| Author | Affiliation |
|---|---|
| Steven T Dorsey, MD | Emergency Services Institute, Cleveland Clinic, Cleveland, Ohio |
| Eric T Harrington, DO | Quincy Valley Medical Center, Quincy, Washington |
| W. F. Peacock IV, MD | Emergency Services Institute, Cleveland Clinic, Cleveland, Ohio |
| Charles L Emerman, MD | MetroHealth Medical Center, Department of Emergency Medicine, Cleveland, Ohio |
ABSTRACT
Introduction:
The purpose of our study was to describe the evaluation and outcome of patients with ileus and bowel obstruction admitted to an emergency department (ED) observation unit (OU) and to identify predictors of successful management for such patients.
Methods:
We performed a retrospective chart review of 129 patients admitted to a university-affiliated, urban, tertiary hospital ED OU from January 1999 through November 2004. Inclusion criteria were all adult patients admitted to the OU with an ED diagnosis of ileus, partial small bowel obstruction, or small bowel obstruction, and electronic medical records available for review. The following variables were examined: ED diagnosis, history of similar admission, number of prior abdominal surgeries, surgery in the month before, administration of opioid analgesia at any time after presentation, radiographs demonstrating air–fluid levels or dilated loops of small bowel, hypokalemia, use of nasogastric decompression, and surgical consultation.
Results:
Treatment failure, defined as hospital admission from the OU, occurred in 65 (50.4%) of 129 patients. Only the use of a nasogastric tube was associated with OU failure (21% discharged versus 79% requiring admission, P = 0.0004; odds ratio, 5.294; confidence interval, 1.982–14.14).
Conclusion:
Half of the patients admitted to our ED OU with ileus or varying degrees of small bowel obstruction required hospital admission. The requirement of a nasogastric tube in such patients was associated with a greater rate of observation unit failure.
INTRODUCTION
The primary objective for the emergency physician (EP) in the evaluation of patients with abdominal pain is to detect conditions requiring urgent surgical intervention, because prompt recognition might obviate the potential morbidity and mortality associated with delays in diagnosis. Although conditions such as acute appendicitis generally require prompt operative intervention, surgeons often manage presumed partial bowel obstruction and adynamic ileus expectantly with observation and serial examinations. The goals of this exploratory study were to identify characteristics predictive of ultimate disposition and to assess whether it is useful to manage such patients in the emergency department (ED) observation unit (OU) setting.
METHODS
This was a retrospective review of adult OU admissions from January 1999 through November 2004. Inclusion criteria were adult patients admitted to the OU with an ED diagnosis of ileus, partial small bowel obstruction (PSBO), or small bowel obstruction (SBO), and electronic medical records available for review. Eligible admissions from January 1999 through July 2000 were identified through review of handwritten patient logs. The patients admitted to the OU for the remainder of the study period were identified through the ED electronic tracking system (EmStat 2.8.5; Allscripts 4A Health Systems, Chicago, Illinois) for the ICD-9 diagnostic codes 560.1 (Paralytic ileus) and 560.9 (Unspecified intestinal obstruction). Patients were admitted to the OU solely at the discretion of the attending EP, with no specific criteria required and with no standard order set or care pathway established for such patients. During the study period, the admitting diagnoses of ileus, PSBO, and SBO accounted for fewer than 0.3% of all OU admissions.
The charts were independently reviewed by 2 of the investigators for the following data points: age, sex, number of prior surgeries, recent surgery within 4 weeks of presentation, record of prior similar admission in the institution’s medical record, serum potassium level in the ED, use of nasogastric decompression or opiate analgesics, presence of an enterocutaneous stoma, presence of dilated loops of small bowel (DLSB) or air–fluid (AF) levels on plain abdominal radiograph, surgical service following the patient’s case in consultation, disposition, and time in the OU. Hypokalemia was defined as a serum potassium level of less than 3.5 mEq/L. Treatment failure was defined as inpatient hospitalization from the OU. Data missing from the medical record were recorded as missing. For univariate analysis, alpha was defined as 0.004 by the Bonferroni correction (0.05 divided by 12 variables). Results were recorded on a standardized Excel spreadsheet (Microsoft Office 2003, Redmond, Washington). Data were analyzed with the SAS software (Version 9.1, Cary, North Carolina) and Open Source Epidemiologic Statistics for Public Health, (Version 2.3.1;www.OpenEpi.com), with the primary outcome measure defined as treatment failure versus discharge home from the OU. The study was approved by our local institutional review committee.
