| Author | Affiliation |
|---|---|
| Megan M. Mroczkowski, MD | Columbia University Irving Medical Center, Department of Psychiatry, New York, New York |
| John T. Walkup, MD | Ann & Robert H. Lurie Children’s Hospital of Northwestern University, Department of Psychiatry and Behavioral Sciences, Chicago, Illinois |
| Paul S. Appelbaum, MD | Columbia University Irving Medical Center, Department of Psychiatry, New York, New York |
Background
Methods
Results
Discussion
ABSTRACT
Introduction
Violence risk assessment is one of the most frequent reasons for child and adolescent psychiatry consultation with adolescents in the pediatric emergency department (ED). Here we provide a systematic review of risk factors for violence in adolescents using the risk factor categories from the MacArthur Violence Risk Assessment study. Further, we provide clinical guidance for assessing adolescent violence risk in the pediatric ED.
Methods
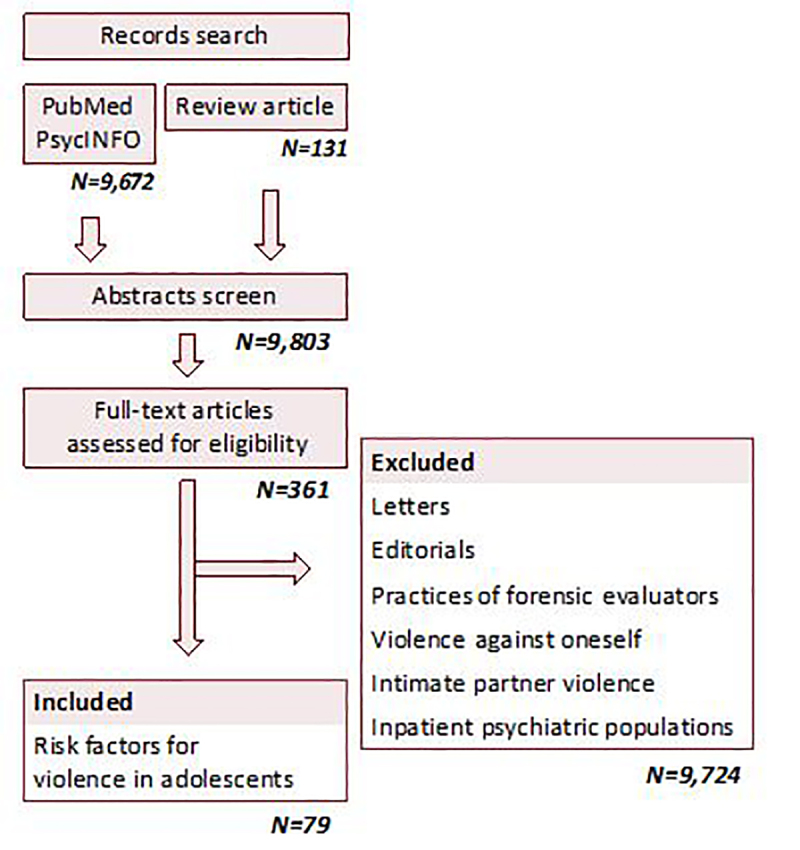
For this systematic review, we used the preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2009 checklist. We searched PubMed and PsycINFO databases (1966–July 1, 2020) for studies that reported risk factors for violence in adolescents.
Results
Risk factors for adolescent violence can be organized by MacArthur risk factor categories. Personal characteristics include male gender, younger age, no religious affiliation, lower IQ, and Black, Hispanic, or multiracial race. Historical characteristics include a younger age at first offense, higher number of previous criminal offenses, criminal history in one parent, physical abuse, experiencing poor child-rearing, and low parental education level. Among contextual characteristics, high peer delinquency or violent peer-group membership, low grade point average and poor academic performance, low connectedness to school, truancy, and school failure, along with victimization, are risk factors. Also, firearm access is a risk factor for violence in children and adolescents. Clinical characteristics include substance use, depressive mood, attention deficit hyperactivity disorder, antisocial traits, callous/unemotional traits, grandiosity, and justification of violence.
Conclusion
Using MacArthur risk factor categories as organizing principles, this systematic review recommends the Structured Assessment of Violence Risk in Youth (SAVRY) risk- assessment tool for assessing adolescent violence risk in the pediatric ED.
