| Author | Affiliation |
|---|---|
| Monica H. Swahn, PhD, MPH | Georgia State University, School of Public Health, Atlanta, Georgia |
| Sarah Braunstein, BS | Georgia State University, School of Public Health, Atlanta, Georgia |
| Rogers Kasirye, MA | Uganda Youth Development Link, Kampala, Uganda |
Introduction
Methods
Results
Discussion
ABSTRACT
Introduction:
The use of mobile phones and other technology for improving health through research and practice is growing quickly, in particular in areas with difficult-to-reach population or where the research infrastructure is less developed. In Sub-Saharan Africa, there appears to be a dramatic increase in mobile phone ownership and new initiatives that capitalize on this technology to support health promotion campaigns to change behavior and to increase health literacy. However, the extent to which difficult-to-reach youth in the slums of Kampala may own and use mobile phones has not been reported despite the burden of injuries, substance use, and HIV that they face. The purpose of this study is to determine the prevalence of mobile phone ownership and use in this high-risk population and to identify psychosocial characteristics that may differentiate those owning and using a phone from those who do not.
Methods:
We conducted secondary analyses of the Kampala Youth Survey (N=457). Data collection took place in 2011, and the survey was designed to quantify high-risk behaviors in a convenience sample of urban youth living on the streets or in the slums, 14–24 years of age, who were participating in a Uganda Youth Development Link drop-in center for disadvantaged street youth. We computed chi-square analyses to determine any significant differences in psychosocial characteristics based on phone ownership and use.
Results:
Overall, 46.9% of youth reported owning a mobile phone and ownership did not vary by sex but was more common among youth older than 18 years of age. Mobile phone ownership was also more common among those who reported taking care of themselves at night, who reported current drug use and who reported trading sex for money, food or other things.
Conclusion:
Given that nearly half of the youth own and use phones daily, new research is needed to determine next steps for mobile health (mhealth), including the feasibility of using mobile phones for data collection and interventions with this hard-to-reach population. Moreover, this technology may also be suitable for injury-specific research given that there were few differences with respect to injury-related variables in mobile phone ownership and usage.
INTRODUCTION
Mobile health, or mhealth, is a new emerging field of the “use of mobile information and communication technologies for improving health.”1 More specifically, mhealth includes using mobile technologies, which are any device or application that has cellular or wireless capabilities.2 Mhealth is used in many areas directly or indirectly related to health (e.g., education and awareness, service care centers, patient monitoring, disease outbreaks and surveillance, emergency medical response, health information system, distance learning education, and health financing).3 It is also used in the creation and adaptation of health interventions to individuals.4 The use of mhealth is rapidly emerging in developing countries.5 A United Nations Foundation and Vodafone Foundation collaborative report found that mobile phones usage in developing countries is the mostly widely used technology in health infrastructures.5
Mhealth programs appear to be frequently used in Africa, especially in Uganda, South Africa, and Rwanda.5 Mobile phone usage in Africa has soared.Mobile phones, which are more frequently used in Africa than landlines, have become integral in the economy of African countries.6 Although those who initially owned and used mobile phones were educated, young, wealthy, male and living in urban areas, more recently, cell phone use has expanded to include those living in rural areas, the elderly, and those with less resources.6 According to an Afro Barometer report, 72% of the respondents in 34 countries in Africa stated that they owned and used a mobile phone.7 In Uganda alone in 2009, there were about 9.5 million mobile phone subscribers.8
The use of mobile phones for public health campaigns ranges from management of chronic to communicable diseases.5 The use of SMS (short message service or text messaging) has become a popular, cost-effective way of promoting awareness, education, and intervention of diseases.5 The use of text messaging, specifically, has helped with medication and appointment adherence and public awareness.5 In a study on the use of mobile phone technology for the enhancement of the prevention of mother-to-child transmission of HIV program, women use cell phones to call their healthcare provider, for medication reminders and to schedule appointments.9 From a healthcare provider perspective, mobile phones are very helpful, less time consuming, and more cost efficient than traditional methods of seeing or interacting with patients.10
Even though there has been substantial growth in mobile phone use for health promotion and prevention campaigns, there seem to be very few mhealth strategies for violence and injury prevention research or programming specifically. One recent study used a low-cost mobile phone system for prospective surveillance of access to dog-bite care and risk of dog-bite exposure in Pakistan.11 Also, while research demonstrates that many population groups in Uganda have access to mobile phones, the extent to which these findings extend to poor youth who live in the slums of Kampala is not known. For example, one recent study demonstrated that about 27% of secondary school students in Mbarara, Uganda, have a mobile phone.12 The youth who live in the Kampala slums is a high priority for prevention strategies for a range of risk-behaviors including injuries and violence, but it can be difficult to reach these youth using traditional methods since most do not attend school.13,14
The goal of this study is to document the prevalence of mobile phone ownership and usage and also to examine factors that differentiate phone ownership. We hope that this information can assist in program planning and development and future research that seeks to improve the health and well-being of these marginalized youth using innovative mhealth approaches.
