| Author | Affiliation |
|---|---|
| Marcela Garrido, MD | P. Universidad Católica de Chile, Emergency Medicine Program, Santiago, Chile |
| Pablo Aguilera, MD | P. Universidad Católica de Chile, Emergency Medicine Program, Santiago, Chile |
A 15-year-old boy presented to the emergency department with a chief complaint of bilateral pleuritic chest pain and shortness of breath. His symptoms began suddenly, hours earlier, while studying in school without any history of trauma. The patient did not smoke, denied illicit drug use, had no known toxic exposures, but did report cough and upper respiratory symptoms for the previous 2 days. Otherwise, he had no significant past medical or surgical history. The patient was alert, appropriately responsive, and in moderate respiratory distress. He was afebrile with a heart rate of 105 beats per minute, blood pressure of 135/90 mmHg, respiratory rate of 30 breaths per minutes and peripheral oxygen saturation was 97% on room air. The patient was noted to have decreased breath sounds bilaterally. Supplemental oxygen via a nasal cannula was started, and an emergent chest radiograph was obtained (Figure 1).
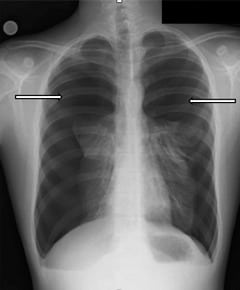
A diagnosis of bilateral spontaneous pneumothorax was made and given the possibility of progression to tension; needle decompression was performed anteriorly to both sides of the chest. Although a less invasive Heimlich valve placement was favored, lack of stock within the department limited this option. As a result, emergent chest thoracostomy tubes were placed (Figure 2).

The patient had complete re-expansion of the left lung, and partial re-expansion on the right. No clinically significant signs of postprocedural pulmonary edema were noted. Subsequent computed tomography of the chest revealed apical subpleural blebs, and the patient underwent thoracoscopic surgical resection followed by bilateral pleurodesis.
Bilateral spontaneous pneumothorax is an extremely rare clinical condition representing approximately only 1% of all cases of spontaneous pneumothorax.1–2 Even rarer is to see a patient with near complete spontaneous bilateral pneumothorax without cardiovascular collapse. Perhaps this suggests that the patient had asymptomatic or compensated unilateral symptoms followed by acute decompensation following onset of bilateral spontaneuous pneumothorax.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted October 8, 2011; Accepted October 10, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.10.6910
Address for Correspondence: Marcela Garrido, MD
P. Universidad Cato´ lica de Chile, Emergency Medicine Program, 63 Lira, Santiago, Chile 8330074
E-mail: migarrid@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Wang H, Nugent WC. Cough-induced bilateral spontaneous pneumothorax. Ann Thorac Surg.2010;90:1363–1365. [PubMed]
2. Lee SC, Cheng YL, Huang CW, et al. Simultaneous bilateral primary spontaneous pneumothorax.Respirology. 2008;13:145–148. [PubMed]