BACKGROUND
Violence or aggression among adolescents is a common problem of enormous public health significance. Physical fighting is the most common form of violence in adolescents.1 In addition to the increased risk for injury and substance abuse, those who fight report less satisfaction with life, poorer relations with family and peers, and a worse perception of school. Within the past 12 months, 32.8% of high school-aged youth have been in a fight and 16.6% carried weapons to school.2 Since the 1980s, youths aged 10–17 years constituted less than 12% of the US population but have been offenders in 25% of serious violent victimizations.3
The evolution of violence can be conceptualized to begin in young childhood. Children first learn to manage aggression from their parents as toddlers; poor parenting, such as abuse, neglect, coercive parenting styles, antisocial modeling, and poor limit setting, may lead to an increased risk for violence.4 About 30% of those with oppositional defiant disorder go on to develop conduct disorder.5 Of those with conduct disorder, about 40% will progress to antisocial personality disorder.6
There are two main patterns of development of violence: early onset and late onset.7 Early-onset violence begins before puberty, accounts for 30% (+/− 15%) of serious violent offenders,—13% of whom go on to violent careers longer than two years—and is strongly associated with general offenses and substance use.7 In contrast, late-onset violence begins after puberty and accounts for 70% (+/− 15%) of serious violent offenders, 2% of whom go on to violent careers longer than two years.7 Late-onset violence is associated with weak social ties, antisocial and delinquent peers, and gang membership. 7
There are key differences between violent behavior in adolescents and adults.7 These differences can be categorized into epidemiology, diagnoses, behavior patterns, treatment, and legal status. In adolescents, compared to adults, violence is much more common and accounts for a higher proportion of all deaths, and violent careers are shorter; the first episode of serious violence most often occurs in adolescence, sometimes childhood, and rarely in adulthood.7 Psychotic disorder is much less common in adolescents who are violent than in adults. Adolescent violent behaviors tend to occur more in groups than adult violent behavior.7
Programs at all levels of schooling are effective in preventing violence. In addition to reducing aggressive and violent behaviors, these programs also improve school achievement and activity levels, and reduce truancy.8 In middle school, programs focus on disruptive behaviors, bullying, and general violence, while high school programs focus on violence, dating violence, and bullying. The programs that decreased violence most drastically were those taught by peers.8 Treatment for adolescents who are violent should consider both peer and family involvement.7 Adolescent legal status allows for legal consent for treatment to be provided by a legal guardian and, with some variation by age across states, hospitalization can occur over the patient’s objection with a legal guardian’s consent.7
Aggression and violence are one of the most frequent reasons for child psychiatry consultation on adolescents in the emergency department (ED).9 Assessment of violence risk may be required to determine appropriate disposition and avoid liability for untoward outcomes. Therefore, predicting who may become violent is of utmost importance. Unfortunately, predicting violence can be difficult; studies have shown that psychiatrist and nurse predictions of violence in both inpatient and community samples are poor, at times not differing from chance. 10
Assessing violence risk falls into the purview of pediatricians and child and adolescent mental health professionals. Following work in adult, actuarial risk-assessment scales, there has been progress in applying scales to adolescents.11 The two scales that have the strongest psychometric support are the Structured Assessment of Violence Risk in Youth (SAVRY) and the Psychopathy Checklist-Youth Version (PCL-YV). 12,13 However, neither these nor other scales are routinely used in clinical practice.
To equip both ED pediatricians and child and adolescent mental health professionals with the best knowledge to confront the assessment and treatment of aggression, we report a systematic review of the literature on risk factors for violence in adolescents in the community and characterize what is currently known using the risk factor categories from the MacArthur Violence Risk Assessment study as organizing principles; identify gaps in knowledge; and discuss recommendations for further research.14 We conclude with recommendations for assessing adolescent violence risk in the pediatric ED.
METHODS
Protocol and Registration
For this systematic review, we used the preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2009 checklist. Full details of this review are listed below.
Eligibility criteria and Data Sources
We searched PubMed and PsycINFO databases (1966–July 1,2020) for studies that reported risk factors for violence in adolescents. We also searched reference lists from identified reports for additional sources. We considered only articles published in English.
Search
To create a comprehensive list of studies examining risk factors for adolescent violence, we used combinations of the following search terms (Figure).
PubMed database
risk factors AND violence AND juveniles (#66); risk factors AND violence AND juveniles AND review (#13); predictors AND violence AND juveniles (#8); predictors AND aggression AND juveniles (#5); predictors AND violence AND adolescents (#1107); risk factors AND violence AND adolescents (#7270).
PsycINFO database
risk factors AND violence AND juveniles (#63), risk factors AND violence AND juveniles AND review (#13), predictors AND violence AND juveniles (#17), predictors AND aggression AND juveniles (#10), predictors AND violence AND adolescents (#297); risk factors AND violence AND adolescents (#803).
Study Selection
We included a study in our dataset if it examined or included risk factors for violence in adolescents. We defined adolescent as an individual between the ages of 11–18. Violence was defined as fighting, using a weapon in a fight, hitting or beating up someone, hurting someone badly enough to need bandages or a doctor, or using a weapon to obtain something. Violence did not include violence against oneself.
We excluded a study from the dataset if it had any of the following characteristics: 1) only included violence among inpatient populations; 2) focused solely on intimate partner violence; 3) was a review, letter or editorial; 4) had been withdrawn; or 5) only described clinical violence assessment practices of forensic evaluators. The lead investigator (MM) searched and vetted each prospective paper, sharing the descriptive information with co-authors (JW and PA) for their review and comments. The lead investigator, taking these comments, had the final say on study inclusion.
Data Collection Process
We extracted data and recorded information on the details of where and how the study was conducted, sample characteristics, size of study, and how risk factors were measured.
Data Items
We categorized the correlates of violence identified in the studies using the typology of the MacArthur risk assessment study: Personal, Historical, Contextual and Clinical characteristics.14 A risk factor was considered positive if there was a statistically significant (P<0.05) association with violence as an outcome. The number of total subjects in each row (N) in Tables 1–4 indicates the number of subjects in studies in which the results for that variable were significant.
