| Author | Affiliation |
|---|---|
| Namita Jayaprakash, MB BCh BAO | St. Vincent’s University Hospital, Department of Emergency Medicine, Dublin, Ireland |
| Ronan O’Sullivan, MB BCh | Our Lady’s Children’s Hospital Crumlin, Department of Emergency Medicine, Dublin, Ireland |
| Tareg Bey, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Suleman S. Ahmed, BS, BA | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Shahram Lotfipour, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
ABSTRACT
Emergency department (ED) crowding is a multifactorial problem, resulting in increased ED waiting times, decreased patient satisfaction and deleterious domino effects on the entire hospital. Although difficult to define and once limited to anecdotal evidence, crowding is receiving more attention as attempts are made to quantify the problem objectively. It is a worldwide phenomenon with regional influences, as exemplified when analyzing the problem in Europe compared to that of the United States. In both regions, an aging population, limited hospital resources, staff shortages and delayed ancillary services are key contributors; however, because the structure of healthcare differs from country to country, varying influences affect the issue of crowding. The approach to healthcare delivery as a right of all people, as opposed to a free market commodity, depends on governmental organization and appropriation of funds. Thus, public funding directly influences potential crowding factors, such as number of hospital beds, community care facilities, and staffing. Ultimately ED crowding is a universal problem with distinctly regional root causes; thus, any approach to address the problem must be tailored to regional influences.
INTRODUCTION
Emergency department (ED) crowding is a global problem that has drawn increasing international attention.1 The nature of emergency medicine (EM) has changed significantly in recent years with the advent of new treatment options and the availability of more medical technology, such as specialized intravenous thrombolysis in stroke, stent placement in acute myocardial infarction, and the use of ultrasound. Many of these are time-critical procedures, leading to greater emphasis on the resuscitation, stabilization, investigation and initial management in the ED. Conditions for which patients were previously admitted and observed are now managed in the ED, allowing for direct discharge without the added cost of inpatient hospitalization. In the United States (U.S.), EDs are required to provide appropriately resourced 24-hour emergency care, 365 days a year. There is a direct correlation between an aging population and increased utilization of emergency services.2
The precise definition of crowding is unclear. Some define it as an inability of ED staff to deliver optimal care because of work overload. Others believe it to be accurately assessed through quality indicators, such as waiting times, treatment times and actual patient census, while trying to provide the best care, service and safety.3 The American College of Emergency Physicians (ACEP) Crowding Resources Task Force has adopted this definition of ED crowding:
“…a situation in which the defined need for emergency services outstrips available resources in the ED…occurs in hospital EDs where there are more patients than staffed ED treatment beds and wait times exceed a reasonable period.”4
The concept of crowding has been difficult to define scientifically. Documentation was once limited to photographs of congested EDs and anecdotes over empirical data. In recent times more efforts have been made to document the problem. Derlet et al.5 surveyed ED directors nationwide to describe the definition, extent and factors associated with the problem as perceived by them. They identified an array of issues as reasons for crowding: increased patient acuity, hospital bed shortage, increasing ED volume, radiology delays, insufficient ED space, laboratory delays, consultation delays, nursing shortage, physician shortage and managed care issues. A qualitative Irish study6described the problem from the point of view of patients and/or relatives/significant others who had spent 12 hours or more in the ED awaiting admission. Descriptions by the participants of this study portrayed an ED that was overcrowded, dirty, lacking in resources and resembling a disaster zone or hospital scene from a Third World country.
Weiss et al.7 attempted to quantify crowding through the National ED OverCrowding Study (NEDOCS). The NEDOCS score was calculated using institutional constants: number of ED beds and number of hospital beds. This was combined with model variables: total patients in the ED, total admits in the ED, number of respirators in the ED, longest admit time (in hours), and waiting room time of last patient put in bed (in hours). They determined that the NEDOCS score (0–20 = not busy, 20–60 = busy, 60–100 = extremely busy but not overcrowded, 100–140 = overcrowded, 140–180 = severely overcrowded, 180–200 = dangerously overcrowded) was a useful indicator of the degree of crowding and could be used reliably to determine the status of an ED at any given time. In 1999, 91% of ED directors in the U.S. reported crowding as a problem, defining it by the presence of patients in hallways, occupied ED beds, full waiting rooms > 6 hours/day, and acutely ill patients waiting > 60 minutes to see a physician.5 A recent study by McCarthy et al.8 showed that ED occupancy rate (total number of patients in the ED divided by total number of licensed beds) can serve as a valid measure of crowding.
