| Author | Affiliation |
|---|---|
| David I. Bruner, MD | Department of Emergency Medicine, Naval Medical Center, Portsmouth, Virginia |
| Lanny Littlejohn, MD | Department of Emergency Medicine, Naval Medical Center, Portsmouth, Virginia |
| Amy Pritchard, DO | Department of Emergency Medicine, Naval Medical Center, Portsmouth, Virginia |
ABSTRACT
While sinusitis is a common ailment, intracranial suppurative complications of sinusitis are rare and difficult to diagnose and treat. The morbidity and mortality of intracranial complications of sinusitis have decreased significantly since the advent of antibiotics, but diseases such as subdural empyemas and intracranial abscesses still occur, and they require prompt diagnosis, treatment, and often surgical drainage to prevent death or long-term neurologic sequelae. We present a case of an immunocompetent adolescent male with a subdural empyema who presented with seizures, confusion, and focal arm weakness after a bout of sinusitis.
INTRODUCTION
Intracranial suppurative lesions are life-threatening surgical emergencies that are rarely seen, difficult to diagnose, and can have serious long-term morbidity if not diagnosed and managed promptly and appropriately.1,2 When present, these lesions are found often in adolescents and can present with non-specific symptoms of fever and headache. While meningitis and encephalitis are often the first diagnoses considered in this case, space-occupying lesions such as abscesses or subdural empyemas must be considered as well, in particular when there are neurologic deficits, altered mental status or seizures at presentation. We present a case of an adolescent male who presented with confusion, seizure, and left arm weakness due to a subdural empyema.
CASE REPORT
A 16-year-old male presented to the ED with 1 day of a reported fever, a right temporal headache, and a witnessed tonic-clonic seizure. He arrived confused with left arm weakness noted as well. He had no past history of seizures. For the preceding week, he had complained of sinus congestion and received an antibiotic from his primary care provider several days prior.
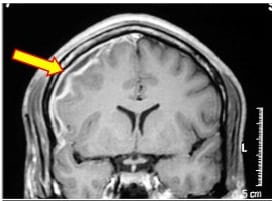
His review of systems was negative for rash, emesis or dyspnea. His medical history was unremarkable, and his immunizations were up to date. He lived at home with his family, none of whom were ill, and he took no medications or over-the-counter medications. He denied any allergies. Physical examination revealed a drowsy, but arousable, black male who was only oriented to person. His vital signs included a temperature of 36.6°C, pulse of 108, respiratory rate of 18, blood pressure of 118/54 mmHg, and an oxygen saturation of 100% on room air. His head and neck examination demonstrated only rhinorrhea but no meningismus, sinus tenderness, nystagmus or pupillary irregularity. His neurologic examination revealed isolated 0/5 weakness in the left upper extremity and confusion to time and place. His leg strength and reflexes were normal, but his gait was not tested. The remainder of his examination was normal. Diagnostic testing included an initial computed tomography (CT) that showed a right, frontal subdural hypodensity. His complete blood count was remarkable only for a white blood cell count of 17,300 cells/mm with a left shift. His basic metabolic panel showed normal electrolytes, glucose, and renal function. A magnetic resonance imaging (MRI) was obtained showing right frontal sinusitis with right subdural space extension (Figure). A subsequent lumbar puncture demonstrated no organisms on gram stain and 3 white blood cells per high power field.
He was diagnosed with a subdural empyema and started on intravenous ceftriaxone and vancomycin. He received supportive care and pain control, and he was admitted to the pediatric intensive care unit (PICU) with neurosurgical consultation. His empyema was surgically drained on the day of presentation. The patient slowly recovered in the PICU without any further seizure activity. At the time of discharge, his left arm strength was 4/5 and he had a normal mental status. He was kept on anti-seizure prophylaxis for 6 months without recurrent seizures, and his strength returned to normal with physical therapy over the subsequent 6 months.
