| Author | Affiliation |
|---|---|
| Federico E. Vaca, MD, MPH | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| Diane Winn, RN, MPH | Department of Emergency Medicine, University of California, Irvine School of Medicine |
ABSTRACT
Nearly eight million emergency department (ED) visits are attributed to alcohol every year in the United States. A substantial proportion is due to trauma. In 2005, 16,885 people were killed as a result of alcohol-related motor vehicle crashes. Patients with alcohol-use problems (AUPs) are not only more likely to drive after drinking but are also at greater risk for serious alcohol-related illness and injury. Emergency departments have an important and unique opportunity to identify these patients and intervene during the “teachable moment” of an ED visit. The American College of Emergency Physicians, Emergency Nurses Association, American College of Surgeons-Committee on Trauma, American Public Health Association, and the National Highway Traffic Safety Administration, have identified Alcohol Screening, Brief Intervention and Referral to Treatment (SBIRT) as a pivotal injury- and illness-prevention strategy to improve the health and well-being of ED patients. We provide a general overview of the basis and need for integrating SBIRT into EDs. Models of SBIRT, as well as benefits and challenges to its implementation, are also discussed.
INTRODUCTION
In the United States (U.S.), someone is injured in an alcohol-related motor vehicle crash every two minutes, and every 31 minutes an alcohol-related crash fatality occurs.1 In 2005, these crash fatalities accounted for 39% of the 43,443 national traffic deaths.1Between 1992 and 2000, U.S. emergency departments had more than 860 million visits. Emergency Department (ED) visits attributable to alcohol during the same period averaged nearly 8 million annually with an 18 % rise over nine years.2 Alcohol intoxication remains a leading risk factor for injury.3–5 Similarly, alcohol is implicated as an independent risk factor in a multitude of medical and psychiatric conditions (e.g. cancer, community-acquired pneumonia, cardiomyopathy, gastrointestinal, liver disease, pancreatitis, anxiety disorder, depression, schizophrenia)6–10. More recent studies have implicated alcohol in other life-threatening events, such as intracerebral hemorrhage in younger adults.11
Alcohol’s impact on the public’s health is detrimental, and there is considerable need to mitigate alcohol-related illness and injury. Applying the public health model to the readily identified burden results in preventive measures such as Alcohol Screening, Brief Intervention and Referral to Treatment (SBIRT).
Although organized pre-hospital care and regionalization of trauma centers have saved tens of thousands of lives over the past 30 years, further progress through injury prevention will save the greatest number of lives in the shortest period of time.12, 13 SBIRT is one important prevention strategy that has great potential to make a significant impact in the health and well-being of ED patients.
What Is SBIRT?
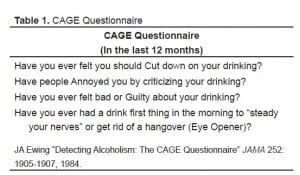
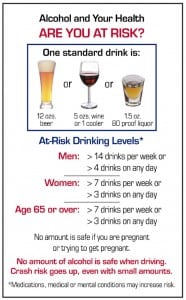
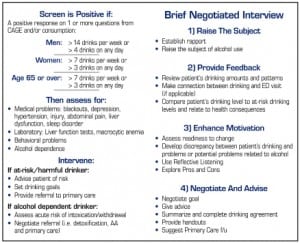
In the last decade, SBIRT in EDs has gained significant momentum and acceptance. SBIRT allows medical and nursing professionals or specially trained personnel to quickly and effectively survey patients regarding their alcohol-use habits (quantity and frequency) and categorize them as a non-drinker, drinker not at risk, drinker at risk or alcohol dependent. Survey tools commonly used in SBIRT have been validated in multiple settings worldwide. These questionnaires gather information about a patient’s drinking frequency, habits and experiences. Today, the two survey tools most commonly used in the ED are the CAGE questionnaire and the Alcohol Use Identification Test (AUDIT) (Table 1 and Figure 1).
The CAGE questionnaire (four questions) is the simpler of the two survey tools. However, the limited focus of CAGE identifies only alcohol-dependent subjects who likely need intervention beyond the scope of what can be provided during an ED visit. In contrast, the AUDIT is a 10-question survey used by the World Health Organization that identifies a subject “at risk” for harmful and hazardous events. The AUDIT surveys three key domains (hazardous use, dependence symptoms, and harmful use), which yield a more complete profile of a person with an alcohol-use disorder. More importantly, AUDIT identifies the individuals “at risk” for alcohol-use problems who may benefit the most from SBIRT.