International studies have shown that where a patient is waiting in the ED beyond the time the decision is made to admit, clinical outcomes are adversely affected.9–11 This correlates to the reality that EDs cannot adequately fulfil their primary function of stabilization and disposition while also functioning as an inpatient ward. As a result, both functions are performed suboptimally with consequent predictable adverse effects on patient outcome.
FACTORS THAT INFLUENCE CROWDING ACROSS EUROPE
EM across Europe is still in a developing state with many European countries having yet to form their own EM societies or have dedicated EM journals. The Casualty Surgeons Association was formed in the United Kingdom (UK) in 1967. The name was changed in 1990 to the British Association of Accident and Emergency Medicine and then again in 2004 to the British Association for Emergency Medicine (BAEM). A collaboration of BAEM and the Faculty of Accident and Emergency Medicine (formed in 1992) developed the College of Emergency Medicine in 2005.12 In the UK and Ireland, the ED is sometimes referred to as “casualty” or the “accident and emergency department.”
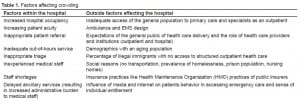
The majority of studies looking at quantifying ED crowding have emerged from the U.S. and Australasia. In Europe, as in the U.S., the problem is multifactorial (Table 1), and the issue is becoming one of major societal concern.13
Increased Hospital Occupancy
One of the most significant reported causes of ED crowding is hospital bed shortage, especially ICU and telemetry beds.3,5,14,15 The ability to move admitted patients from the ED to hospital beds depends upon the availability of hospital beds, nursing staff, nursing ratios, ancillary service availability, local structure and likely many other factors. Hospitals in the UK and Ireland are faced with the situation in which elective and emergency admissions compete for bed occupancy. In these countries the typical picture is one in which elective surgical patients are often brought in over the weekend for procedures scheduled to occur later in the week. Thus, beds are occupied and made unavailable to admissions from the ED. A similar situation in the U.S. may exist (although not studied extensively), as it has been shown that each additional elective surgical admission is associated with a prolonged daily mean length of stay for all ED patients.16 In the UK, it has been shown that the total time spent in EDs, even for patients who are discharged, is related to hospital bed occupancy rates and has negative effects on patient satisfaction and the economic bottom line of the hospital.17
According to an Irish government report entitled “Acute Hospital Bed Capacity: A National Review,” the number of acute hospital beds in 2000 (11,832) was approximately 6,000 lower than that in 1980 (17,655).18 The report also documents that the number of acute hospital beds per capita in Ireland – 3.1 beds per 1,000 population compared to 5.1 per 1,000 in 1980 – is one of the lowest among the European Union (EU) and the Organization for Economic Cooperation and Development (OECD) countries. Germany has also reduced the number of hospital beds. Closure of German hospitals resulted in 49,472 fewer hospital beds between 1995 and 2000 alone, bringing the available bed count to 559,651 (6.8 per 1,000) in the year 2000.19 This trend continued in 2006, when Germany cut another 13,000 hospital beds (or 2.5%), decreasing the total to 511,000 nationally (6.2 per 1,000).20
In one study conducted at a large Irish ED with an annual census of 45,000 patients, over half reported that lack of beds contributed to their prolonged ED stay.21 In the same study 85.9% of patients felt that health authorities were not doing enough to address the crowding issue and over 35% reported that the prospect of a prolonged stay affected their willingness to come to the ED or to return. This latter finding may be particularly important, as there are no real alternatives to ED-delivered emergency care in Ireland, thus raising the possibility that a prior adverse experience might lead to a subsequent delay in future emergency care. According to a study conducted in the U.S., as hospital occupancy increased by 10% the median ED length of stay increased by 18 minutes.22
Factors affecting bed occupancy also include those that lie outside the hospital. Inadequate community services for appropriate transfer of care of patients back to the community leads to prolonged stays in the hospital and blocks acute hospital bed access.23 The recently published report by the Irish Health Service Executive (HSE) identified patients who were clinically discharged but unable to leave the hospital due to lack of community services for continuation of care.24 These facilities are dependent on public funding and limitations on the availability of funds prolong hospital stay and decrease the numbers of available hospital beds. This in turn affects the transfer of patients out of the ED. An estimated 12% of hospital beds are unavailable due to delayed discharges. The equivalent of 675 beds could be made available in acute care hospitals if such measures as improving long term care and rehabilitation facilities, were put in place to improve delays in discharge. One of the authors reported that there are two types of patients in Irish hospitals, those awaiting tests and procedures and those waiting for non-acute, long stay and rehabilitation care.
