| Author | Affiliation |
|---|---|
| Mark J. Deaver, MD, MBA | Harbor-University of California, Los Angeles, Department of Emergency Medicine |
| Eric F. Silman, MD | University of California, San Francisco, Department of Emergency Medicine |
| Shahram Lotfipour, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
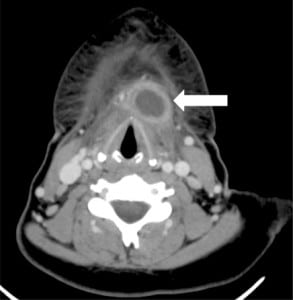
A 23-year-old female presented to the emergency department (ED) with a five-day history of sore throat, body aches and 24 hours of throat swelling accompanied by globus sensation and hoarseness. The patient was afebrile with normal vital signs. Physical exam was significant for a firm, non-erythematous anterior neck mass that was exquisitely tender to palpation. The mass was noted to move slightly with swallowing. A CT scan with contrast revealed a 2 x 2.5 x 3 cm cystic lesion with a thick, enhancing rim located inferior to the hyoid bone with overlying soft tissue swelling. Given the history and radiographic appearance of the lesion, a diagnosis of infected thyroglossal duct cyst was made. The patient was started on Clindamycin in the ED and admitted to ENT for needle aspiration and 23-hour observation.
Thyroglossal duct cysts (TGDC) are the most common cause of midline neck masses.1TGDC are typically located inferior to the hyoid bone (65%) in the region adjacent to the thyrohyoid membrane.2 However, these remnants can occur anywhere along the path followed by the primordial thyroid gland during descent from the base of the tongue. Frequently presenting as an asymptomatic neck mass in the pediatric population, the most common presentation in adults is underlying infection of the cyst.1 Other common causes of midline neck masses include lymphadenopathy, dermoid cysts, and various odontogenic anomalies. Classic physical exam findings include a mobile neck mass that moves with swallowing or protrusion of the tongue. Accompanying symptoms include sore throat, pain, dysphagia, hoarseness, and globus. Serious complications involve airway obstruction precipitated by rapid enlargement of the cyst. Findings on CT include a well-circumscribed lesion with significant rim enhancement.3
Definitive treatment of infected TGDC involves both antibiotics and needle aspiration. Examination of the aspirate allows for identification of the involved organisms as well as cytologic analysis to rule out underlying TGDC carcinoma. The most common organisms involved include Staphylococus epidermis, Haemophilus influenza, and Staphylococcus aureu.3 Following control of the underlying infection, the patient may elect to surgically remove the cyst to prevent further recurrence.
Footnotes
Supervising Section Editor: Rick A McPheeters, DO
Submission history: Submitted June 26, 2008; Revision Received July 29, 2008; Accepted August 01, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Shahram Lotfipour, MD, MPH, Associate Clinical Professor, 101 The City Drive, Rte 128-01, Orange, CA 92868
Email: SHL@uci.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Acierno S, Waldhausen J. Congenital Cervical Cysts, Sinuses and Fistulae. Otolaryngol.Clin N Am. 2007;40:161–176.
2. Batsakis JG. Tumors of the head and neck: clinical and pathological considerations. 2nd ed. Baltimore: Williams & Wilkins; 1979. pp. 233–239.
3. Reede D, Bergeron R, Som P. CT of Thyroglossal Duct Cysts. Radiology. 1985;157:121–125. [PubMed]