DISCUSSION
Subdural empyemas are neurosurgical emergencies that require prompt recognition and management to salvage a good functional neurologic outcome. These lesions progress rapidly and cause increased intracranial pressure leading to coma and death within 24 to 48 hours if untreated.2,3 Historically, these rare complications occurred secondary to otitis media, but currently they are seen more frequently as a complication of bacterial sinusitis.4 A subdural empyema is a known but rare suppurative complication of bacterial sinusitis. The suppurative complications of sinusitis can be divided into two categories – orbital and intracranial. Orbital complications classically occur from infection of the ethmoid air cells and can include orbital cellulitis, orbital abscesses, and subperiostial abscess (Pott’s puffy tumor). Intracranial complications include subdural empyema, epidural abscess, intracerebral abscess, meningitis, and thrombosis of the cavernous and other dural sinuses. Subdural empyema is the most common intracranial complication associated specifically with sinusitis. 3,5 Historically, subdural empyema was the most common intracranial suppurative complication overall, but epidural abscess may now be the more common entity.6 However, of the possible suppurative intracranial complications, subdural empyemas have the worst long term outcomes.3There are two potential mechanisms for subdural empyema formation following a bout of bacterial sinusitis. First and most commonly, a retrograde thrombophlebitis occurs via the valveless diploic veins and seeds the subdural space. Second, direct extension can occur from an infected sinus. Frontal sinusitis is the most common culprit in this instance. Close anatomic proximity of the sinus to the subdural space allows for this direct extension. The infection may also erode the facial bones causing osteomyelitis and subsequent direct extension as well. Once the infectious process invades the subdural space, a rapid clinical deterioration is common.3,6 Subdural empyemas are often polymicrobial. The most common pathogens are micoraerophilic and anaerobic gram positive cocci, but anaerobic gram negative bacilli may be present as well.7 The most commonly isolated organisms are from the Streptococcus milleri family, but the type of organism isolated has not been associated with the severity of disease or the outcome.3,6,8A preceding course of oral antibiotics may make isolating the offending pathogen difficult, and blood cultures are rarely positive for the infecting bacterium.8 As the use of antibiotics has become more prevalent over the past few decades, the incidence of sinogenic brain abscess has decreased.9 Subdural empyemas present most commonly in the second and third decades of life.3 While they can have a wide variety of symptoms, fever and progressive headache are the most common.2 Some patients do not have a known history of sinus disease, and others may have chronic or subacute sinusitis which can confound the clinical diagnosis further. 3,5,6,8 Germiller et al6 reported a mean symptom duration of 12 days prior to diagnosis, and Farah and colleagues10 found symptoms took 2–6 weeks to develop from sinusitis to signs of intracranial infection. This subacute course and vague symptoms contribute to the risk of misdiagnosis or delay in diagnosis.10 Altered mental status, seizures, and hemiparesis are the most common neurologic manifestations, but focal neurologic deficits may be present as well, particularly if there is an associated intracranial abscess. Interestingly, intracranial abscesses occur concomitantly in 6–22% of cases.3 Neurologic findings are particularly ominous and vary depending on the location of the lesion, but when they are present, rapid neurosurgical intervention is necessary because these symptoms will worsen rapidly.3 Other nonspecific symptoms include nausea, vomiting, meningismus, personality changes, papilledema, periorbital edema, and cranial nerve palsies.5 Because many of these patients may present with vague symptoms, if there are extracranial symptoms, such as facial swelling, periorbital edema, or proptosis, or ocular findings such as vision loss, decreased or painful extra-ocular motion, and diplopia, further testing is recommended because extracranial symptoms may be a harbinger of an intracranial infectious process.5 Singh et al11 found that 37% of patients with subdural empyemas had concomitant extracranial complications. Finding these extracranial complications before neurologic symptoms have developed will improve the likelihood of an uncomplicated outcome.6,8
In this era of frequent CT use, early diagnosis is much more likely to occur than previously, and this has likely contributed to the decreased mortality and long-term morbidity of suppurative intracranial infections. Imaging studies should be performed immediately if there is concern for intracranial extension. CT is typically the first-line choice because it is readily available and may show edema or mass effect. CT should be done with intravenous contrast if there is concern for an intracranial infection. If it is negative, and a subdural empyema is still considered, an MRI must be obtained with gadolinium contrast. MRI is the most sensitive test for intraparenchymal and intracranial infections and is considered the gold standard.5,7 One recent study found CT to have a 63% sensitivity for sinogenic intracranial complications while MRI was 93% sensitive.6 Management of subdural empyemas includes immediate administration of a third generation cephalosporin plus metronidazole and vancomycin to provide appropriate coverage against streptococci species and Staphylococcus aureus.5,7Adjunctive seizure prophylaxis is recommended early as well, as seizures may be present in up to 20% of cases. 3,8,12 Interventions to lower intracranial pressure (elevation of the head of the bed, mannitol, and ventriculostomy) should be performed as necessary. Emergent neurosurgical consultation is paramount as surgical intervention (burr hole or craniotomy) is necessary in most cases to provide the best opportunity at neurologic recovery.2 Likewise, otolaryngologic consultation is recommended because functional endoscopic sinus surgery (FESS) may aid in drainage and recovery.5,8 Historically, mortality from subdural empyema has been as high as 15– 41% even with surgical drainage.3,10,13 Antimicrobials have significantly lowered the mortality rate, as subdural empyema was universally fatal prior to antibiotic use.3 The advent of CT and MRI has also helped to decrease the mortality rate, with recent studies suggesting a mortality rate between 6% and 15%.3,14–17 Germiller and colleagues6 reported a 4% mortality rate in a pediatric series of intracranial suppurative infections. Survivors often have significant morbidity with 12–37.5% having persistent seizures, hemiparesis in 15–35%, or residual neurologic deficits in up to 50% of survivors.3,14–16
CONCLUSION
Intracranial suppurative complications, such as subdural empyemas, are rare and difficult to diagnose because initial symptoms may be vague. Patients with sinus infections and progressive headaches or any neurological deficits should be aggressively evaluated with CT or MRI imaging as needed to rule out intracranial spread. Because subdural empyemas have serious morbidity and mortality if not recognized and treated promptly, emergency physicians must be aware of the risks of subdural empyema and the need to emergency neurosurgical intervention.
