| Author | Affiliation |
|---|---|
| Kim L. Askew, MD | Wake Forest University School of Medicine, Department of Emergency Medicine, Winston-Salem, North Carolina |
| Debra Weiner, MD | Boston Children’s Hospital, Division of Emergency Medicine, Boston, Massachusetts |
| Charles Murphy, MD | Mount Sinai Medical Center, Department of Emergency Medicine, New York, New York |
| Myto Duong, MD | Southern Illinois University, Department of Emergency Medicine, Carbondale, Illinois |
| James Fox, MD | Duke University Medical Center, Department of Pediatrics, Durham, North Carolina |
| Sean Fox, MD | Carolinas Medical Center, Department of Emergency Medicine, Charlotte, North Carolina |
| James C. O’Neill, MD | Wake Forest University School of Medicine, Department of Emergency Medicine, Winston-Salem, North Carolina |
| Milan Nadkarni, MD | Wake Forest University School of Medicine, Department of Emergency Medicine, Winston-Salem, North Carolina |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Supplementary information
ABSTRACT
Introduction
As emergency medicine (EM) has become a more prominent feature in the clinical years of medical school training, national EM clerkship curricula have been published to address the need to standardize students’ experiences in the field. However, current national student curricula in EM do not include core pediatric emergency medicine (PEM) concepts.
Methods
A workgroup was formed by the Clerkship Directors in Emergency Medicine and the Pediatric Interest Group of the Society of Academic Emergency Medicine to develop a consensus on the content to be covered in EM and PEM student courses.
Results
The consensus is presented with the goal of outlining principles of pediatric emergency care and prioritizing students’ exposure to the most common and life-threatening illnesses and injuries.
Conclusion
This consensus curriculum can serve as a guide to directors of PEM and EM courses to optimize PEM knowledge and skills education.
INTRODUCTION
Much attention has been given to the role of emergency departments (ED) in healthcare and in the training of future physicians. The Macy report emphasized the need for establishing academic departments in emergency medicine (EM) in medical schools and for training in EM.1 The Institute of Medicine’s (IOM) report on emergency care highlighted issues that affect the delivery of medical care in the EM arena and raised concerns about current pediatric care.2 Notably, pediatric patients account for more than 25% of ED visits and most do not occur in cities with specialized pediatric care.2 As such, the IOM report emphasized the need to augment pediatric-specific training throughout the healthcare system. Most medical schools now offer experiences in EM and exposure to pediatric emergency medicine (PEM), either as a stand-alone course or as part of their pediatrics or EM courses. This earlier exposure to PEM in medical school provides an invaluable opportunity for students to learn about the unique challenges and complexities of children with acute, undifferentiated complaints.
There have been numerous medical student curriculum statements and revisions related to EM and pediatrics. 3–7 Both a third- and fourth-year EM student curriculum have been published by members of Clerkship Directors in Emergency Medicine (CDEM).3–5 Although there are concepts and content applicable to PEM in each, neither includes pediatric-specific topics. The Council of Medical Student Education in Pediatrics (COMSEP) pediatric clerkship curriculum addresses pediatric emergencies and corresponding diagnoses that should be covered in the core pediatric clerkship, and those that should be mastered outside of the core clerkship, but does not specify which should be covered during a PEM or EM clerkship.7 We therefore created a consensus curriculum that indicates which PEM chief complaints and conditions should be covered during PEM rotations, and which should be covered in EM rotations with exposure to pediatric patients.