In 2007 the American Hospital Association published figures suggesting there were 3.1 hospital beds per 1000 population.25 This places the U.S. within the same range as Ireland, which has one of the lowest averages among EU countries. The difference between the two countries is the greater U.S. emphasis on delivery of critical care medicine. From 1985 to 2000, there was a 6% decrease in the ratio of non-critical care medicine (CCM) beds to hospital beds and a 71.5% increase in the CCM beds to hospital-beds ratio.26 This equated to a 6.7% decrease in the number of inpatient days for non-CCM patients and a 75.2% increase in CCM inpatient days, which reflects the increasing shift in U.S. hospitals towards the delivery of CCM.
Increasing Patient Acuity
As the population ages, the type of patient presenting to the ED has changed. One study conducted in the UK showed that between 1990 and 2004 the median age of the population increased by 10 years.2 It also showed that in 2004 the proportion of patients presenting to EDs who were 70 years or older was 198% higher than in 1990, and the proportion of patients 90 years or older was 671% higher. The elderly were more often admitted to the hospital and once admitted had a greater length of stay compared to younger patients, an effect attributed to acute exacerbations of chronic diseases that require emergent care. Increasing numbers of patients have co-morbidities that prolong evaluation and patient waiting time,3 hence resulting in back logs of patients waiting to be seen.
Patient Self-Referral
In countries such as Germany, Ireland, Italy, Netherlands, Norway, Portugal, Spain, Switzerland and the UK, the general practitioner (GP) acts as a gatekeeper to health services whose role is primary health carer. In Europe, as in the U.S., 80 to 90 percent of health-related activities, including diagnosis and treatment, are initiated by the patients themselves, without seeking professional advice.27 Increasing numbers of patients across Europe are bypassing the GP and primary healthcare system to present to EDs.28
Overuse of the ED for minor complaints that could be dealt with at the GP level decreases the quality of care and increases ED costs.28 A study conducted by Lee et al.29 found that 57% of ED attendees were primary care cases. Reasons for ED attendance over GP attendance include a lack of confidence in the primary healthcare system, inadequate out-of-hours services, and unavailability of care through GPs.28
Inadequate Out-of-Hours Services
Where GPs act as gatekeepers to healthcare systems, they are expected to be available as points of contact 24 hours a day. Different GP groups provide various forms of after-hours service, but there is no uniform system and no guarantee of coverage in every area. When access is unavailable a patient’s only option is the ED. Inadequate after-hours GP services are thus adding to the numbers of patients presenting to the ED. A study conducted by van Uden et al.30 concluded that an after-hours service that optimized the role of the GP as gatekeeper and geared itself towards the patients’ symptoms enabled primary care patients to be dealt with by a GP, thus reducing inappropriate referrals to the ED.
Certain initiatives have attempted to offer alternatives of care to patients requiring urgent treatment. The UK National Health Service (NHS) has developed physician and/or nurse-led minor injury units, urgent care centers and telephone advice systems, such as NHS Direct.31 However, initial evidence from these initiatives would suggest that they have had little impact on ED attendances and waiting times.
Triage in the Emergency Department
A system of ED triaging organizes patients into recognizable groups to prioritize the sickest patients. In the U.S., the commonly accepted “prudent layperson law” in essence requires that the emergent nature of a presentation be judged by the patient’s initial presentation rather than the eventual diagnosis. Furthermore, according to this law, whether the presentation warrants immediate attention should be judged by the patient.32 In contrast, in places such as the UK, the triage system is based on clinical assessment at the pre-hospital level, on arrival at an ED and by the first attending physician.33 A study conducted by Gersenz and Studdert34 found a discrepancy between lay and expert judgments about what constitutes emergency care, a situation underscored by the significant number of ED cases in insurance payment disputes.