RESULTS
In total, 137 OU admissions were identified by observation unit log and ICD-9 search of the computerized data base, accounting for approximately 0.3% of all OU cases during the study period. Six were excluded because their ED diagnosis was obstipation or presumed large bowel obstruction. One patient each was excluded for being younger than 18 years and having an incomplete medical record. The remaining 129 patients were analyzed. Studied data points and their association with hospitalization after an ED OU admission are presented in Table 1.
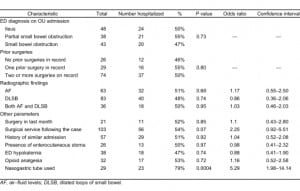
Of the 129 patients, 70% were women. Mean age was 56.5, with a standard deviation of 17.3 years. Admitting diagnosis to the OU was evenly distributed between ileus, PSBO, and SBO (37%, 29%, and 33%, respectively). Among the historical factors, similar admission in the medical record had no impact on need for admission (P = 0.9212). A majority of patients (103 of 129, 79%) had a history of abdominal surgery, with 74 of 129 (57%) having had 2 or more procedures. Twenty-one (16%) patients were seen within 4 weeks of abdominal surgery. Neither remote surgeries nor surgery in the last 4 weeks was associated with an increased rate of admission (P = 0.80 and 0.84, respectively).
Neither hypokalemia nor the presence of an enterocutaneous stoma was predictive of disposition (P= 0.74 and 0.96, respectively). Radiographic findings were likewise not predictive. (For AF, P = 0.68; for DLSB, P = 0.74; for both AF and DLSB, P = 0.94.) Admitting diagnosis from the ED had no correlation with ultimate disposition (P = 0.73).
With regard to management variables, the administration of any opioid analgesics was not predictive of ultimate disposition (P = 0.72). Patients who had a nasogastric tube (NGT) placed had a higher rate of inpatient admission (P = 0.0004; odds ratio [OR], 5.294; confidence interval [CI], 1.982–14.14). For the majority of patients (80%) who had surgical service consultation, a trend was noted toward hospital admission (P = 0.07; OR, 2.251; CI, 0.9186–5.514).
Overall, 65 (50%) of 129 patients were admitted. Average length of stay in the OU was 13.77 ± 7.3 hours. No deaths occurred in the study group. Two patients were found to have acute pathology requiring operative intervention, 1 with a perforated duodenal ulcer, and 1 with a perforated appendicitis.
DISCUSSION
We found that 50% of patients admitted to our ED OU with presumed diagnoses of ileus or varying degrees of SBO were successfully managed, defined as discharged within 24 hours from the OU. Patients treated with nasogastric decompression were more likely to require hospitalization. No other parameter reliably predicted outcomes, although a trend was seen toward failure of observation for patients followed up in consultation by surgical services.
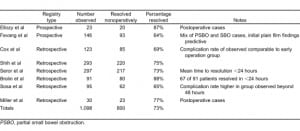
Multiple studies have demonstrated that a period of inpatient observation and serial examinations is a safe initial management approach for varying degrees of SBO.1–8 In Table 2, we summarize the published literature. Of a total of 1,098 patients, 73% resolved nonoperatively. In the Seror5 and Brolin6 series, patients who improved nonoperatively tended to declare themselves in less than 24 hours. Complications were associated with longer periods of observation.7 Although our rate of OU success was lower at 50%, no deaths occurred, and only 2 patients required early operative intervention.
Most of these cases that supported observation as a viable initial management option cited use of nasogastric decompression for the majority of patients in their nonoperative cohorts.1,2,7,8 NGT decompression was used in only 22% of our cases. This may reflect a lower overall acuity for our patients, or that surgical consult services tended to admit patients directly from the ED who were perceived as more ill. Another possibility is that cases of PSBO, intuitively more likely to resolve without nasogastric decompression than those with more-advanced degrees of obstruction, were actually more predominant in our cohort than the distribution of reported admitting diagnoses would suggest (that is, some PSBO cases were labeled as SBO). NGT use was the only factor examined that had any association with disposition for our patients, and paradoxically was associated with OU failure and subsequent hospitalization. As the use of NGT was not randomized, no causal relation should be inferred; our findings may reflect that OU patients who had an NGT placed were more ill, or the fact that it necessarily took longer to advance diet in these patients.