Table 4Clinical risk factors.
| Risk factor | N (total) | References |
|---|---|---|
| Substance use | ||
| Alcohol use | 75,287 | 20,22,24,35,37,42, 47,49,63,66,81,82 |
| Illicit drug use | 121,891 | 56,63,69,83–85,19, 21,22,24,65,71,84, 86 |
| Cigarette smoking | 11,694 | 20,37,86 |
| Depression | ||
| Depression symptoms | 4,491 | 30,35,37,68 |
| Suicide attempt | 16,410 | 49 |
| PTSD | 3 | 90 |
| ADHD | 10,209 | 16,27,32,36,60,64, 66 |
| Psychosis-like experiences | 18,104 | 24 |
| Impulse control | ||
| Lack of self-control | 1,100 | 15,87 |
| Risk-taking behaviors | 9,770 | 27,45,57,75 |
| Previous unintentional injury | 337 | 37 |
| Temperament and personality traits | ||
| Antisocial traits or favorable attitude toward antisocial behavior | 7,989 | 19,51,56,57,68,71 |
| Grandiosity | 974 | 89 |
| Justification of violence | 974 | 89 |
| Anger | 5,312 | 20,69 |
| Callous/unemotional traits | 3,019 | 36,56,69 |
| Perceived invulnerability to future events | 2,335 | 35 |
| Belief that hurting another’s property while intoxicated is acceptable | 1,332 | 84 |
| Cluster A and B personality traits | 717 | 88 |
| Emotional distress | 1,719 | 87 |
| Poor emotion regulation | 310 | 52 |
| Higher levels of aggressive beliefs | 1,719 | 87 |
| Less likely to suppress anger | 282 | 62 |
PTSD, post-traumatic stress disorder; ADHD, attention deficit hyperactivity disorder.
Table 3Contextual risk factors.
| Risk factor | N (total) | References |
|---|---|---|
| School | ||
| Low connectedness/support at school | 23,886 | 32,60,62 |
| Low GPA | 18,613 | 27,46,50,60,63, 64 |
| Truancy | 14,627 | 30,47 |
| Low school motivation | 1,517 | 30 |
| Suspensions | 12,703 | 55,63 |
| Feel unsafe to go to school | 46,756 | 49,65 |
| Poor study skills | 4,432 | 66 |
| School failure/repeat grade | 27,302 | 27,47,67 |
| Wanting to quit school | 3,955 | 51 |
| Felt school discipline unfair | 282 | 62 |
| Social relations | ||
| High peer delinquency | 29,902 | 30,31,55,57,68–70,18,19,31,64, 66,71,72 |
| Friends who use drugs | 3,174 | 31,71 |
| Bullying others | 20,054 | 36,73,74 |
| Victim of bullying or violence | 21,789 | 24,71,75 |
| Gang affiliation | 1,642 | 46 |
| Sexually active | 2,299 | 22 |
| Fewer friends committed to learning | 2,055 | 31 |
| Dating violence | 1,080 | 31 |
| Belonging to a sports team | 1,642 | 46 |
| Low peer support/peer rejection | 28,898 | 61,70,72 |
| Practicing unsafe sex (males only) | 7,548 | 45 |
| Peer pressure | 4,056 | 70 |
| Access to firearms | 12,734 | 59,76 |
| Relationship with parents | ||
| Family strain | 848 | 75 |
| Parental psychological aggression | 302 | 68 |
| High parental stress | 1,517 | 30 |
| Parental non-authoritative behavior | 2,335 | 35 |
| Poor relationship with parents | 9,603 | 31,45 |
| Parent-child conflict | 12,417 | 32,55,70,72 |
| Less family involvement | 1,080 | 31 |
| Less parental control | 1,080 | 31 |
| Living in single-parent household | 10,261 | 36,45 |
| Rejecting parenting | 310 | 52 |
| Socioeconomic status | ||
| Low socioeconomic status | 49,113 | 27,30,61,77 |
| Exposure to community violence | 3,176 | 17,18,31,76,78–80 |
| Drug use in neighborhood | 4,626 | 55,64 |
| Community disorganization | 3,818 | 55 |
| 5+ siblings | 511 | 27 |
| Neighborhoods where young people were in trouble | 808 | 32 |
GPA, grade point average.
Table 1Personal risk factors found to be correlates for violence in adolescents.
| Risk factor | N (total) | References |
|---|---|---|
| Gender | ||
| Male gender | 33,902 | 15,16–19,20–24 |
| Religion | ||
| No religious affiliation | 3,872 | 20 |
| Race | ||
| Black | 3,107 | 16,22 |
| Hispanic | 84,734 | 25 |
| Multiracial | 2,305 | 28 |
| IQ | ||
| Lower IQ | 588 | 26,27 |
| Age | ||
| Younger age | 2,385 | 19 |
IQ, intelligence quotient.
Table 2Historical risk factors.
| Risk factor | N (total) | References |
|---|---|---|
| Criminal history | ||
| Younger age at first offense | 11,008 | 15,29–33 |
| Prior violence | 24,784 | 55–57,21,47,58 |
| Drug selling | 4,586 | 21 |
| Arrests | 3,818 | 55 |
| Disruptive behavior | ||
| Cruel to people | 1,517 | 30 |
| Childhood aggressiveness (boys) | 415 | 54 |
| Children characterized as under-controlled at age 6 | 731 | 53 |
| Childhood fighting | 808 | 16 |
| Early antisocial influences | 808 | 16 |
| Conduct problems | 11,580 | 27,36,50–52 |
| Carrying weapon | 29,520 | 47,49 |
| Animal cruelty | 542 | 23 |
| Parental criminal history | ||
| Parental or familial criminality | 8,012 | 29,27 |
| Physical abuse | ||
| Physical abuse | 172,957 | 38,40–48 |
| Sexual abuse | 140,021 | 38,39 |
| Neglect | 1,037 | 39 |
| Witnessing abuse | 136,549 | 38 |
| Family history | ||
| Poor child-rearing of parent | 411 | 27 |
| Low parental education level | 5,385 | 35–37 |
| Parental job loss | 4,586 | 21 |
| Higher maternal antisocial personality disorder score | 2,562 | 19,26 |
| Maternal bipolar disorder and perpetrating intraparental violence | 120 | 34 |
| Family alcohol or drug use | 139,386 | 38,71 |
| Low parental support | 29,565 | 20,21,61 |
| Parent convicted of crime | 411 | 27 |
Risk of Bias in Individual Studies and Across Studies
We considered potential biases at the study level, broadly defined, focusing on flawed study design. Given that in this systematic review we considered studies with multiple outcome measures that differed across studies, standard metrics of bias in the literature (eg, publication bias) were inapplicable.