Studies in the UK have found that the accepted five-category triage is not being used in practice; instead they use a three-category triage system that simply assigns patients as “life-threatening”, “major”, and “minor.”35 This nurse-led three-category triage system, which provides little more information than one could ascertain without clinical evaluation, is time consuming and leaves patients most amenable to treatment in a waiting room while those patients judged more critical are seen first.36
In 2002 the NHS Modernisation Agency in the UK proposed a system of “see and treat,” which suggested abandoning triage and adopting a method in which patients are seen and treated by senior clinical physicians as early as possible.37 As soon as patients arrive at the ED they are seen, assessed, treated, admitted or discharged by one physician. Several studies have shown that the earlier a person is seen in the ED by a senior clinician the shorter the length of stay.31 It is now widely accepted across the NHS that triage is an exercise of prioritization that needs to be executed when there is a delay in seeing the practitioner.
Other NHS initiatives, such as “streaming,” or “triage-out,” assess patients at the point of triage and direct them to appropriate services. An experienced member of the nursing staff assesses whether the ED medical staff, an ED nurse or a member of the primary healthcare team best meets the patient’s needs. The nurse can then direct the patient to the appropriate service. Audits have shown that the use of such initiatives have reduced patient complaints and increased job satisfaction amongnurses.31
Inexperienced Medical Staff
Across the EU, medical education generally includes 5–7 years of undergraduate medical training with 1–2 years of initial training as a house officer followed by 4–8 years of specialist training.38,39In Ireland, for example, medical school consists of five years, followed by one year as a house officer, which is similar to that of a first year intern with broad-based introductory training. The first year is followed by a three-year period as a senior house officer with generalist training (although one can emphasize emergency medicine), after which there are five years of higher specialist training (specialist registrar). Finally, the physician passes an exit examination and becomes a consultant, which is equivalent to full American Board of Emergency Medicine certification conferring attending-physician status.40 Junior doctors, such as a senior house officer, play an integral role in seeing and treating patients in the ED; however, they lack the experiences and expertise of more senior staff members (consultants). Experienced doctors spend less time with patients and order fewer studies to arrive at clinical decisions, while inexperienced doctors are slower in decision making.35 In the UK (population 60 million) there are currently 749 consultant posts in EM, while in Ireland (population 4 million) there are currently 59 consultants in EM, working in 35 EDs. In contrast, there are over 22,000 board-certified emergency physicians in the U.S. (population 282 million). Patients treated by experienced medical personnel have reduced time to medical assessment, laboratory examination, radiology and discharge.36
Staff Shortages
Reports suggest that nursing shortages worldwide are a cause of ED crowding.5 Across the EU there is an average of 3.4 doctors per 1000 population.38 In the U.S., between 1980 and 2000, the population grew from 227 million to 282 million and this is projected to increase to 420 million by 2050. Medical school enrollments, however, have remained constant from 1980 to 2005 .41 This would result in an increasing shortage of physicians in coming years.
Delayed Ancillary Services
Emergency radiology is essential in the rapid diagnosis of patients, implementation of treatment, and final decision on the patient’s status. Thus, delays in getting imaging result in delayed assessments and prolonged stays within the ED, especially in the case of trauma patients.42 Similarly, delays in lab reports reporting lab findings also mean patients unnecessarily occupying ED beds, prolonging wait time and decreasing patient satisfaction.
STRUCTURE OF HEALTHCARE IN EUROPE
Emergency department crowding is a universal problem. While several factors that contribute to crowding in Europe are comparative to factors in the U.S., differences in the structure of healthcare between these regions of the world have varying influences.
In Europe, unlike in the U.S., healthcare is viewed as a utility with equal access to the whole population, as opposed to a free-market commodity with supply and demand influencing access to care. All European countries have a legal framework of healthcare delivery for the general population. It is planned and administered centrally by the respective government ministries with a variety of delivery systems. For example, in France and the UK the system is controlled centrally with management directly responsible to the Ministry of Health. In Germany, Italy and Spain the healthcare delivery system is decentralized and local government bodies have the autonomy to pass their own legislation.19,27 In Ireland, delivery of health services is the responsibility of the HSE, while the Department of Health and Children oversees the development and overall strategic management of the health system in accordance with legislation.43
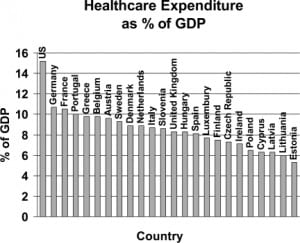
For the provision of their healthcare, EU member states rely predominantly on public funding sources, such as taxation or health insurance premiums. Direct out-of-pocket expenditure with private health insurance represents a small proportion of the funding.44 While the U.S. spent 15.2% of its Gross Domestic Product (GDP) on healthcare in 2004, the EU average was 9.43% (Figure 1).45,46 Despite this, the share of public spending on health in the U.S. is 45% compared to well over 80% in the UK and parts of Scandinavia. Public insurance covered just 26.2% of the U.S. population in 2005,47 In contrast to many EU countries where healthcare is a public utility with access to all, the U.S. healthcare system is fragmented and market-driven. Multiple purchasers allow healthcare costs to rise above those of other industrialized countries. Further, the increased administrative overhead required to manage the complex financial system utilizes a high fraction of U.S. spending.48 Ultimately this results in a greater out-of-pocket expenditure for the individual and less dependence on public funding.
