| Author | Affiliation |
|---|---|
| Tara Benesch, MD, MS | Highland General Hospital, Department of Emergency Medicine, Oakland, California |
| Daniel Mantuani, MD | Highland General Hospital, Department of Emergency Medicine, Oakland, California |
| Arun Nagdev, MD | Highland General Hospital, Department of Emergency Medicine, Oakland, California |
Introduction
Case report
Discussion
Conclusion
ABSTRACT
Introduction
The serratus anterior plane block (SAPB) has been shown to effectively treat pain following breast surgery, thoracotomies, and rib fractures. We present the first reported case of a bilateral ultrasound-guided SAPB in a multimodal analgesic regimen after an acute large, thoracic, deep partial-thickness burn.
Case Report
A 72-year-old male presented in severe pain two days after sustaining a deep partial- thickness burn to his anterior chest wall after his shirt caught on fire while cooking. The area of injury was on bilateral chest walls, and the patient was consented for bilateral SAPBs at the level of the third thoracic ribs (T3). With ultrasound guidance, a mixture of ropivacaine and lidocaine with epinephrine was injected into the fascial plane overlying bilateral serratus muscles at T3. The patient reported complete resolution of pain for approximately 15 hours and required minimal additional intravenous analgesia.
Conclusion
The ultrasound-guided SAPB may be an excellent addition to the multimodal analgesic regimen in superficial and partial-thickness burns of the anterior chest wall.
INTRODUCTION
Chest wall burns are relatively common, and often do not require specialized treatment at a burn center.1 In cases of non-circumferential injuries of the chest that do not require surgical intervention, the most common medical management priorities include volume resuscitation and optimal pain management. Mainstays of pain regimens include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, opioids and ketamine, with ultrasound-guided regional anesthesia uncommonly employed in the non-operative setting.2
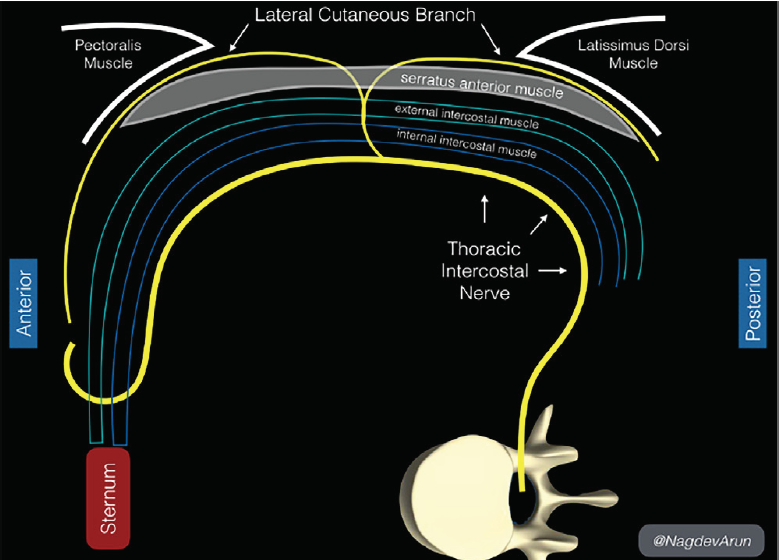
The ultrasound-guided serratus anterior plane block (SAPB), first described by Blanco et al in 2013, is an effective method of achieving analgesia of the hemithorax from the second thoracic (T2) to ninth thoracic (T9) dermatomes.3 Approximately 25–30 milliliters (mL) of anesthetic is injected into the fascial plane either superficial or deep to the serratus anterior (SA) muscle. This targets lateral cutaneous branches of the thoracic intercostal nerves that reside in these fascial planes. SAPBs have been used to reduce pain following breast surgeries, major lung resection, and cardioverter defibrillator insertion.4-7 More recently, the SAPB is being used in the emergency department (ED) to treat severe pain from rib fractures, herpes zoster, and tube thoracostomy placement.8, 9 This technique can be easily and safely performed at the bedside and offers another option in the multimodal strategy for pain control in a variety of thoracic injuries. We present the first case of bilateral ultrasound-guided SAPBs incorporated into a multimodal acute pain regimen in a case of large thoracic partial-thickness burn in the ED.