RESULTS
Study Characteristics
All but two of the studies in this review were surveys or longitudinal observational studies. There were no randomized controlled trials addressing violence risk in adolescents.
Risk of Bias Within Studies
Many of the studies suffered from flaws in study design. Taken as a whole, the studies considered a constricted range of risk factors, weak criterion measures of violence, narrow study samples, and data gathered at a single site. These flaws are elaborated on in the Discussion section.
Results of Individual Studies
Personal characteristics (Table 1) found to be correlates for violence in adolescents included male gender, race (Black, Hispanic, or multiracial), religion (no religious affiliation), IQ (lower IQ), and age (younger age). 15-28
Historical characteristics (Table 2) can be further organized within the following subcategories: criminal history, disruptive behavior, parental criminal history, physical abuse, and family history. Within the subcategory of criminal history, a younger age at first offense, higher number of previous criminal offenses, prior violence, and drug selling were found to be correlates for violence in children and adolescents. Disruptive behavior can be characterized by aggressiveness or fighting in childhood, cruelty to people, early antisocial influences or behaviors, conduct problems, under-controlled behavior at age six, carrying a weapon, and animal cruelty. Parental criminal history involves criminal history in either parent. Physical abuse is described as maltreatment starting in childhood or adolescence. Family history risk factors include the child’s parents experiencing poor child-rearing when they were children, low parental education level, and higher maternal antisocial personality disorder score, maternal bipolar disorder, interparental violence, family alcohol or drug use, and low parental support.15,16,19,21,23,26,27,29-58
Contextual characteristics (Table 3) found to be correlates for violence in adolescents include the categories of school, social relations, firearm access, relationship with parents, and socioeconomic status. Within the category of school, low connectedness or support at school, low grade point average, truancy, low school motivation, suspensions, feeling unsafe at school, poor study skills, school failure or repeating a grade, wanting to quit school, or feeling school discipline is unfair are all risk factors. Social relations that were risk factors included high peer delinquency, friends who use drugs, bullying others, victim of bullying, gang affiliation, sexually active, unsafe sex (in males), fewer friends committed to learning, dating violence, belonging to a sports team, peer pressure, and low peer support. Firearm access is a risk factor for violence in children and adolescents.59 Risk factors within the category relationship with parents include family strain, high parental stress, parental psychological aggression, parental non-authoritative behavior, poor relationship with parents, parent-child conflict, less parental control, rejecting parenting, and living in a single-parent household. Socioeconomic status risk factors include low socioeconomic status, exposure to community violence, drug use in the community, community disorganization, having five or more siblings, and living in a neighborhood where young people are in trouble.17-19,22,24,27,30-32,35-37,45-47,49-52,55,57,59-80
Clinical characteristics (Table 4) associated with correlates for violence in adolescents were organized into the following categories: substance use; depressive symptoms; attention deficit hyperactivity disorder (ADHD); impulse control; temperament and personality trait; and psychopathy. Cigarette, alcohol, and other illicit substances were found to be risk factors and can be classified under substance use. Symptoms related to depression, including suicide attempts, are risk factors for violence, as are ADHD, post-traumatic stress disorder, and psychotic-like experiences. Impulse control deficits, including lack of self-control, risk-taking behaviors, and previous unintentional injury, were also associated with violence risk. Temperament and personality traits that were risk factors include antisocial traits, callous/unemotional traits, grandiosity, justification of violence, intrapersonal strain, anger, perceived invulnerability to future events and the belief that damaging another’s property while intoxicated was acceptable, Cluster A and B personality traits, emotional distress, higher levels of aggressive beliefs, poor emotion regulation, and reduced likelihood of suppressing anger were also risk factors for violence.15,16,19-22,24,27,30,32,35-37,42,45,47,49,51,52,56,57,60,62-66,68,69,71,75,81-90
DISCUSSION
Summary of Evidence
From the studies included in our dataset, several risk factors were found in multiple studies and stand out clearly. Personal risk factors include male gender and race (Black, Hispanic or multi-racial), along with lower IQ and younger age. Historical risk factors include childhood aggressiveness in boys, childhood fighting, early antisocial influences, hyperactivity and withdrawal in childhood, child maltreatment, and higher maternal antisocial personality disorder score. Younger age at first offense and prior violence were described in a multitude of studies. These risk factors fit with the adage that “the best predictor of future behavior is past behavior,” in that those children who were aggressive or in fights were at risk for future violent behavior. Moreover, early influences are also apparent within this category; specifically, maltreatment as a child or early antisocial influences, especially by the mother, were risk factors. Children learn from the actions of their early caretakers, even if these are antisocial in nature. Additionally, children and adolescents who were themselves maltreated are at risk for perpetrating violence on others.
Limitations of the Literature
The flaws identified in this body of research can be organized and addressed using the critique of violence research on persons with mental illness offered by Monahan and Steadman.10 They identified four problems: constricted range of risk factors; weak criterion measures of violence; narrow study sample; and data gathered at a single site.
Restricted range of risk factors
The first problem is that different studies focus on different risk factors, with no study looking comprehensively at the full range of risk factors. While studies may have included several risk factors, unless they are all measured simultaneously, it is unclear how they interact or whether one fully accounts for the variance that would otherwise be associated with the other. This limits the utility of the data for clinicians, who may be uncertain how much weight to give one or another variable in assessing violence risk.