Identification of “at risk” drinkers is only one part of the SBIRT method. The intervention component of SBIRT is accomplished through a motivational interviewing technique better known as the brief negotiated interview (BNI). Utilizing the BNI, introspective discussion and questioning of a patient leads to an eventual assessment of their willingness to modify their alcohol consumption toward healthier limits (Figure 2 and and3).3). Finally, upon completion of the BNI, the patient’s new alcohol-use reduction goals and outpatient treatment and follow-up plans are reviewed.
Why SBIRT in the ED?
Emergency departments remain the healthcare safety net for the nation. By default, millions of individuals seek “primary care” in the ED. SBIRT has the potential to reach this vulnerable yet neglected population to identify drinking patterns and habits that put them at significant risk for alcohol-related illness and serious injury. Further, studies repeatedly find that a substantial proportion of ED patients have significant underlying alcohol problems.14–16 As a result, millions more will be caught in the cycle of recidivism for alcohol-related disease and trauma.17, 18
According to the American College of Surgeons Committee on Trauma (ACS-COT), as of 2006 all Level I and Level II trauma centers must be SBIRT-capable and integrate it into their trauma service repertoire. Without this service, trauma centers place their verification status in jeopardy. While the ACS-COT makes the requirement for SBIRT clear for Level I and II trauma centers in its publication, Resources for Optimal Care of the Injured Patient: 2006, it also recommends that all trauma centers utilize SBIRT as part of routine trauma care.19 The ACS-COT, in collaboration with the Center for Disease Control and Prevention, National Highway Traffic Safety Administration, and the Substance Abuse and Mental Health Service Administration, is holding national SBIRT training sessions for trauma care providers throughout the United States for the 2007 year.20Finally, and most importantly, studies show that patients are amenable to participating in SBIRT21 and that SBIRT is efficacious in patients with alcohol-use problems.12, 22–29 In a review conducted by D’Onofrio and Degutis, positive effects of SBIRT were found in 32 of 39 clinical studies.24 SBIRT studies in EDs and trauma centers have reported reduction in alcohol consumption and repeat-injury hospitalizations as well as decreased drinking and driving.12, 14, 23, 26, 30
Models of SBIRT Administration
The most common models used to administer SBRIT to ED patients are emergency physician (EP)/nurse- directed SBIRT or administration through the use of specially trained health promotion/education paraprofessionals. These models are not without their limitations.
In busier EDs, it may be infeasible to have only emergency physicians or nurses administer SBIRT. While time constraints in some ED settings are challenging, this should not completely preclude the integration of SBIRT into the ED. If resources allow, specially trained paraprofessionals can administer SBIRT. The added value of these personnel can positively impact both customer satisfaction as well as health promotion activities.31Another method for SBIRT administration in a busy ED setting is that of using computer technology and human-computer interaction to accomplish SBIRT tasks and goals. The use of computers in the ED for SBIRT and other health promotion activities has been feasible and holds considerable promise.32–34 While several variations in the method of computer use for SBIRT do exist, they all focus on minimizing the physician time to administer SBIRT; they also facilitate standardization and fidelity of SBIRT delivery. Further, through relatively simple computer programming and the use of software, computers offer greater facilitation of multi-lingual administration with little added additional effort or cost.