CASE REPORT
A 72-year-old male with diabetic polyneuropathy presented to the ED with a chief complaint of chest pain two days after sustaining a flame burn while cooking. His vital signs were stable and his physical exam revealed a deep partial-thickness burn over the majority of his right pectoralis extending across midline to the left sternal border (Image 1). The patient reported severe thoracic pain (10/10) unrelieved with oral therapy consisting of NSAIDs and acetaminophen at home.
After obtaining informed consent, bilateral SABPs were performed in the manner described by Blanco et al.3 The anesthetic dose was calculated based on the patient’s weight of 66 kilograms (kg) and recommended maximum dose of 3 milligrams (mg)/kg ropivacaine. This yielded a maximum of 20 milliliters (mL) of 1% ropivacaine (10mg/mL) total for both SABPs, or 10 mL per side. An additional 5 mL of 1% lidocaine with epinephrine was added to each SABP to prolong the effect of the block and reduce the systemic absorption of ropivacaine.10
CPC-EM Capsule
What do we already know about this clinical entity?
Serratus anterior plane blocks (SAPB) effectively treat pain following breast surgery, thoracotomies, and rib fractures.
What makes this presentation of disease reportable?
This is the first description of an ultrasound-guided SAPB performed in the emergency department (ED) for the management of pain from an extensive partial-thickness thoracic burn.
What is the major learning point?
Ultrasound-guided SAPBs can provide safe and rapid analgesia for patients with superficial and partial-thickness chest wall burns in the ED.
How might this improve emergency medicine practice?
Ultrasound-guided SAPBs can facilitate chest wall burn treatments such as dressing changes and wound debridement while reducing reliance on opioid medications.
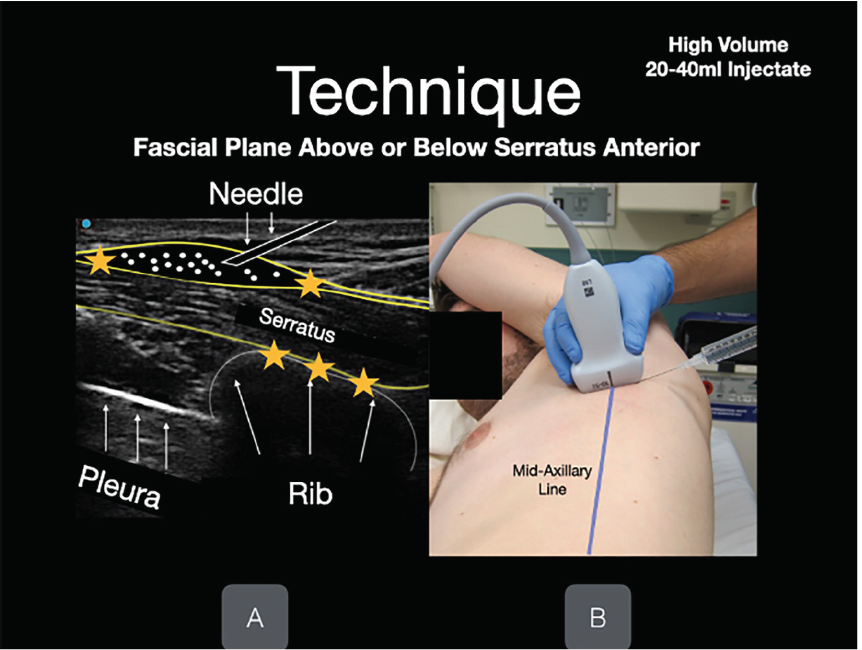
The patient was positioned in the left lateral decubitus position with right arm overhead for the right-sided block. A high-frequency 10-5 megahertz linear transducer was used to locate the third rib in cross section in the mid-axillary line. Superficial to the rib lies the SA, which is deep to the latissimus dorsi (LD) (Figure). The targeted lateral cutaneous branches of the intercostal nerves at thoracic vertebral levels three to nine (T3–T9), are located in the fascial plane separating the SA and LD muscles. Anesthetic spreads in the fascial plane above and below the level of injection to the lateral cutaneous branches of the thoracic intercostal nerves. Although anesthetic will affect dermatomes above and below the site of injection, it is necessary to adjust the injection site based on the dermatome level. We recommend injecting just above the superior level of injury, targeting the level above the dermatome in case of miscounting the ribs. In this patient, whose burns were located in the T2-T5 dermatomes, we injected at the T2 dermatome above the third rib at the mid-axillary line.