Risk factors in studies of adolescents have focused on past history and symptom rating scales, such as the Brief Psychiatric Rating Scale. These variables are too narrow and may miss many key risk factors. For instance, risk factors should be studied in multiple domains, including historical and contextual, along with those within a single domain that may be theoretically related, such as impulsivity and anger management. In this review, studies did look at childhood traits such as hyperactivity, conduct problems, and aggressiveness, which may be a good start. Further, various symptoms have been studied, including depressive symptoms and substance abuse. However, it would be more meaningful to document changes in symptoms over time and explore how specific symptom clusters within a broader diagnosis may affect risk. Situational risk factors have been addressed, such as poor academics, truancy, peer delinquency, access to firearms, parental stress and low socioeconomic status, but not consistently across studies.
Weak criterion for violence
The second problem is weak criterion measures for violence. Typically, violence was defined in an undifferentiated manner, ie, all violent outcomes were treated the same. It may be helpful for researchers to define subtypes of violence, as predictors for one type of violence (eg, impulsive violence) may vary from another type (eg, gang violence). However, studies in our review rarely divided violent outcome by subtypes.
Narrow study samples
The third problem identified was narrow study samples. A majority of the studies in this review focused on populations of juvenile delinquents, schools in high-crime areas with low socioeconomic status, mental health clinics, and so-called at-risk youth. Broader samples of subjects should be sought. For example, studies should include both genders, those with and without a history of violence, and multiple socioeconomic statuses. Crucial for further research is the need to widen the inclusion criteria such that risk factors can be understood more universally.
Data gathered from single site
The fourth problem found was data gathered at a single site. When only one site is used, idiosyncratic aspects of the sample available, treatments used, and approaches to rating study variables can limit the generalizability of the data. Studies with larger samples and, therefore, more stable findings usually require research efforts to be coordinated across multiple sites. A few of the studies in this review were national in scope, in the United States and Finland, but the majority were limited to one or a small number of sites. As the research currently stands, groups have created their own lists of predictors and variables, which has led to disjointed findings in the literature. Ideally, groups of researchers should combine efforts in a multidisciplinary and multisite fashion to create common predictors and variables to study risk factors in large number of adolescents.
Limitations of the Review
We did not rate the potential bias in individual studies. There were no randomized controlled trials identified in this search. A majority of the studies were surveys or longitudinal observational studies and, therefore, we did not include the study grade in our tables. Furthermore, we included only English-language papers, searching PubMed and PsycINFO, which may have led to the exclusion of some studies.
Implications for Clinical Risk Assessment
Clinically, organizing risk factors by MacArthur risk factor categories may be useful as a means to carry out a risk assessment with an adolescent presenting to the ED with violence risk. Risk assessment may include interviews with the subject, caretaker, family member, and teacher, along with reviewing mental health, school and police records.91 Given the large number of variables that have been associated with violence and likelihood of significant overlap in the variance for which they account, risk assessment tools may be useful, as may tests of psychopathology, intelligence, and psychopathy. In a study of forensic evaluators, the most used of such tests were the Wechsler Intelligence Scales (75%), the Minnesota Multiphasic Personality Inventory (66.2%), and the SAVRY risk-assessment tool (35.1%). 91 Additionally, one third of clinicians surveyed always or almost always used the Psychopathy Checklist: Youth Version (PCL:YV).91 Each of these tests provides further information for risk assessment and includes a portion of the factors identified in this review.
The SAVRY is the violence risk-assessment instrument for adolescents most commonly used by forensic evaluators.91 Its rating form is organized into historical risk factors, social/contextual risk factors, individual/clinical risk factors, and protective factors.12 Historical risk factors include history of violence; early initiation of violence and exposure to violence at home; childhood history of maltreatment; parental/caregiver criminality; and poor school achievement. Social/contextual risk factors include peer delinquency; peer rejection; stress and poor coping; and poor parental management, among others. Individual/clinical risk factors include risk taking/impulsivity; substance use difficulties; anger management problems; attention deficit/hyperactivity difficulties; and low interest/commitment to school, among others. Protective factors include prosocial involvement; strong social support; strong commitment to school; and positive attitude toward intervention and authority.12
Conclusions and Recommendations for Assessing Violence Risk in the Pediatric Emergency Department
Violence in adolescents is a problem with large public health significance. Its risk factors can be organized using the MacArthur risk assessment study categories. The Structured Assessment of Violence Risk in Youth is the most commonly used violence risk-assessment instrument for adolescents by forensic evaluators.91 Given this systematic review, we recommend its use in the pediatric ED to assess adolescent violence risk. Its rating form is organized into historical risk factors, social/contextual risk factors, individual/clinical risk factors, and protective factors.10 Overall, the SAVRY provides a comprehensive means of assessing risk factors as the literature now stands, and likely is best used in combination with clinical interviews and other testing.
Footnotes
Section Editor: Muhammad Waseem, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Megan M. Mroczkowski, MD, Morgan Stanley Children’s Hospital of NewYork-Presbyterian, Columbia University Irving Medical Center, Department of Psychiatry, 3959 Broadway CHN 619C, New York, NY 10032. Email: mmm2323@cumc.columbia.edu. 5 / 2021; 22:533 – 542
Submission history: Revision received July 24, 2020; Submitted January 10, 2021; Accepted January 24, 2021
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
REFERENCES
1. Pickett W, Molcho M, Elgar FJC, et al. Trends and socioeconomic correlates of adolescent physical fighting in 30 countries. Pediatrics. 2013;131(1):e18-26.