In Europe, because healthcare is planned and administered by a central body, policies that affect crowding can be implemented universally. In England, for example, the Department of Health launched the National Health Service Plan, a policy declaring that the total time for a patient in the ED be no more than four hours.49 Implemented in 2003, the plan was to address the perceived shortcomings in the UK ED system and achieve efficiency.50 With this four-hour target came support systems, such as the Modernization Agency and other government resources, to build capacity, support performance and aid in compliance.51–53 Despite the struggle to achieve this target, massive transformations have occurred and the outcome has been largely positive.53 Muran et al.54found waiting times reduced and Banerjee et al.55 concluded that “long waits in the ED are a thing of the past in the UK.” While implementing a similar plan in the U.S. would seem difficult without a central regulatory body and major support systems to increase bed capacity and support staff, the U.S. may be able to adopt some effective aspects of the four-hour target, such as coordination throughout a hospital system, rather than having crowding be the burden of one department.
CONCLUSION
The issue of ED crowding has been brought to the forefront of healthcare, and newspaper photos of patients waiting on gurneys have become a political standpoint for election candidates. The problem has been attributed to many factors, some universal and others specific to certain regions of the world. Overcrowded EDs lead to adverse clinical outcomes. Patient dissatisfaction is increased as waiting times are prolonged and resources are stretched.
To begin to address crowding, the root of the problem has to be determined. There is no single cause and effect scenario; instead there are many causes depending on the region of the world and the governing healthcare system. Within the EU increased hospital occupancy, bed shortages, increased patient acuity, staff shortages and delayed ancillary services are all contributing factors, as in the U.S. However, differences in healthcare delivery between the two regions result in a common problem with different roots. The European approach to healthcare as a utility with equal access for everyone and not a free market commodity requires centralized management of healthcare and governments that ensure that adequate allocation of funds for acute hospital and community supports. In the U.S. however, supply and demand influences the availability of health resources, and the proportion of public spending is significantly less.
The problem of crowding in the ED is one that affects both Europe and the U.S. The ED is the gateway to the hospital; problems arising there have the potential to affect the entire hospital. Because ED crowding has different regional causes, any potential solutions must be tailored to regional variations. These differences suggest that while a universal solution is not necessarily practical, we can look at various policies that have had a positive impact on crowding and implement similar solutions across countries, tailored to the needs of individual regions.
