts for conditions such as smoking cessation, intimate partner violence, and alcohol aversion suggest that interventions for chronic conditions can be effective in the ED setting.11–15 It follows that the ED visit may represent a unique teachable moment during which patients with diabetes can be offered resources to improve glycemic control and physical functioning. Moreover, for many patients with diabetes, the ED may be the primary potential entry point into the healthcare system.
LIMITATIONS
A limitation of our study is that we sampled only two academic Southern California EDs with largely Latino populations, thus limiting the generalizability of these findings. However, the EDs did vary in terms of size (170,000 vs. 40,000) and primary funding mechanism (county vs. private). A second limitation is that this study may underestimate the prevalence of diabetes in ED patients as some patients may have forgotten about this diagnosis while many others may yet be undiagnosed. Recent studies suggest the prevalence of undiagnosed diabetes in ED patients may be 3–7%, suggesting, if anything, a greater need for ED-based diabetes programs.8.9 The use of a convenience sample may have introduced some selection bias although we cannot determine the direction this may have biased the result. In addition, we excluded patients who were critically ill or injured as we believed they would not be able to complete the survey. Thus, we do not know the prevalence of diabetes in this subset of patients. Finally, we did not test patients’ glycosylated hemoglobin, and therefore cannot determine which variables are associated sub-optimal glycemic control.
CONCLUSION
In this study 11.3% of patients had a self-reported history of diabetes. These patients were older, less educated, had poorer physical and mental health and were less likely to speak English than their counterparts without diabetes. These findings should be considered when developing appropriate, effective and culturally sensitive ED-based mechanisms to help patients achieve glycemic control.
Footnotes
Supervising Section Editor: Trevor Mills, MD, MPH
Submission history: Submitted January 31, 2010; Revision Received: April 14, 2010; Accepted May 7, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Michael D Menchine, MD, MPH, Department of Emergency Medicine, Keck School of Medicine, University of Southern California, LAC+USC Medical Center, 1200 N. State Street, Room 1011, Los Angeles CA 90033
Email: menchine@usc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Weber EJ, Showstack JA, Hunt KA, et al. Does lack of a usual source of care or health insurance increase the likelihood of an emergency department visit? Results of a national population-based study. Ann Emerg Med. 2005;45(1):4–12. [PubMed]
2. Hunt KA, Weber EJ, Showstack JA, et al. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006 Jul;48(1):1–8. [PubMed]
3. Josephsen G, Rusnak R. Poor glycemic control in diabetic patients seeking care in the ED. Am J Emerg Med. 2006 Oct;24(6):721–4. [PubMed]
4. Babamoto KS, Sey KA, Camilleri AJ, et al. Improving diabetes care and health measures among Hispanics using community health workers: results from a randomized controlled trial. Health Educ Behav. 2009 Feb;36(1):113–26. [PubMed]
5. Sixta CS, Ostwald S. Texas-Mexico border intervention by promotores for patients with type 2 diabetes. Diabetes Educ. 2008;34(2):299–309. [PubMed]
6. Davis KL, O’Toole ML, Brownson CA, et al. Teaching how, not what: the contributions of community health workers to diabetes self-management. Diabetes Educ. 2007;33 (Suppl 6):208S–215S. [PubMed]
7. Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization: a randomized, controlled trial. Ann Intern Med. 1998;129(8):605–12. [PubMed]
8. Ginde AA, Cagliero E, Nathan DM, et al. Point-of-care glucose and hemoglobin A1c in emergency department patients without known diabetes: implications for opportunistic screening. Acad Emerg Med. 2008;15(12):1241–7. Epub 2008 Sep 8. [PubMed]
9. Silverman RA, Pahk R, Carbone M, et al. The relationship of plasma glucose and HbA1c Levels among emergency department patients with no prior history of diabetes mellitus. Acad Emerg Med.2006;13(7):722–6. [PubMed]
10. Witmer A, Seifer SD, Finocchio L, et al. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–8. [PMC free article] [PubMed]
11. Bernstein SL, Boudreaux ED, Cabral L, et al. Efficacy of a brief intervention to improve emergency physicians’ smoking cessation counseling skills, knowledge, and attitudes. Subst Abus.2009;30(2):158–81. [PubMed]
12. MacMillan HL, Wathen CN, Jamieson E, et al. Screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2009;302(5):493–501. [PubMed]
13. Bernstein E, Bernstein J. Effectiveness of alcohol screening and brief motivational intervention in the emergency department setting. Ann Emerg Med. 2008;51(6):751–4. Epub 2008 Apr 23.[PubMed]
14. D’Onofrio G, Pantalon MV, Degutis LC, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Ann Emerg Med. 2008;51(6):742–750.e2. Epub 2008 Apr 23.[PMC free article] [PubMed]
15. Stein LA, Minugh PA, Longabaugh R, et al. Readiness to change as a mediator of the effect of a brief motivational intervention on posttreatment alcohol-related consequences of injured emergency department hazardous drinkers. Psychol Addict Behav. 2009;23(2):185–95.[PMC free article] [PubMed]