2. Youth Violence: Facts at a Glance. 2010. Available at: www.cdc.gov/violenceprevention. Accessed January 3, 2021.
3. Hahn R, Fuqua-Whitley D, Wethington H, et al. The effectiveness of universal school-based programs for the prevention of violent and aggressive behavior: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recomm Rep. 2007;56(RR-7):1-12.
4. Tremblay RE, Nagin DS, Séguin JR, et al. Physical aggression during early childhood: trajectories and predictors. Pediatrics. 2004;114(1):e43-50.
5. Loeber R, Burke JD, Lahey BB, et al. Oppositional defiant and conduct disorder: a review of the past 10 years, Part I. J Am Acad Child Adolesc Psychiatry. 2000;39(12):1468-84.
6. Zoccolillo M, Pickles A, Quinton D, et al. The outcome of childhood conduct disorder: implications for defining adult personality disorder and conduct disorder. Psychol Med. 1992;22(4):971-86.
7. Ash P. Children are different: liability issues in working with suicidal and dangerous youths. Focus (Am Psychiatr Publ). 2019;17(4):355-9.
8. Hahn R, Fuqua-Whitley D, Wethington H, et al. Effectiveness of universal school-based programs to prevent violent and aggressive behavior: a systematic review. Am J Prev Med. 2007;33(2 Suppl):S114-29.
9. Edelsohn GA, Braitman LE, Rabinovich H, et al. Predictors of urgency in a pediatric psychiatric emergency service. J Am Acad Child Adolesc Psychiatry. 2003;42(10):1197-202.
10. Monahan J, Steadman HJ. Violence and Mental Disorder Developments in Risk Assessment. 1994. Available at: https://press.uchicago.edu/ucp/books/book/chicago/V/bo3684057.html. Accessed January 2, 2021.
11. Vincent GM. Psychopathy and violence risk assessment in youth. Child Adolesc Psychiatr Clin N Am. 2006;15(2):407-28.
12. Borum R, Bartel PA, Forth AE. Structured assessment of violence risk in youth. Mental Health Screening and Assessment in Juvenile Justice. 2005:311-323.
13. Forth A, Kosson D, Hare R. Hare Psychopathy Checklist: Youth Version. Mental Health Screening and Assessment in Juvenile Justice. :324-335.
14. Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur Violence Risk Assessment Study. Am J Psychiatry. 2000;157(4):566-72.
15. Vries AM, Liem M. Recidivism of juvenile homicide offenders. Behav Sci Law. 2011;29(4):483-98.
16. Kosterman R, Graham JW, Hawkins JD, et al. Childhood risk factors for persistence of violence in the transition to adulthood: a social development perspective. Violence and Victims. 2001;16(4):355-69.
17. Frey A, Ruchkin V, Martin A, et al. Adolescents in transition: school and family characteristics in the development of violent behaviors entering high school. Child Psychiatry Hum Dev. 2009;40(1):1-13.
18. Lagasse LL, Hammond J, Liu J, et al. Violence and delinquency, early onset drug use, and psychopathology in drug-exposed youth at 11 years. Ann N Y Acad Sci. 2006;1094:313-8.
19. Reyes JC, Moscoso M, Vélez CN, et al. Risk and protective factors associated with youth violence among secondary school students in a nationally representative sample in Puerto Rico. Bol Asoc Med P R. 2004;96(4):253-60.
20. Gudlaugsdottir GR, Vilhjalmsson R, Kristjansdottir G, et al. Violent behaviour among adolescents in Iceland: a national survey. Int J Epidemiol. 2004;33(5):1046-51.
21. Saner H, Ellickson P. Concurrent risk factors for adolescent violence. J Adolesc Health. 1996;19(2):94-103.
22. Valois RF, Vincent ML, McKeown RE, et al. Adolescent risk behaviors and the potential for violence: a look at what’s coming to campus. J Am Coll Health. 1993;41(4):141-7.
23. Baxendale S, Lester L, Johnston R, et al. Risk factors in adolescents’ involvement in violent behaviours. J Aggress Confl Peace Res. 2015;7(1):2-18.
24. Kinoshita Y, Shimodera S, Nishida A, et al. Psychotic-like experiences are associated with violent behavior in adolescents. Schizophr Res. 2011;126(1–3):245-51.
25. Rajan S, Namdar R, Ruggles KV. Aggressive and violent behaviors in the school environment among a nationally representative sample of adolescent youth. J Sch Health. 2015;85(7):446-57.
26. Loeber R, Green SM, Lahey BB, et al. Physical fighting in childhood as a risk factor for later mental health problems. J Am Acad Child Adolesc Psychiatry. 2000;39(4):421-8.
27. Farrington DP. Early predictors of adolescent aggression and adult violence. Violence Vict. 1989;4(2):79-100.
28. Choi Y, Harachi TW, Gillmore MR, et al. Are multiracial adolescents at greater risk? Comparisons of rates, patterns, and correlates of substance use and violence between monoracial and multiracial adolescents. Am J Orthopsychiatry. 2006;76(1):86-97.
29. Grunwald HE, Lockwood B, Harris PW, et al. Influences of neighborhood context, individual history and parenting behavior on recidivism among juvenile offenders. J Youth Adolesc. 2010;39(9):1067-79.
30. Loeber R, Pardini D, Homish DL, et al. The prediction of violence and homicide in young men. J Consult Clin Psychol. 2005;73(6):1074-88.
31. Fries L, Grogan-Kaylor A, Bares C, et al. Gender differences in predictors of self-reported physical aggression: exploring theoretically relevant dimensions among adolescents from Santiago, Chile. Int Perspect Psychol. 2013;2(4).