Footnotes
Supervising Section Editor: Chris Mills, MD, MPH
Submission history: Submitted October 5, 2008; Revision Received August 14, 2009; Accepted September 30, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Shahram Lotfipour, MD, MPH, Department of Emergency Medicine, University of California Irvine School of Medicine, 101 The City Drive, Rte 128-01 Orange, CA 92868
Email: SHL@uci.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Sinclair D. Emergency department crowding – implications for paediatric emergency medicine.Paediatr Child Health. 2007;12:491–4. [PMC free article] [PubMed]
2. George G, Jell C, Todd BS. Effect of population ageing on emergency department speed and efficiency: a historical perspective from a district general hospital in the UK. Emerg Med J.2006;23:379–83. [PMC free article] [PubMed]
3. Derlet RW, Richards JR. Crowding in the nation’s emergency departments: Complex Causes and Disturbing Effects. Ann Emerg Med. 2000;35:63–7. [PubMed]
4. Schneider SM, Gallery ME, Schafermeyer R, et al. Emergency department crowding: A Point in Time. Ann Emerg Med. 2003;42:167–72. [PubMed]
5. Derlet RW, Richards JR, Kravitz RL. Frequent crowding in US emergency departments. Acad Emerg Med. 2001;8:151–5. [PubMed]
6. Coughlan M, Corry M. The experiences of patients and relatives/significant others of crowding in accident and emergency in Ireland: A qualitative descriptive study. Accid Emerg Nurs.2007;15:201–9. [PubMed]
7. Weiss SJ, Derlet R, Arndahl J, et al. Estimating the degree of emergency department crowding in academic medical centers: results of the National ED crowding study (NEDOCS) Acad Emerg Med.2004;11:38–50. [PubMed]
8. McCarthy ML, Aronsky D, Jones I, et al. The emergency department occupancy rate: a simple measure of emergency department crowding. Ann Emerg Med. 2008;51:15–24. [PubMed]
9. Richardson D. Increase in patient mortality at 10 days associated with emergency department crowding. Med J Aust. 2006;184:213–6. [PubMed]
10. Sprivulis PC, Silva JD, Jacobs IG, et al. The association between hospital crowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust.2006;184:208–12. [PubMed]
11. Cameron PA. Hospital crowding: a threat to patient safety? Managing access block involves reducing hospital demand and optimising bed capacity. Med J Aust. 2006;184:203–4. [PubMed]
12. Bloomfield J. BAEM – emergency medicine landmark British Association for Emergency MedicineAvailable at: www.emergencymed.org.uk Accessed March, 2008.
13. Donnellan E. Making beds for those in need. Irish Times. Nov 25, 2008.
14. Krall S, O’Conner RE, Maercks L. Higher inpatient medical surgical bed occupancy extends admitted patients stay. West J Emerg Med. 2009;10:93–6. [PMC free article] [PubMed]
15. O. Miró M, Sánchez G, Espinosa B, et al. Analysis of patient flow in the emergency department and the effect of an extensive reorganisation. Emerg Med J. 2003;20:143–8. [PMC free article] [PubMed]
16. Rathlev N, Chessare J, Olshaker J, et al. Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med. 2007;49:265–271. [PubMed]
17. Cooke MW, Wilson S, Halsall J, et al. Total time in English accident and emergency departments is related to bed occupancy. Emerg Med J. 2004;21:575–6. [PMC free article] [PubMed]
18. Department of Health and Children Dublin: 2002. Acute hospital bed capacity a national review.
19. Platz E, Bey T, Walter FG. International report: current state and development of health insurance and emergency medicine in germany. the influence of health insurance laws on the practice of emergency medicine in a European country. J Emerg Med. 2003;25(2):203–210.[PubMed]
20. Höhere Auslastung der Krankenhausbetten. 2006. Available at:http://www.destatis.de/jetspeed/portal/cms/Sites/destatis/Internet/DE/Presse/pm/2007/09/PD07__350__231 Accessed January 29, 2008.
21. Gilligan P, Gupta V, Singh I, et al. Why are we waiting? A study of the patient’s perspectives about their protracted stays in an emergency department. Ir Med J. 2007;100:627–9. [PubMed]
22. Forster AJ, Stiell I, Wells G, et al. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med. 2003;10:127–32. [PubMed]
23. Cooke MW. Reforming the UK emergency care system. Emerg Med J. 2003;20:113–4.[PMC free article] [PubMed]
24. PA Consulting Group Health Service Executive. Dublin: 2008. Acute hospital bed capacity review: a preferred health system in Ireland to 2020.
25. American Hospital Association Fast facts on U.S. hospitalsHealth Forum LLC. April 13, 2009. Available at: http://www.aha.org/aha/resource-center/Statistics-and-Studies/fast-facts.htmlAccessed August 12, 2009.
26. Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985–2000: An analysis of bed numbers, use, and costs. Crit Care Med. 2004;32:1408–9. [PubMed]
27. Jepson GMH. How do Primary Health Care systems compare across Western Europe? Pharm J.2001;267:269–73.
28. Rieffe C, Oosterveld P, Wijkel D, et al. Reasons why patients bypass their GP to visit a hospital emergency department. Accid Emerg Nurs. 1999;7:217–25. [PubMed]
29. Lee A, Lau F, Hazlett CB, et al. Measuring the inappropriate utilization of accident and emergency services? Int J Health Care Qual Assur. 1999;12:287–92.