Footnotes
Supervising Section Editor: Rick A. McPheeters, DO
Submission history: Submitted January 1, 2012; Revision received April 17, 2012; Accepted May 14, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.5.11727
Address for Correspondence: David Bruner, MD, Department of Emergency Medicine, Naval Medical Center Portsmouth, 620 John Paul Jones Circle, Portsmouth, VA 23708
E-mail: dibruner@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors diclosed none. The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense or the United States Government.
REFERENCES
1. Adame N, Hedlund G, Byington CL. Sinogenic intracranial empyema in children.Pediatrics. 2005;116:e461–7. [PubMed]
2. Waseem M, Khan S, Bomann S. Subdural Empyema Complicating Sinusitis. J Emerg Med. 2008;35(3):277–81. [PubMed]
3. Osborn MK, Steinberg JP. Subdural Empyema and Other Suppurative Complications of Paranasal Sinuses. The Lancet Infectious Disease. 2007;7(1):62–7.
4. Bradley PJ, Manning KP, Shaw HD. Brain abscesses secondary to paranasal sinusitis. J Laryngol Otol. 1984;98:719–25. [PubMed]
5. Kombogiorgas D, Seth R, Athwal R, et al. Suppurative intracranial complications of sinusitis in adolescence. Single institute experience and review of literature. Brit J Neurosurg. 2007;21(6):603–9. [PubMed]
6. Germiller JA, Sparano AM. Intracranial complications of sinusitis in children and adolescents and their outcomes. Arch Otolaryngol Head Neck Surg. 2006;132:969–76.[PubMed]
7. Greenlee JE. Subdural empyema. Curr Treat Options Neurol. 2003 Jan;5(1):13–22.[PubMed]
8. Hicks CW, Weber JG, Reid JR, et al. Identifying and managing intracranial complications of sinusitis in children: A retrospective series. Pediatr Infect Dis J.2011;30:222–6. [PubMed]
9. Goodkin HP, Harper MB, Pomeroy SL. Intracerebral abscess in children: historical trends at Children’s Hospital Boston. Pediatrics. 2004;113:1765–70. [PubMed]
10. Farah JO, Kandasamy J, May P, et al. Subdural empyema secondary to sinus infection in children. Childs Nerv Syst. 2009;25:199–205. [PubMed]
11. Singh B, Van Dellen J, Ramjettan S, et al. Sinogenic intracranial complications. J Laryngol Otol. 1995;109:945–50. [PubMed]
12. Clayman GL, Adams GL, Paugh Intracranial complications of paranasal sinusitis: a combined institutional review. Laryngoscope. 1991;101:234–9. [PubMed]
13. Quarashi H, Zevallos JP. Subdural empyema as a complication of sinusitis in the pediatric population. Int J Pediatr Otorhinolaryngol. 2006;70:1581–6. [PubMed]
14. Dill SR, Cobbs CG, McDonald CK. Subdural empyema: analysis of 32 cases and review.Clin Infect Dis. 1995;20:372–86. [PubMed]
15. Hoyt DJ, Fisher SR. Otolaryngologic management of patients with subdural empyema. Laryngoscope. 1991;101:20–4. [PubMed]
16. Nathoo N, Nadvi SS, van Dellen JR, et al. Intracranial subdural empyemas in the era of computed tomography: a review of 699 cases. Neurosurgery. 1999:529–35. [PubMed]
17. Bok AP, Peter JC. Subdural empyema: burr holes or craniotomy? A retrospective computerized tomography-era analysis of treatment in 90 cases. J Neurosurg.1993;78:574–8. [PubMed]