In our institution we have been successful in integrating a bilingual (English and Spanish) “roll-to-the-bedside” Computerized Alcohol Screening and Intervention (CASI) kiosk prototype. We have found the average patient screening time with CASI to be less than five minutes. This kiosk is fully interactive through an audio and graphical interface. Through a touch-screen monitor and head phones, CASI engages the patient in conversation, administers the AUDIT questionnaire, undertakes a brief negotiated interview, and prints a personal alcohol-reduction plan with referral to treatment information. While the integration of a human-computer interaction model for SBIRT administration is feasible, more rigorous studies using computerized SBIRT are needed to more completely assess its efficacy. Such efforts continue to be encouraged by federal research funding agencies.35
Challenges to SBIRT Integration
The availability of time to administer SBIRT in the ED is arguably the most significant challenge. However, innovative approaches to SBIRT delivery have helped to overcome this barrier in some EDs. Further, it should be noted that the majority of ED patients who will encounter SBIRT will either be non-drinkers or drinkers found not to be at risk. This essentially removes 70–75% of those screened from the brief negotiated interview. For subjects identified by SBIRT as “at risk drinkers” who undergo both the screening and brief negotiated interview, the aggregate time remains an average of 10 minutes. Further, with computerized SBIRT the screening and brief intervention delivery is routinely less than 10 minutes for the “at risk” drinker. While for some the time expense to SBIRT may still be considered too much of a “cost,” one only need compare the amount of time and vigor spent to screen patients for tetanus even though the average number of new tetanus cases per year in the U.S. is only 43.36 Contrast that to the number of annual alcohol-related crash fatalities of nearly 17,000, with nearly 8 million alcohol-attributable ED visits every year.
Another challenge to SBIRT in the ED is the comfort level at which EPs and nurses can administer SBIRT to patients. Some training and learning must take place before the person-to-person SBIRT interaction becomes efficient and routine. Even though most acute care providers may be comfortable asking a patient if they drink alcohol, a more in-depth discussion about alcohol-use patterns takes practice, particularly as the healthcare professional conducts the brief negotiated interview and motivates the patient to consider healthier and safer alcohol use. In general, the skills to become effective in delivering SBIRT in the ED are relatively easy to acquire. Some helpful online resources can be found on internet web pages hosted by the American College of Emergency Physicians (http://www.acep.org/webportal/PracticeResources/issues/pubhlth/alcscreen), the Substance Abuse and Mental Health Administration (http://sbirt.samhsa.gov/ andhttp://sbirt.samhsa.gov/documents/SBIRT_guide_Sep07.pdf) and the National Institute for Alcohol Abuse and Alcoholism (http://www.niaaa.nih.gov/Publications/EducationTrainingMaterials/guide.htm). While physicians and nurses can become proficient at administering SBIRT, it should be noted that the available resources and services for in-patient and long-term treatment for dependent drinkers remain under-funded and limited in most communities.
A final challenge to consider comes from a policy perspective in the form of The Uniform Accident and Sickness Policy Provision Law, or UPPL. In 1950, the National Association of Insurance Commissioners developed the provision that allows insurance carriers to exclude coverage to patients for alcohol- and drug-related injuries. As a result, physicians and hospital staff have the false perception that reimbursement for their services will universally be denied. This perception is counterproductive to helping patients who might otherwise benefit from SBIRT. There continues to be growing legislative activity throughout the nation with recent repeals of UPPL in some states. Furthermore, studies show significant legislative support for wider repeal of UPPLs nationwide.37, 38
Promising Facilitators of SBIRT
Several recent developments have begun to further facilitate and support ED SBIRT efforts. In addition to the ACS-COT mandate, according to George Washington University Medical Center’s research group, Ensuring Solutions to Alcohol Problems, the 2007 federal legislative year may be the busiest yet in repealing UPPL or Alcohol Exclusion Laws. Moreover, as of January 2007, current procedural terminology codes (CPT) have been approved to allow the U.S. Center for Medicare and Medicaid Services to reimburse for alcohol and drug screening and brief intervention.38 While there are many more details to work out in billing and reimbursement for SBIRT, there is potential for a regular revenue stream to counter the argument that ED personnel are too busy to perform this critical public health intervention.
CONCLUSION
Although the initial “cost” of implementing SBIRT in the ED may appear to be an additional burden, the savings are great and include less recidivism and avoidance of alcohol-related medical illness, injury and fatality. Alcohol SBIRT offers advantages to patient care, patient well-being and the public’s health.
Footnotes
Submission history: Submitted May 8, 2007; Accepted June 25, 2007
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Federico Vaca, MD, MPH, University of California, Irvine Medical Center, Center for Trauma and Injury Prevention Research 101 The City Drive, Route 128-01 Orange, CA, 92868
Email: fevaca@uci.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. National Highway Traffic Safety Administration. Traffic Safety Facts 2005: Alcohol.Washington DC: US Department of Transportation; 2006. DOT HS 810 616.