METHODS
A committee was convened by CDEM in conjunction with the Pediatric Interest Group of the Society of Academic Emergency Medicine (SAEM) to develop a medical student curriculum in PEM. The group consisted of eight EM and/or PEM physicians from six institutions. Members possessed dual board certifications in pediatrics and EM (1), EM and PEM (2), or pediatrics and PEM (5). All members had served as a course director in the third or fourth year of medical school training at their institution. The committee met from June 2010 to June 2011 during announced public meeting at national conferences (ACEP, SAEM) to allow other educators to participate via teleconferences several times throughout the year and by email on routine basis. The group used Kern’s model for the development of a curriculum and followed the National Institute of Health guidelines for consensus building to determine the appropriate student audience for the curriculum and to formulate the content that should be included in the PEM curriculum.8–9 The group reviewed prior published curricula in EM and pediatrics, along with resources from the Liaison Committee on Medical Education (LCME) and Accreditation Council for Graduate Medical Education (ACGME) to assist in establishing the audience, goals and objectives, and knowledge content.3,4,7,10–11 In establishing content, the group reviewed the frequency with which complaints are seen in the ED, prior exposure and knowledge base from previous clerkships, and topic relevance within PEM.12
RESULTS
After review of the current published national curricula, several opportunities existed for development of a PEM student curriculum. The consensus was that the curriculum should be targeted to the fourth-year medical student completing a four-week course in PEM, taking advantage of the knowledge and skills students had obtained during their core pediatric clerkship and potentially an EM clerkship. The group also concluded that certain PEM topics could be addressed in an EM clerkship with a PEM component. These topics would address the current absence of PEM topics in the current CDEM national curricula. Therefore, a two-tiered system was built for the curriculum: 1) topics for a fourth-year medical student course in PEM, and 2) topics that should be covered in an EM clerkship with a PEM component.
The working group then focused on the development of specific goals and objectives that would guide the experience of the four-week PEM course. To promote continuity between undergraduate and graduate medical education, the group composed objectives based on ACGME core competencies (Appendix). These objectives can be assessed through observation on shifts, standardized and virtual patients, self-directed learning, simulation, and other means.
Subsequently, the committee focused on knowledge content. In evaluating topics that were felt to be important for the fourth-year student completing a PEM course, the committee realized there were several features of PEM that needed to be considered:
Patients typically present with complaints/symptoms, rather than a diagnosis.
The evaluation and management of pediatric patients is affected by their unique anatomy, physiology, and psychosocial development.
Certain complaints are so frequently encountered in PEM that they should be included in this curriculum.
Complaints and diagnoses have seasonal variability.
Pediatric patients are at greater risk for medication and treatment errors.
The committee agreed that a general approach to the undifferentiated pediatric patient was an essential component of a PEM curriculum to address factors #2 and #5 above. The committee developed its knowledge content on a chief complaint perspective, rather than a disease process, to address factor #1. Ten complaints were agreed upon (Table 1). These complaints were divided into two categories: 1) complaints students would be expected to evaluate firsthand in the ED, and 2) complaints to which students should be exposed (in a clinical, didactic, simulation, or other environment). This classification was developed due to the seasonal nature of PEM, the frequency the complaint is encountered, and the unique pathophysiology of certain disease process to pediatrics.
Table 1. Pediatric emergency medicine (PEM) topics/complaints to be covered in PEM/EM clerkships.
| Topic | PEM course | EM course with pediatric exposure | Overlap topics with EM national curricula |
|---|---|---|---|
| General approach to pediatric patient | X | X | |
| Complaints that students should evaluate clinically | |||
| Respiratory difficulty | X | X | X |
| Fever | X | ||
| Abdominal pain/vomiting | X | X | |
| Altered mental status | X | X | |
| Trauma/musculoskeletal injury | X | X | |
| Complaints to which students should be exposed | |||
| Limp | X | ||
| Crying child | X | ||
| Headache | X | X | |
| Ingestion | X | X | |
| Shock/cardiac arrest | X | X | |
EM, emergency medicine
While specific complaints appear repeatedly in the ED (e.g fever), predicting which specific diagnoses a student will encounter cannot be assured, especially given the seasonal variability in PEM (e.g. bronchiolitis). The group, however, agreed that students completing a PEM course should have an understanding of the presentation, diagnosis, and management of specific diagnoses in PEM. The group compiled a list of specific disease processes in a similar fashion as the complaints, those to be evaluated clinically and to be exposed via other educational modalities. These disease processes are divided by organ system in Table 2.