Although only half of our patients were discharged home within 24 hours, ancillary benefit may be derived from using the ED observation unit for management of varying degrees of ileus or SBO. Operationally, observation provides the opportunity to offload the ED and improve throughput by identifying patients with concern for obstruction early in their course; they might benefit from OU admission, so that time-consuming additional imaging studies (for example, computed tomography scan) and consultation are completed in an environment with less competition for bed space than a busy ED. Any concern for inefficiency about a 50% admission rate for these patients must be weighed against improved ED efficiency from bed turnover, which, by decreasing wait times, can positively affect patient satisfaction and patient safety.9
Future analyses should include a comparison of outcomes between patients observed in the ED observation unit versus those admitted directly to an inpatient bed from the ED, as the initial admitting service may affect multiple metrics. Malangoni et al10 examined the impact of admitting service on outcomes in 336 inpatient SBO admissions. Of these, 222 were admitted to surgical services, whereas 114 patients were admitted to medical services, with surgeons following along in consultation in 75% of cases. Factors associated with admission to medical services included presence of diarrhea and lack of prior abdominal surgery. Lengths of stay were shorter for patients admitted to surgical services who ultimately required operative intervention. Lengths of stay were similarly shorter for patients admitted to nonsurgical services who improved without operative intervention. A trend appeared toward higher numbers of complications in the patients admitted to nonsurgical services, and patients with complications had longer lengths of stay. Patients who went to surgery within 24 hours had overall lower lengths of stay, lower mortality, and were more likely to be have been admitted to surgical services.
LIMITATIONS
Limitations of our analysis include its retrospective design and the possibility of incomplete records. With regard to chart abstraction, several previously published guidelines for retrospective reviews were not followed; specifically, the 2 reviewers were not blinded to each other’s findings, were not trained in abstraction methods, and were not monitored for performance. Last, their interrater reliability was not measured.11 Medication administration records were not reviewed, and the potential impact on disposition was not defined. Radiographic interpretation was not standardized. The parameters selected for analysis were not literature based. Finally, the number of postoperative cases in our series was low, reflecting either higher acuity or a selection bias by the surgical services to admit their patients directly to inpatient beds.
CONCLUSION
To our knowledge, this is the first study in the emergency medicine literature regarding the evaluation and outcomes of patients with ileus or degrees of SBO admitted to an emergency department observation unit. Approximately half of the patients in our study required hospital admission. The requirement of a NGT in such patients was associated with a greater rate of observation unit failure. Future investigations should compare outcomes for such patients managed in the OU versus those admitted directly to an inpatient service.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted January 3, 2011; Revision received February 21, 2011; Accepted March 23, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.3.2175
Address for Correspondence: Steven T. Dorsey, MD
Emergency Services Institute, Cleveland Clinic, 9500 Euclid Ave, Cleveland, OH 44195
E-mail: dorseys1@ccf.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Ellozy SH, Harris MT, Bauer JJ, et al. Early postoperative small-bowel obstruction: a prospective evaluation in 242 consecutive abdominal operations. Dis Colon Rectum. 2002;;45:1214–1217.[PubMed]
2. Fevang BT, Jensen D, Svanes K, et al. Early operation or conservative management of patients with small bowel obstruction? Eur J Surg. 2002;;168:475–481. [PubMed]
3. Cox MR, Gunn IF, Eastman MC, et al. The safety and duration of non-operative treatment for adhesive small bowel obstruction. Aust N Z J Surg. 1993;;63:367–371. [PubMed]
4. Shih SC, Jeng KS, Lin SC, et al. Adhesive small bowel obstruction: how long can patients tolerate conservative management? World J Gastroenterol. 2003;;9:603–605. [PubMed]
5. Seror D, Feigin E, Szold A, et al. How conservatively can postoperative small bowel obstruction be treated? Am J Surg. 1993;;165:121–126. [PubMed]
6. Brolin RE. Partial small bowel obstruction. Surgery. 1984;;95:145–149. [PubMed]
7. Sosa J, Gardner B. Management of patients diagnosed as acute intestinal obstruction secondary to adhesions. Am Surg. 1993;;59:125–128. [PubMed]
8. Miller G, Boman J, Shrier I, et al. Readmission for small-bowel obstruction in the early postoperative period: etiology and outcome. Can J Surg. 2002;;45:255–258. [PubMed]
9. Ross MA, Graff LG. Principles of observation medicine. Emerg Med Clin North Am. 2001;;19:1–17.[PubMed]
10. Malangoni MA, Times ML, Kozik D, et al. Admitting service influences the outcomes of patients with small bowel obstruction. Surgery. 2001;;130:706–711. [PubMed]
11. Gilbert EH, Lowenstein SR, Koziol-McLain J. et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;;27:305–308.