30. van Uden CJT, Winkens RAG, Wesseling GJ, et al. Use of out of hours services: a comparison between two organisations. Emerg Med J. 2003;20:184–87. [PMC free article] [PubMed]
31. Cooke MW, Fisher J, Dale J, et al. Reducing attendances and waits in emergency departments: a systematic review of present innovations Report to the National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO) Warwick: The University of Warwick; 2004.
32. Hall MA. The Impact and Enforcement of Prudent Layperson Laws. Ann Emerg Med.2004;43:558–66. [PubMed]
33. Robertson-Steel I. Evolution of triage systems. Emerg Med J. 2006;23:154–5. [PMC free article][PubMed]
34. Gresenz CR, Studdert DM. Disputes over coverage of emergency department services. a study of two health maintenance organizations. Ann Emerg Med. 2004;43:155–62. [PubMed]
35. Gunal MM, Pidd M. Understanding Accident and Emergency Department performance using simulation. Proceedings of the 2006 Winter Simulation Conference. 2006.
36. Subash F, Dunn F, McNicholl B, et al. Team triage improves emergency department efficiency.Emerg Med J. 2004;21:542–4. [PMC free article] [PubMed]
37. BAEM The way ahead 2005 London: BAEM, CEM; Available at:www.emergencymed.org.uk/baem Accessed March 1st, 2008.
38. Directive 2005/36/EC of the European Parliament and of the Council of 7 September 2005 on the recognition of professional qualifications Official Journal of the European Communities 2005. L255/22–142.142Available at: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CONSLEG:2005L0036:20081211:EN:PDF Accessed July 11, 2009.
39. Dick WF. Anglo-American vs. Franco-German emergency medical services system. Prehosp Disaster Med. 2003;18:29–35. [PubMed]
40. McHugh DF, Driscoll PA. Accident and emergency medicine in the United Kingdom. Ann Emerg Med. 1999;33:702–9. [PubMed]
41. Williams TE, Jr, Ellison EC. Populaiton analysis predicts a future critical shortage of general surgeons. Surgery. 2008;144:548–54. [PubMed]
42. Miele V, Andreoli C, Grassi R. The management of emergency radiology: key facts. Eur J Radiol.2006;59:311–314. [PubMed]
43. Irish College of General Practitioners What is the structure of Irish healthcare?Available at:www.icgp.ie Accessed September 9, 2007.
44. Ryden L, Stokoe G, Breithardt G, et al. Patient access to medical technology across Europe. Eur Heart J. 2004;25:611–16. [PubMed]
45. Davis K, Schoen C, Guterman S, et al. Slowing the growth of u.s. health care expenditures: what are the options?. 2007 Bipartisan Congressional Health Policy Conference: The Common Wealth Fund; 2007.
46. Kerem K, Puss T, Viess M, et al. Health and convergence of health care expenditure in EU 2007. EABR (Business) & ELTC (Teaching) Conference. Ljubljana, Slovenia; 2007. Available at:www.cluteinstitute.com Accessed September, 2007.
47. Anderson GF, Frogner BK. Health spending in oecd countries: obtaining value per dollar. Health Aff. 2008;27:1718–27.
48. Reinhardt UE, Hussey PS, Anderson GF. US health care spending in an international context.Health Aff. 2004;23:10–25.
49. Department of Health London, UK: Crown; 2000. The NHS plan: a plan for investment, a plan for reform.
50. Gautam V. International perspective from the united kingdom on “surgeons’ and emergency physicians’ perceptions of trauma management and training.” West J Emerg Med. 2009;10:150–1.[PMC free article] [PubMed]
51. Departmen of Health Richmond, Surrey UK: Crown; 2007. Modernization Agency.
52. Proudlove NC, Gordon K, Boaden R. Can good bed management solve the crowding in accident and emergency departments? Emerg Med J. 2003;20:149–55. [PMC free article] [PubMed]
53. Cronin JG, Wright J. Breach avoidance facilitator – managing the A&E 4-hour target. Accid Emerg Nurs. 2006;14:43–8. [PubMed]
54. Munro J, Mason S, Nicholl Effectiveness of measures to reduce emergency department waiting times: a natural experiment. Emerg Med J. 2006;23:35–9. [PMC free article] [PubMed]
55. Banerjee A, Mbamalu D, Hinchley G. The impact of process re-engineering on patient throughput in emergency departments in the UK. Int J Emerg Med. 2008;1:189–95. [PMC free article] [PubMed]