Table 2. Specific conditions by system that students should evaluate clinically or be exposed to during a pediatric emergency medicine (PEM) course and their applicability with national EM curricula.
| Condition | Evaluate during PEM course | Exposure during PEM course | Align with EM curricula |
|---|---|---|---|
| Neurological | |||
| a. Head injury | X | X | |
| b. Seizure | X | ||
| c. Apparent life threatening event | X | ||
| Ear/nose/throat | |||
| a. Otitis media | X | ||
| b. Upper respiratory infection | X | ||
| c. Pharyngitis | X | ||
| Respiratory | |||
| a. Asthma | X | X | X |
| b. Bronchiolitis | X | X | |
| c. Croup | X | ||
| Cardiac | |||
| a. Cardiac arrest | X | X | |
| Gastrointestinal | |||
| a. Gastroenteritis | X | ||
| b. Dehydration | X | ||
| c. Intussusception | X | X | |
| d. Pyloric stenosis | X | X | |
| Musculoskeletal | |||
| a. Extremity fracture | X | ||
| b. Nursemaid’s elbow | X | ||
| Genitourinary | |||
| a. Sexually transmitted disease | X | X | |
| b. Abuse | X | X | |
| c. Testicular torsion | X | X | |
| Dermatologic | |||
| a. Viral exanthem | X | ||
| b. Henoch-Schönlein purpura | X | ||
| c. Tinea | X | ||
| Psychiatric | |||
| a. Behavior/emotional disturbance | X | X | |
| Endocrine | |||
| a. Hypo/hyperglycemia | X | X | |
Figure
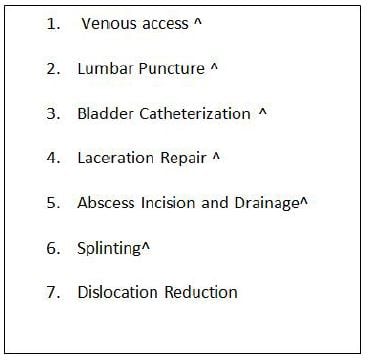
Procedures to which students should have exposure during pediatric emergency medicine course (^Procedures that align with National EM Curricula1, 2).
The group also considered procedures that fourth-year medical students should experience during a PEM course. Procedures selected are those performed frequently in the care of pediatric patients in most EDs. The committee felt the procedural education should address indications, contraindications, complications, appropriate equipment, explanation of the procedure to families and patients, elements of consent when required, and aftercare, in addition to the specifics of performing the procedure.
Finally, after completing the development of the PEM course content, the content was reviewed and compared to national EM curricula.3–5 Many areas of overlap were noted between the knowledge content areas of complaints and procedures. The committee felt two content areas within the PEM curriculum should be addressed by EM rotations with pediatric exposure: 1) Approach to the pediatric patient and 2) Respiratory difficulty. The committee, therefore, recommends that an EM course with a PEM component incorporate these topics into their curriculum. Given the amount of overlap in the complaints in both the national EM curricula and our consensus curriculum, EM course directors may want to consider exploring pediatric perspectives of these common complaints as part of their curriculum (Table 1).
DISCUSSION
As with any medical course, the experience that may be provided and the content that could be covered can be daunting. One of the greatest challenges in developing this curriculum was determining the topics to be covered. Multiple factors led to this challenge, such as differing educators’ perspectives on topic importance, expectations of what a medical student should know and be exposed to, and consideration of institutions resources and patient volumes. Ultimately, some course directors may place higher importance on some complaints/conditions which are not listed here. The committee attempted to balance essential PEM topics (shock, cardiac arrest, trauma) with more frequently encountered complaints (respiratory difficulty, abdominal pain), and complaints that have unique pediatric considerations (limp, crying child). As for the procedures, the committee attempted to identify procedures performed frequently in all EDs and appropriate for a medical student level of training. Other procedures, such as procedural sedation and bedside ultrasound, may not be performed at all institutions for pediatric patients and were therefore omitted from the recommended curriculum. A future goal of the committee will be to seek feedback from course directors about the curriculum content and implementation for purposes of determining if the curriculum needs revision, as was done with the EM national curriculum.2,3
Implementation of this curriculum at individual institutions will undoubtedly be affected by the specifics of the ED, institution resources and strengths, patient population and location, seasonal variability of conditions, among other variables. By limiting complaints and diagnoses in the “should evaluate clinically” to those most frequently encountered complaints in EDs, the committee hoped to prevent any conflict with LCME standards for individual course directors. LCME educational standards state that a course must ensure that students have some way of seeing expected diagnoses if not encountered clinically.10 By classifying complaints and diagnoses as “should have exposure,” individual course directors can use strengths of their institution to develop ways to expose students to the less frequently seen complaints. In order to provide further resources, CDEM plans to develop resources that can help course directors incorporate this curriculum and ensure students are exposed to all conditions/diagnoses.
