| Author | Affiliation |
|---|---|
| Jennifer A. Cooper, DO | Brooke Army Medical Center, Department of Emergency Medicine, San Antonio, Texas |
| Curtis J. Hunter, MD | Brooke Army Medical Center, Department of Emergency Medicine, San Antonio, Texas |
INTRODUCTION
Penetrating injuries to the face or neck can cause difficult airway issues. There is a relative dearth of literature to define the best approach to these patients. Impalement injuries are uncommon, and survivable injuries are most commonly confined to the abdomen or thorax. We report the case of a patient with an obviously difficult airway due to a facial impalement (Jael’s Syndrome) injured at a local construction site.
CASE REPORT
A 25-year-old male was working with braided cable under tension at a local construction site when the cable, approximately 2 inches in diameter, snapped without warning and perforated his right cheek, penetrating his right temporal and right parietal lobe. After shortening the cable to 1.5 feet at the construction site, emergency medical services brought the patient to our Level I trauma center. He was transported wearing a cervical spine collar in the sitting position. On arrival, he was awake and alert, unable to speak, and mildly agitated. His initial vital signs were a blood pressure of 159/67 mmHg, heart rate of 54 beats per minute, respiratory rate of 18 breaths per minute, and a pulse oximetry reading of 97% on 15 liters of oxygen. The remainder of his primary and secondary surveys revealed no further injuries.
Because of the position of the cable through his jaw and upward into his brain, the patient was unable to open his mouth more than two centimeters. In the trauma bay he became more agitated and began to pull at the cable that protruded 1.5 feet outside of his mouth. We decided to sedate and intubate him to facilitate further evaluation and treatment of his injuries. After 30 mg of etomidate and 100 mg of succinylcholine administered intravenously, blood and construction site debris was suctioned from his oropharynx, and he was intubated using the GlideScope Portable GVL and a 7.5 endotracheal tube on the first attempt.
The patient was taken for an IV-contrasted computed tomography of his brain, face, and neck to assess vascular injury and define the extent of damage (Figure).
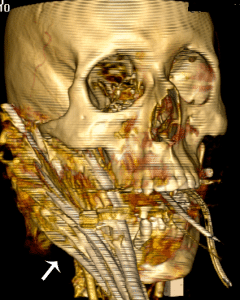
The cable entered the right mandible at the level of the angle of the mandible and superiorly near the condyle, terminating 3 cm into the right temporal lobe.
The patient was taken to the operating room for cable removal, neck exploration, facial nerve exploration, right temporal craniotomy, and tracheostomy. He was found to have a cranial nerve XII paralysis, right temporal and parietal lobe traumatic brain injury and intraparenchymal hemorrhage, intraventricular hemorrhage, right cochlea damage, and some general soft tissue damage. On post-operative day 3, he was transferred to the floor on a liquid diet. On post-operative day 7 he was diagnosed with bacterial meningitis after developing a headache, fever, and neck rigidity. On post-operative day 13 he was discharged on oral antibiotics to a rehabilitation facility.
DISCUSSION
This patient clearly had a difficult airway, with a large foreign body inhibiting evaluation, and limiting options for definitive airway choices. Assisted ventilation was not an option with the foreign body in place, and removing his ability to protect his own airway took us down the potential road of not being able to ventilate or intubate. The size of the cable and extent of external damage was daunting; clinically we were most concerned about swelling and hemorrhage into the airway, further pressured by his increasing agitation. Intubation via “line-of-sight” direct laryngoscopy or placement of an laryngeal mask airway was not feasible given the patient’s inability to open his mouth.
At our institution, the emergency medicine (EM) junior resident is responsible for patient intubation. Because of the patient’s agitation, we felt an awake fiber-optic intubation would have been difficult. We chose the GlideScope® as a method of laryngeal visualization with minimal orofacial manipulation, with the added benefit of having the faculty EM physician and senior anesthesia resident able to directly monitor the procedure. Our backup airway plan included an Eschmann introducer, and our final airway plan was for cricothyroidotomy, with the neck already prepped for the surgical procedure.
Literature reviewing difficult airways suggests an algorithm that considers direct laryngoscopy, awake intubations, surgical airways, various airway adjuncts, and fiberoptic choices, to include videolaryngoscopy.1–3 Studies examining airway management in penetrating neck and face injury generally recommend direct laryngoscopy when feasible, with rapid progression to surgical airways.4–10 Medical paralysis to facilitate definitive airway management is controversial, with some recommending against it.4,11 One large retrospective study suggested lack of neuromuscular blockade increased the risk of difficult intubations, and other small studies have suggested that rapid sequence intubation is the approach of choice.5–6,12 The American Society of Anesthesiology recommends the awake approach in the difficult airway algorithm.11
The leading causes of orotracheal intubation failures in trauma patients are difficult anatomy, a foreign body in the airway, or unrecognized head or neck injury, causing an unanticipated difficult airway.13 Videolaryngoscopy in the hands of an experienced user (able to manipulate the endotracheal tube based on the video view rather than a direct view) can mitigate the effects of difficult anatomy. The only previous case reports we could find with a similar injury were mixed in their airway approach. One moved directly to a surgical airway when the patient’s oxygen saturation began to decline, and the others did an awake or anesthetized fiber-optic nasotracheal intubation.14–16 Management of the difficult airway is best guided by the urgency of the patient’s injuries and the options available to the team doing the intubation; weighing the risks and benefits of awake endotracheal intubation versus rapid sequence intubation in patients with penetrating neck injuries requires special consideration.