After sterilizing and anesthetizing the skin, an in-plane technique was used to inject the 15-mL mixture of ropivacaine and lidocaine with epinephrine between SA and LD muscles (Image 2) following hydrodissection with 10 mL of normal saline. The same process was repeated on the patient’s left side. The injected ropivacaine and lidocaine spreads along the fascial plane above and below the site of injection, a process facilitated by hydrodissection with 10mL of normal saline before and after anesthetic administration. Thus, it is not necessary repeat injections at each thoracic vertebral level to achieve analgesia across the chest wall.
Five minutes after the initial injection, the patient reported significant analgesia over his right chest, and 20 minutes after the termination of the procedure he was able to sleep comfortably. The patient reported no discomfort during the injection process and experienced no side effects. A local burn center recommended admission for treatment with silver sulfadiazine and fluid resuscitation; when the patient was interviewed on hospital day two, he reported the SABP took approximately 20–30 minutes to take full effect and lasted for an estimated 15–18 hours. He ultimately required two doses of 2 mg intravenous morphine at approximately 30 hours and 35 hours after his SABP. His only other medications were acetaminophen 500 mg orally every six hours, ibuprofen 600 mg orally every six hours, and home medications gabapentin and trazodone. The patient was discharged in stable condition on hospital day two.
DISCUSSION
The SAPB, originally used to control pain following breast surgery, is now becoming increasingly popular among emergency physicians to control pain from thoracic injuries in the ED.3,8 Although the majority of cases in the literature describe the use of the SAPB to relieve pain from rib fractures, other authors have demonstrated its utility in reducing pain from herpes zoster and tube thoracostomy placement.8,9 To our knowledge, this is the first description of an ultrasound-guided SAPB used for the management of pain from an extensive partial-thickness thorax burn in the ED.
Burns are a leading cause of accidental injury, many of which will not require management at a burn center. Aggressive pain control is necessary in the treatment of these injuries. A multimodal regimen including opioids and ketamine is often required to achieve adequate analgesia for large burns. However, opioids carry risks and side effects of respiratory depression, nausea/vomiting, constipation, and addiction; and ketamine may cause dizziness, dysphoria, and altered mental status.11,12 As demonstrated by this case, we believe regional anesthesia is a valuable tool in a multimodal pain control regiment for burn patients in the ED. Peripheral nerve blocks have been effectively used for analgesia in patients undergoing wound debridement and dressing changes at burn centers.13 A single-injection SAPB can provide approximately 12 hours or more of pain relief to the anterolateral hemithorax without affecting motor function, and may be an ideal option for pain relief prior to dressing changes, wound debridement, or rehabilitation exercises in patients with chest wall burns.
With regard to anesthetic choice, ropivacaine was selected for its long duration of anesthesia and good safety profile. When compared to lidocaine, ropivacaine has a slightly longer mean onset time but provides a much longer mean duration of anesthesia (21.5 hours for ropivacaine compared to 2.4 hours for lidocaine in digital blocks).14 Although bupivacaine has a similar mean duration of anesthesia as ropivacaine, ropivacaine has fewer motor effects and a better safety profile (including being safe to use in pregnancy).15-17
We recognize that the ultrasound-guided SAPB may not be ideal for burns posterior to the mid-axillary line. We have noted minimal success of this planar block in patients with posterior rib fractures and are unclear of the efficacy of this block for these injuries. We also recognize that clinicians performing high-volume SAPB blocks should be aware of maximal anesthetic dosing to prevent administering a toxic dose. The patient’s weight should be measured and a dosing calculator should be used to ensure safety.