METHODS
Survey Participants and Recruitment
The overarching goal of the secondary analyses of this cross-sectional survey called the “Kampala Youth Survey,” conducted in May and June 2011, was to quantify and describe high-risk behaviors and exposures in a convenience sample of urban youth (14 to 24 years of age) living on the streets or in the slums who were participating in a Uganda Youth Development Link (UYDEL) drop-in center for disadvantaged street youth. UYDEL is a not-for-profit organization that operates 8 centers with a primary goal of reducing risk behaviors such as HIV acquisition and drug use among youth, primarily ages 12–24, living in the slums. The details of the survey have been described elsewhere.13–15 Brief, face-to-face surveys, lasting approximately 30 minutes, were administered by trained UYDEL staff across 8 drop-in centers across Kampala. Participating youth received snacks and transportation for completing the survey. No identifying information was collected and the surveys were completely anonymous. Surveys were administered in English or Uganda’s local language Luganda, and to the extent possible, in private locations, to ensure privacy of survey questions and responses. Recruitment took place using word-of-mouth, and youth between 14 and 24 years of age were invited to participate following the approved assent and consent process. The participation rate was 90.9%. Analyses are based on the 457 completed surveys (31.1% boys and 68.5% girls).
Survey Measures
The questionnaire, modeled from existing surveys, has been described elsewhere.13–17 Measures included demographic characteristics, family context, alcohol and drug use, injuries, violence, suicidal behaviors and sexual behavior, including victimization, and are available from the authors upon request. Information about mobile phone ownership and usage was based on two questions: 1. Do you have your own mobile phone; and 2. How often do you use a mobile phone (your own or someone else’s)? Youth were also asked if they “get on the internet,” if they have an email account and if they use Facebook.
Ethical Approvals
The study was approved by the Institutional Review Board at Georgia State University and by the Uganda National Council for Science and Technology. Funding to conduct the study was obtained from the International Strategic Initiative at Georgia State University and also from funds leveraged through collaboration with the Emory Center for Injury Control.
Data Analysis
We computed descriptive analyses and Wald F Chi Square analyses. The analytic sample (n=415) was constructed to include two groups: 1. Those who reported that they had a phone and used it daily (45.5%); 2. Those who did not have a phone and did not use a phone daily (54.5%). Participants who reported using a phone daily but who did not have their own phone or who had their own phone but did not use it daily were excluded from analyses (n=42).
RESULTS
The demographic characteristics and psychosocial characteristics of owning a mobile phone and using it daily are presented in the table. Owning a mobile phone did not vary by sex, but was more common among youth older than 18 years of age. Among those less than 18 years of age, 22.3% reported mobile phone ownership and use compared to 62.9% among those age 18 years or older (p<0.0001). Mobile phone ownership was also more common among those who reported taking care of themselves at night, who reported current drug use and who reported trading sex for money, food or other things.
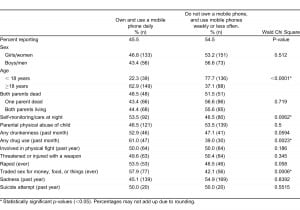
Associations between psychosocial correlates and mobile phone ownership and daily usage among youth living in the slums of Kampala (N=415).
In terms of using other technology, 9.3% of youth reported using the internet, 5.3% reported using an email account, and 4.9% reported using Facebook.
DISCUSSION
This study of mobile phone ownership and use among youth living in the slums of Kampala demonstrates surprisingly high levels of both mobile phone ownership and use given their high levels of poverty. The findings also demonstrate that while internet and social media use remains low in this population (less than 10%), use of mobile phones is much more common. Additionally, while phone ownership and use was more common among youth older than 18 and those who were monitoring themselves, there were few psychosocial factors that distinguished phone users from those who did not. The findings demonstrate that youth involved in high-risk behaviors including drug use and commercial sex had higher prevalence of owning and using mobile phones.
Some limitations restrict the interpretation of the findings of this study, including potential limited generalizability of the youth, limited questions about mobile phone use, underreporting of risk behaviors, and a relatively small sample size. However, it is unclear if any of these potential limitations would impact mobile phone ownership or use.
Because of the scarcity of data related to high-risk behaviors among vulnerable youth in Uganda, the current study provides support for future research that examines the feasibility of using mobile phones in service delivery and interventions with hard-to-reach populations. Also, because internet and social media use remains low in this population, mobile phones should be examined as potential viable strategies for data collection and interventions in the short term. Moreover, given that mobile phone ownership and use did not vary for most other factors examined, using mobile phones may be suitable for data collection on a range of issues including violence and injuries. While there are a number of studies examining use of mobile phones for both data collection and dissemination of health promotion messages, few studies if any, seem to be using this technology for injury specific research11 which may be another innovative approach for increasing the scope and reach for injury prevention research more broadly, particularly in underserved settings and populations.11
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.


