| Author | Affiliation |
| Stephanie Spring, DO | Saint Vincent Health System, Department of Emergency Medicine, Erie, Pennsylvania |
| Richard Anderson, MD | Saint Vincent Health System, Department of Emergency Medicine, Erie, Pennsylvania |
| Jestin N. Carlson, MD, MSc | Saint Vincent Health System, Department of Emergency Medicine, Erie, Pennsylvania; Unviersity of Pittsburgh School of Medicine, Department of Emergency Medicine, Pittsburgh, Pennsylvania |
A 13-year old female patient presented to the emergency department (ED) with four days of intermittent non-radiating, left upper quadrant pain, associated with non-bloody, non-bilious emesis and decreased appetite. The patient had been evaluated by a gastroenterologist three months prior for abdominal pain. At that time an esophagogastroduodenoscopy revealed a trichobezoar in the stomach too large for endoscopic removal. Elective surgical removal had been offered to the patient, although surgery had not yet been scheduled.
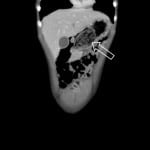
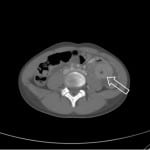
Vital signs were within reference limits for the patient’s age. The patient had tenderness throughout the left upper quadrant, however there was no guarding or rebound tenderness. The patient underwent computed tomography (CT) of the abdomen and pelvis, which confirmed the thichobezoar in the stomach and intussusception of the bowel (Figures 1 and 2) consistent with Rapunzel Syndrome.
DISCUSSION
Rapunzel Syndrome, named after the Brothers Grimm’s fairy tale princess with long hair by the same name, is a rare disorder resulting from trichobezoar formation and subsequent extension of the tail of the bezoar into small bowel associated with trichophagia (Figure 1).1 The tail of the hair acts as a lead point, causing intussusception of the bowel (Figure 2). Bezoars are rare, occurring in less than 1% of patients undergoing upper gastrointestinal endoscopy and only a small number of patients have been reported with Rapunzel Syndrome.1-3 While many patients may undergo CT scans, ultrasound and plain radiographs have also been used to establish the diagnosis.4,5 Management includes removal via endoscopy or elective surgery although complications including gastric perforation has been reported.6,7 The patient was transferred to a pediatric hospital where she underwent an exploratory laparotomy including bezoar removal from both the stomach and jejunum. Over the next 48 hours the patient’s diet was advanced and was discharged home on post-operative day five.
Figure 1. Bezoar in the stomach.
Figure 2. Target sign signifying intussusception. The arrow points to the tail of the bezoar acting as a lead point for the intussusception.
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jestin Carlson, MD, MSc, Saint Vincente Health Center, 232 West 25th St. Erie, PA 16544. Email: jcarlson@svhs.org.
Submission history: Submitted November 4, 2014; Revision received November 5, 2014; Accepted November 25, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Balik E, Ulman I, Taneli C, et al. The ”Rapunzel syndrome” a case report and review of the literature. Eur J Pediatr Surg. 1993;3(3):171-3.
- Kadian RS, Rose JF, Mann NS. Gastric bezoars—spontaneous resolution. Am J Gastroenterol. 1978;70(1):79-82.
- Singla SL, Rattan KN, Kaushik N, et al. Rapunzel syndrome — a case report. Am J Gastroenterol. 1999;94(7):1970-1.
- Belsky J, Whitcomb V, Zimmerman E, et al. Rapunzel Syndrome: diagnosis via radiograph and history. Pediatr Emerg Care. 2014;30(5):352-3
- Middleton E, Macksey LF, Phillips JD. Rapunzel Syndrome in a pediatric patient: a case report. AANA J. 2012;80(2)115-9
- Fallon SC, Slater BJ, Larimer EL, et al. The surgical management of Rapunzel Syndrome: a case series and literature review. J Pediatr Surg. 2013;48(4):830-4.
- Pul N, Pul M. The Rapunzel Syndrome (trichobezoar) causing gastric perforation in a child: a case report. Eur J Pediatr. 1996;155(1):18-9.