We chose what we felt was our best method of laryngeal visualization and orotracheal intubation, to include neuromuscular blockade, with the understanding that a failed first attempt would most likely result in a surgical airway. The intubating physician had previous experience with the GlideScope®, performing two live intubations and 10 mannikin intubations, and was familiar with manipulating the endotracheal tube based on the video picture alone. Given the clinical need for sedation and paralysis, we saw no significant risks to a single attempt at videolaryngoscopy while the patient’s neck was being prepared for cricothyroidotomy.
CONCLUSION
The diverse nature of penetrating face and neck injuries precludes a single method for airway management. Emergency physicians are reminded to be prepared for a difficult airway with appropriate equipment and a rapidly executable algorithm. It is important that a backup surgical airway is prepared and available prior to administration of paralytic agents. In this case, the choice of the GlideScope® was successful, suggesting that videolaryngoscopy can be included in the algorithm of a provider who is familiar with the instrument.
Footnotes
Supervising Section Editor: Rick A. McPheeters, DO
Submission history: Submitted March 28, 2012; Revision received June 17, 2012; Accepted July 9, 2012
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.7.11984
Address for Correspondence: Jennifer A. Cooper, San Antonio Military Medical Center, 3851 Roger Brooke Drive, San Antonio, TX 78234. Email: jaye32@hotmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none. The views expressed herein are those of the authors and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, Department of Defense or the U.S. Government.
REFERENCES
1. Dupanovic M, Fox H, Kovac A. Management of the airway in multitrauma. Curr Opin Anaesthesiol.2010;23:276–282. [PubMed]
2. Langergon O, Birenbaum A, Amour J. Airway management in trauma. Minerva Anestesiol.2009;75:307–311. [PubMed]
3. Sise MJ, Shackford SR, Sise CB, et al. Early intubation in the management of trauma patients: indications and outcomes in 1,000 consecutive patients. J Trauma. 2009;66:32–40. [PubMed]
4. Boahene KO, Thompson DM, Schulte DL, et al. Craniofacial Metal bolt injury: an unusual mechanism. J Trauma. 2004;56:716–719. [PubMed]
5. Mandavia DP, Qualls S, Rokos I. Emergency airway management in penetrating neck injury. Ann Emerg Med. 2000;35:221–225. [PubMed]
6. Shearer VE, Giesecke AH. Airway management for patients with penetrating neck trauma: a retrospective study. Anesth Analg. 1993;77:1135–1138. [PubMed]
7. Cogbill TH, Cothren CC, Ahearn MK, et al. Management of maxillofacial injuries with severe oronasal hemorrhage: a multicenter perspective. J of Trauma. 2008;65:994–999. [PubMed]
8. Brywczynski JJ, Barrett TW, Lyon JA, et al. Management of penetrating neck injury in the emergency department: a structured literature review. Emerg Med J. 2008;25:711–715. [PubMed]
9. Grewal H, Rao PM, Mukerji S, et al. Management of penetrating laryngotracheal injuries. Head and Neck. 1995;17:494–502. [PubMed]
10. Eggen JT, Jorden RC. Airway management, penetrating neck trauma. J Emerg Med. 1993;11:381–385. [PubMed]
11. Tallon JM, Ahmed JM, Sealy B. Airway management in penetrating neck trauma at a Canadian tertiary trauma centre. CJEM. 2007;9:101–104. [PubMed]
12. Lundstrom LH, Moller AM, Rosenstock C, et al. Avoidance of neuromuscular blocking agents may increase the risk of difficult tracheal intubation: a cohort study of 103 812 consecutive adult patients recorded in the Danish Anaesthesia Database. British J of Anaesth. 2009;103:283–290. [PubMed]
13. Stephens CT, Kahntroff S, Dutton RP. The success of emergency endotracheal intubation in trauma patients: a 10-year experience at a major adult trauma referral center. Anesthesia and Analgesia. 2009;109:866–872. [PubMed]
14. Tabariai E, Sandhu S, Alexander G, et al. Management of facial penetrating injury – a case report.J Oral Maxillofac Surg. 2010;68:182–187. [PubMed]
15. Joly LM, Oswald AM, Disdet M, et al. Difficult endotracheal intubation as a result of penetrating cranio-facial injury by an arrow. Anesth Analg. 2002;94:231–232. [PubMed]
16. Melillo EP, Hawkins DJ, Lynch L, et al. Difficult airway management of a child impaled through the neck. Pediatric Anaesthesia. 2001;11:615–617. [PubMed]