CONCLUSION
Ultrasound-guided serratus anterior plane blocks can potentially provide a safe and rapid method of analgesia for patients with superficial and partial-thickness chest wall burns in the ED. They may be easily performed at the bedside with minimal risk of affecting respiration, mental status, or motor function. As such, they may be a valuable addition to a multimodal pain regimen used in the evaluation and treatment of chest wall burns, and may facilitate treatments such as dressing changes and wound debridement while reducing reliance on opioid medications.
Footnotes
Section Editor: R. Gentry Wilkerson, MD
Full text available through open access at http://escholarship.org/uc/uciem_cpcem
The authors attest that their institution requires neither Institutional Review Board approval, nor patient consent for publication of this case report. Documentation on file.
Address for Correspondence: Tara Benesch, MD, MS, Highland General Hospital, Department of Emergency Medicine, 1411 East 31st Street, Oakland, CA 94602. Email: tbenesch@alamedahealthsystem.org. 5:117 – 120
Submission history: Revision received October 8, 2020; Submitted December 21, 2020; Accepted December 18, 2020
Conflicts of Interest: By the CPC-EM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Gibran NS. Burns of the chest wall. Thoracic Trauma and Critical Care. 2002.
2. Griggs C, Goverman J, Bittner EA, et al. Sedation and pain management in burn patients. Clin Plast Surg. 2017;44(3):535-40.
3. Blanco R, Parras T, Mcdonnell JG, et al. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107-13.
4. Hetta DF, Rezk KM. Pectoralis-serratus interfascial plane block vs thoracic paravertebral block for unilateral radical mastectomy with axillary evacuation. J Clin Anesth. 2016;34:91-7.
5. Ahiskalioglu A, Yayik AM, Demir U, et al. Preemptive analgesic efficacy of the ultrasound-guided bilateral superficial serratus plane block on postoperative pain in breast reduction surgery: a prospective randomized controlled study. Aesthetic Plast Surg. 2020;44(1):37-44.
6. Ziacchi M, Bisignani G, Palmisano P, et al. Serratus anterior plane block in subcutaneous implantable cardioverter defibrillator implantation: a case-control analysis. J Cardiovasc Electrophysiol. 2020;31(1):144-9.
7. Viti A, Bertoglio P, Zamperini M, et al. Serratus plane block for video-assisted thoracoscopic surgery major lung resection: a randomized controlled trial. Interact Cardiovasc Thorac Surg. 2020;30(3):366-72.
8. Lin J, Hoffman T, Badashova K, et al. Serratus anterior plane block in the emergency department: a case series. Clin Pract Cases Emerg Med. 2020;4(1):21-5.
9. Durant E, Dixon B, Luftig J, et al. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2017;35(1):197.e3-6.
10. Karmakar MK, Ho AM, Law BK, et al. Arterial and venous pharmacokinetics of ropivacaine with and without epinephrine after thoracic paravertebral block. Anesthesiology. 2005;103(4):704-11.
11. Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105-20.
12. Rosenbaum SB, Gupta V, Palacios JL. Ketamine. 2020. Available at: https://www.ncbi.nlm.nih.gov/books/NBK470357. Accessed October 11, 2020.
13. Kovac AL, Mehta N, Salerno S, et al. Peripheral nerve blocks for analgesia in burn unit patients: a retrospective study. J Burn Care Res. 2018;39(1):S195-6.
14. Keramidas EG, Rodopoulou SG. Ropivacaine versus lidocaine in digital nerve blocks: a prospective study. Plast Reconstr Surg. 2007;119(7):2148-52.
15. Arthur GR, Feldman HS, Covino BG. Comparative pharmacokinetics of bupivacaine and ropivacaine, a new amide local anesthetic. Anesth Analg. 1988;67(11):1053-8.
16. Scott DB, Lee A, Fagan D, et al. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg. 1989;69(5):563-9.
17. McGlade DP, Kalpokas MV, Mooney PH, et al. A comparison of 0.5% ropivacaine and 0.5% bupivacaine for axillary brachial plexus anaesthesia. Anaesth Intens Care. 1998;26(5):515-20.


