| Author | Affiliation |
|---|---|
| Jag S Heer, MD | Kern Medical Center, Department of Emergency Medicine, Bakersfield, California |
| Denver K Chao, MD | Kern Medical Center, Department of Emergency Medicine, Bakersfield, California |
| Rick A McPheeters, DO | Kern Medical Center, Department of Emergency Medicine, Bakersfield, California |
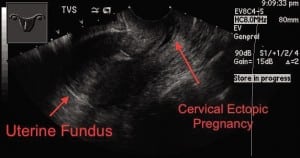
A 31-year-old, who is gravida 2 para 1 at 6 weeks by last menstrual period, presents for vaginal bleeding starting approximately 5 days earlier. The bleeding was initially light, and there was no associated abdominal pain. The bleeding seemed to stop when she laid down and increased upon standing. Past medical, surgical, and social histories were unremarkable. On exam, vital signs were normal. Pelvic exam showed blood at the external orifice of the uterus, no cervical motion tenderness or adenexal tenderness. The remainder of the exam was unremarkable. Quantitative serum human chorionic gonadotropin was 7,470. Transabdominal and transvaginal bedside ultrasounds are shown in Figures 1 and 2, demonstrating an hour-glass deformity of the cervix. Fetal heart tones were present. The findings are consistent with cervical ectopic pregnancy.

DISCUSSION
Cervical pregnancy is a rare, life-threatening form of ectopic pregnancy occurring in approximately 1:9,000 pregnancies. The majority of women with a cervical pregnancy are those of low parity. Thus the current treatment trend is to preserve their reproductive function. The major predisposing factor seems to be dilatation and curettage, but others include previous cesarean delivery and in vitro fertilization. Asherman’s syndrome, prior instrumentation or therapeutic abortion use, infertility, and prior ectopic pregnancies have also been implicated as predisposing factors.1 The hallmark of the presentation is profuse, painless vaginal bleeding. Lower abdominal cramping is conspicuously absent and is found in less than one third of patients. Findings on bimanual exam include a soft, disproportionately large cervix compared to the uterus or an hour-glass shaped uterus. Sonography has led to the correct diagnosis in 81.8% of patients. Emergency physicians should have a high index of suspicion for cervical ectopic pregnancy with a low-lying gestation. Early diagnosis allows early intervention, increasing the likelihood of successful conservative treatment.1,2 Our patient received conservative treatment with methotrexate and intra-amniotic injection of potassium chloride. She did well and was discharged 2 days later.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted April 18, 2011; Revision received May 5, 2011; Accepted May 9, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.5.6774
Address for Correspondence: Jag S. Heer, MD
Kern Medical Center, Department of Emergency Medicine, 1700 Mount Vernon Ave, Bakersfield, CA 93306
E-mail: jheer@bak.rr.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Ushakov FB, Elchalal U, Aceman PJ, et al. Cervical pregnancy: past and future. Obstet Gynecol Surv. 1997;52:45–59. [PubMed]
2. Vela G, Tulandi T. Cervical pregnancy: the importance of early diagnosis and treatment. J Minim Invasive Gynecol. 2007;14:481–484. [PubMed]