32. Herrenkohl TI, Lee J, Hawkins JD. Risk versus direct protective factors and youth violence: Seattle Social Development Project. Am J Prev Med. 2012;43(2 Suppl 1):S41-56.
33. Tolan PH, Thomas P. The implications of age of onset for delinquency risk. II: Longitudinal data. J Abnorm Child Psychol. 1995;23(2):157-81.
34. Narayan AJ, Chen M, Martinez PP, et al. Interparental violence and maternal mood disorders as predictors of adolescent physical aggression within the family. Aggress Behav. 2015;41(3):253-66.
35. Blitstein JL, Murray DM, Lytle LA, et al. Predictors of violent behavior in an early adolescent cohort: similarities and differences across genders. Health Educ Behav. 2005;32(2):175-94.
36. Sourander A, Elonheimo H, Niemela SF, et al. Childhood predictors of male criminality: a prospective population-based follow-up study from age 8 to late adolescence. J Am Acad Child Adolesc Psychiatry. 2006;45(5):578-86.
37. Mattila VM, Parkkari JP, Rimpelä AH. Risk factors for violence and violence-related injuries among 14- to 18-year-old Finns. J Adolesc Health. 2006;38(5):617-20.
38. Duke NN, Pettingell SL, McMorris BJ, et al. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125(4):e778-86.
39. Yun I, Ball JD, Lim H. Disentangling the relationship between child maltreatment and violent delinquency: using a nationally representative sample. J Interpers Violence. 2011;26(1):88-110.
40. Stewart A, Livingston M, Dennison S. Transitions and turning points: examining the links between child maltreatment and juvenile offending. Child Abuse Negl. 2008;32(1):51-66.
41. Lansford JE, Miller-Johnson S, Berlin LJ, et al. Early physical abuse and later violent delinquency: a prospective longitudinal study. Child Maltreat. 2007;12(3):233-45.
42. Gover AR. The effects of child maltreatment on violent offending among institutionalized youth. Violence Vict. 2002;17(6):655-68.
43. Crooks CV, Scott KL, Wolfe DA, et al. Understanding the link between childhood maltreatment and violent delinquency: what do schools have to add?. Child Maltreat. 2007;12(3):269-80.
44. Lee C, Cronley C, White HR, et al. Racial differences in the consequences of childhood maltreatment for adolescent and young adult depression, heavy drinking, and violence. J Adolesc Health. 2012;50(5):443-9.
45. Thurnherr J, Berchtold A, Michaud PA, et al. Violent adolescents and their educational environment: a multilevel analysis. J Dev Behav Pediatr. 2008;29(5):351-9.
46. Wright DR, Fitzpatrick KM. Violence and minority youth: the effects of risk and asset factors on fighting among African American children and adolescents. Adolescence. 2006;41(162):251-62.
47. Resnick MD, Ireland M, Borowsky I. Youth violence perpetration: What protects? What predicts? Findings from the National Longitudinal Study of Adolescent Health. J Adolesc Health. 2004;35(5):424.e1-10.
48. Widom CS. The cycle of violence. Science. 1989;244(4901):160-6.
49. Swahn MH, Bossarte RM, Palmier JB, et al. Psychosocial characteristics associated with frequent physical fighting: findings from the 2009 National Youth Risk Behavior Survey. Inj Prev. 2013;19(2):143-6.
50. Ellickson PL, McGuigan KA. Early predictors of adolescent violence. Am J Public Health. 2000;90(4):566-72.
51. Kingery PB, Zimmerman RS, Biafora F. Risk factors for violent behaviors among ethnically diverse urban adolescents: beyond race/ethnicity. Sch Psychol. 1996;17(2):171-88.
52. Sitnick SL, Shaw DS, Weaver CM, et al. Early childhood predictors of severe youth violence in low-income male adolescents. Child Dev. 2017;88(1):27-40.
53. Atkins R. The association of personality type in childhood with violence in adolescence. Res Nurs Health. 2007;30(3):308-19.
54. Petras H, Chilcoat HD, Leaf PJ, et al. Utility of TOCA-R scores during the elementary school years in identifying later violence among adolescent males. J Am Acad Child Adolesc Psychiatry. 2004;43(1):88-96.
55. Hemphill SA, Smith R, Toumbourou JW, et al. Modifiable determinants of youth violence in Australia and the United States: A longitudinal study. Aust N Z J Criminol. 2009;42(3):289-309.
56. Brook JS, Brook DW, Whiteman M. Growing up in a violent society: longitudinal predictors of violence in Colombian adolescents. Am J Community Psychol. 2007;40(1–2):82-95.
57. Sijtsema JJ, Kretschmer T, van Os T. The Structured Assessment of Violence Risk in Youth in a large community sample of young adult males and females: the TRAILS study. Psychol Assess. 2015;27(2):669-77.
58. Kaya F, Bilgin H, Singer MI. Contributing factors to aggressive behaviors in high school students in Turkey. J Sch Nurs. 2012;28(1):56-69.
59. Ruback RB, Shaffer JN, Clark VA. Easy access to firearms: juveniles’ risks for violent offending and violent victimization. J Interpers Violence. 2011;26(10):2111-38.
60. Bernat DH, Oakes JM, Pettingell SL, et al. Risk and direct protective factors for youth violence: results from the National Longitudinal Study of Adolescent Health. Am J Prev Med. 2012;43(2 Suppl 1):S57-66.
61. Pickett W, Iannotti RJ, Simons-Morton B, et al. Social environments and physical aggression among 21,107 students in the United States and Canada. J Sch Health. 2009;79(4):160-8.