Lastly, the ACGME has developed milestones which pediatric and EM residency programs are incorporating in the evaluation of their residents.13,14 The AAMC is in the final stages of developing entrustable professional activities (EPAs) for medical students.15 Many of the Level 1 residency milestones and student EPAs are based on the learner’s ability to accurately obtain a history, perform a physical exam, and to develop an appropriate differential diagnosis and plan. The milestones expect learners at the beginning of residency to be able to recognize abnormal vitals and begin the process of recognizing higher acuity patients. The nature of PEM and the objectives of this curriculum will allow course directors and faculty to observe a student’s ability to initially evaluate a patient, from history to differential, while developing a plan of care for certain complaints in PEM. To address the need of learners to begin to recognize higher acuity patients, the approach-to-pediatric-patients topic will need to encompass the range of abnormal vital signs, the art of recognizing the subtle findings in children that suggest sicker patients, among other components. Therefore, this curriculum should allow course directors to evaluate learners in these areas, but will also provide students further opportunity to develop the skills residency programs expect of them upon entry. These areas also need to be addressed in future evaluation of this curriculum’s adoption by course directors and feedback about its contents.
LIMITATIONS
The curriculum is the consensus result of a working group of eight educators. The recommendations presented here may vary with different members or with a larger number of committee members. Future feedback on the curriculum will need to address this limitation. Also, this curriculum will need to be incorporated by course directors based on their own institution’s strengths and resources. Each institution will have differing abilities to support the curriculum. CDEM plans on developing online resources for institutions and students to use to address topics in the curriculum, which may assist in institutions with lower pediatric volume or more limited resources.
CONCLUSION
Given the role of the ED in the care of children, biopsychosocial factors specific to children, and the lack of a national medical student curriculum in PEM, a consensus curriculum was created by a subcommittee of CDEM and SAEM Pediatric Interest Group. This consensus curriculum can serve as a guide to directors of PEM and EM courses to optimize PEM knowledge and skills education. The committee hopes that by standardizing the curriculum of PEM rotations, the recognition of the uniqueness of emergently ill and injured children will begin at the medical student level, and continue throughout training and practice.
Supplementary Information
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Kim L. Askew, MD; Department of Emergency Medicine, Wake Forest University School of Medicine, Medical Center Blvd, Winston-Salem, NC 27157. Email: kaskew@wakehealth.edu 9 / 2014; 15:647 – 651
Submission history: Revision received October 14, 2013; Submitted March 11, 2014; Accepted April 15, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Macy J The role of emergency medicine in the future of American medical care. Ann Emerg Med. 1995; 25:230-233
2 IOM report: the future of emergency care in the United States health system. Acad Emerg Med. 2006; 17:638-644
3 Tews MC, Wyte CM, Coltman M Developing a third year emergency medicine medical student curriculum; a syllabus of content. Acad Emerg Med. 2011; 18:S36-40
4 Manthey DE, Coates WC, Ander DS Report of the task force on national fourth year medical student emergency medicine curriculum guide. Ann Emerg Med. 2006; :47 e1-7
5 Manthey DE, Ander DS, Gordon DC Emergency medicine clerkship curriculum: an update and revision. Acad Emerg Med. 2010; 17:638-634
6 Konopasek L, Sanguino S, Bostwick S . COMSEP and APPD Pediatric Subinternship Curriculum. 2011;
7 . COMSEP General Pediatric Clerkship Pediatric Emergencies. ;
8 Kern D, Thomas P, Hughes M . Curriculum Development for Medical Education. 2009;
9 Nair R, Aggarwal R, Khanna D Methods of formal consensus in classification/diagnostic criteria and guideline development. Semin Arthritis Rheum. 2011; 41:95-105
10 . Standards for Accreditation of Medical Education Programs Leading to the M.D. Degree 2010. ;
11 . ACGME Outcome Project. ;
12 Middleton K Pediatric Emergency Department Visits in the United States, 2003–2005. . 2007;
13 . The Pediatrics Milestone Project. ;
14 . The Pediatrics Milestone Project. ;
15 Aschenbrener R, Englander R Core Entrustable Professional Activities for Entering Residency. MedEdPORTAL. 2013;