62. Thomas SP, Smith H. School connectedness, anger behaviors, and relationships of violent and nonviolent American youth. Perspect Psychiatr Care. 2004;40(4):135-48.
63. Swahn MH, Donovan JE. Correlates and predictors of violent behavior among adolescent drinkers. J Adolesc Health. 2004;34(6):480-92.
64. Herrenkohl TI, Maguin E, Hill KG, et al. Developmental risk factors for youth violence. J Adolesc Health. 2000;26(3):176-86.
65. Murphy SM, McPherson S, Robinson K. Non-medical prescription opioid use and violent behaviour among adolescents. J Child Adolesc Ment Health. 2014;26(1):35-47.
66. Henry DB, Tolan PH, Gorman-Smith D, et al. Risk and direct protective factors for youth violence: results from the Centers for Disease Control and Prevention’s Multisite Violence Prevention Project. Am J Prev Med. 2012;43(2 Suppl 1):S67-75.
67. Borowsky IW, Ireland M, Resnick MD. Violence risk and protective factors among youth held back in school. Ambul Pediatr. 2002;2(6):475-84.
68. Ferguson CJ. Video games and youth violence: a prospective analysis in adolescents. J Youth Adolesc. 2011;40(4):377-91.
69. Swaim RC, Henry KL, Kelly K. Predictors of aggressive behaviors among rural middle school youth. J Prim Prev. 2006;27(3):229-43.
70. Smokowski PR, Guo S, Cotter KL, et al. Multilevel risk factors and developmental assets associated with aggressive behavior in disadvantaged adolescents. Aggress Behav. 2016;42(3):222-38.
71. Brook DW, Brook JS, Rosen Z, et al. Early risk factors for violence in Colombian adolescents. Am J Psychiatry. 2003;160(8):1470-8.
72. Smokowski PR, Guo S, Evans CB, et al. Risk and protective factors across multiple microsystems associated with internalizing symptoms and aggressive behavior in rural adolescents: modeling longitudinal trajectories from the Rural Adaptation Project. Am J Orthopsychiatry. 2017;87(1):94-108.
73. Nansel TR, Overpeck MD, Haynie DL, et al. Relationships between bullying and violence among US youth. Arch Pediatr Adolesc Med. 2003;157(4):348-53.
74. Kim YS, Leventhal BL, Koh YJ, et al. School bullying and youth violence: causes or consequences of psychopathologic behavior?. Arch Gen Psychiatry. 2006;63(9):1035-41.
75. Logan-Greene P, Nurius PS, Herting JR, et al. Multi-domain risk and protective factor predictors of violent behavior among at-risk youth. J Youth Stud. 2011;14(4):413-29.
76. Scherzer T, Pinderhughes HL. Violence and gender: reports from an urban high school. Violence Vict. 2002;17(1):57-72.
77. Djerboua M, Chen BE, Davison CM. Physical fighting, fighting-related injuries and family affluence among Canadian youth. BMC Public Health. 2016;16(1):199.
78. McMahon SD, Todd NR, Martinez A, et al. Aggressive and prosocial behavior: community violence, cognitive, and behavioral predictors among urban African American youth. Am J Community Psychol. 2013;51(3–4):407-21.
79. Weaver CM, Borkowski JG, Whitman TL. Violence breeds violence: childhood exposure and adolescent conduct problems. J Community Psychol. 2008;36(1):96-112.
80. McCabe KM, Lucchini SE, Hough RL, et al. The relation between violence exposure and conduct problems among adolescents: a prospective study. Am J Orthopsychiatry. 2005;75(4):575-84.
81. White HR, Loeber R, Stouthamer-Loeber M, et al. Developmental associations between substance use and violence. Dev Psychopathol. 1999;11(4):785-803.
82. Tschann JM, Flores E, Pasch LA, et al. Emotional distress, alcohol use, and peer violence among Mexican-American and European-American adolescents. J Adolesc Health. 2005;37(1):11-8.
83. Molcho M, Harel Y, Dina LO. Substance use and youth violence. A study among 6th to 10th grade Israeli school children. Int J Adolesc Med Health. 2004;16(3):239-51.
84. Sussman S, Skara S, Weiner MD, et al. Prediction of violence perpetration among high-risk youth. Am J Health Behav. 2004;28(2):134-44.
85. Shetgiri R, Boots DP, Lin H, et al. Predictors of weapon-related behaviors among African American, Latino, and White Youth. J Pediatr. 2016;171:277-82.
86. Sousa S, Correia T, Ramos E, et al. Violence in adolescents: social and behavioural factors. Gac Sanit. 2010;24(1):47-52.
87. Wang FM, Chen JQ, Xiao WQ, et al. Peer physical aggression and its association with aggressive beliefs, empathy, self-control, and cooperation skills among students in a rural town of China. J Interpers Violence. 2012;27(16):3252-67.
88. Johnson JG, Cohen P, Smailes E, et al. Adolescent personality disorders associated with violence and criminal behavior during adolescence and early adulthood. Am J Psychiatry. 2000;157(9):1406-12.
89. Calvete E. Justification of violence and grandiosity schemas as predictors of antisocial behavior in adolescents. J Abnorm Child Psychol. 2008;36(7):1083-95.
90. Heide KM, Solomon EP. Female juvenile murderers: biological and psychological dynamics leading to homicide. Int J Law Psychiatry. 2009;32(4):244-52.
91. Viljoen JL, McLachlan K, Vincent GM. Assessing violence risk and psychopathy in juvenile and adult offenders: a survey of clinical practices. Assessment. 2010;17(3):377-95.