2. McDonald AJ, 3rd, Wang N, Camargo CA., Jr US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Arch Intern Med.2004;164:531–537. [PubMed]
3. Soderstrom CA, Dischinger PC, Smith GS, McDuff DR, Hebel JR, Gorelick DA. Psychoactive substance dependence among trauma center patients. JAMA.1992;267:2756–2759. [PubMed]
4. Rivara FP, Jurkovich GJ, Gurney JG, et al. The magnitude of acute and chronic alcohol abuse in trauma patients. Arch Surg. 1993;128:907–912. [PubMed]
5. Soderstrom CA, Dischinger PC, Smith GS, et al. Alcoholism at the time of injury among trauma center patients: vehicular crash victims compared with other patients. Accid Anal Prev. 1997;29:715–721. [PubMed]
6. Lieber CS. Medical disorders of alcoholism. N Engl J Med. 1995;333:1058–1065.[PubMed]
7. De Roux A, Cavalcanti M, Marcos MA, et al. Impact of alcohol abuse in the etiology and severity of community-acquired pneumonia. Chest. 2006;129:1219–1225. [PubMed]
8. Rehm J, Gmel G, Sempos CT, Trevisan M. Alcohol-related morbidity and mortality.Alcohol Res Health. 2003;27:39–51. [PubMed]
9. Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98:1209–1228. [PubMed]
10. Cargiulo T. Understanding the health impact of alcohol dependence. Am J Health Syst Pharm. 2007;64:S5–S11. [PubMed]
11. Feldmann E, Broderick JP, Kernan WN, et al. Major risk factors for intracerebral hemorrhage in the young are modifiable. Stroke. 2005;36:1881–1885. [PubMed]
12. Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230:473–480.[PMC free article] [PubMed]
13. Maier RV. Controlling alcohol problems among hospitalized trauma patients. J Trauma. 2005;59:S1–S2. [PubMed]
14. Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med. 1997;30:181–189. [PubMed]
15. Cherpitel CJ. Emergency room and primary care services utilization and associated alcohol and drug use in the United States general population. Alcohol. 1999;34:581–589.
16. D’Onofrio G, Becker B, Woolard RH. The impact of alcohol, tobacco, and other drug use and abuse in the emergency department. Emerg Med Clin North Am. 2006;24:925–967.[PubMed]
17. Lowenstein SR, Weissberg MP, Terry D. Alcohol intoxication, injuries, and dangerous behaviors–and the revolving emergency department door. J Trauma. 1990;30:1252–1258. [PubMed]
18. Rivara FP, Koepsell TD, Jurkovich GJ, Gurney JG, Soderberg R. The effects of alcohol abuse on readmission for trauma. JAMA. 1993;270:1962–1964. [PubMed]
19. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Service Administration, Center for Substance Abuse Treatment. Alcohol Screening and Brief Intervention (SBI) for Trauma Patients: Committee on Trauma Quick Guide; Washington, DC. 2007. (SMA) 07–4266.
20. American College of Surgeons – Committee on Trauma. Screening and Brief Intervention Training for Trauma Care Providers [electronic] [Accessed April 10, 2007]. Available at: http://www.mayatech.com/cti/sbitrain07.
21. Hungerford DW, Pollock DA, Todd KH. Acceptability of emergency department-based screening and brief intervention for alcohol problems. Acad Emerg Med. 2000;7:1383–1392. [PubMed]
22. Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review.Addiction. 1993;88:315–335. [PubMed]
23. Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med.1997;12:274–283. [PMC free article] [PubMed]
24. D’Onofrio G, Degutis LC. Preventive care in the emergency department: screening and brief intervention for alcohol problems in the emergency department: a systematic review. Acad Emerg Med. 2002;9:627–638. [PubMed]
25. Longabaugh R, Woolard RE, Nirenberg TD, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001;62:806–816. [PubMed]
26. Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67:989–994. [PubMed]
27. Crawford MJ, Patton R, Touquet R, et al. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomised controlled trial. The Lancet. 2004;364:1334–1339.
28. Hungerford DW, Pollock DA. Alcohol interventions in emergency medicine: referral makes a difference. The Lancet. 2004;364:1289–1290.
29. D’Onofrio G, Degutis LC. Screening and Brief Intervention in the Emergency Department. Alcohol Res Health. 2004/2005;28:63–72.
30. Dinh-Zarr T, DiGuiseppi C, Heitman E, Roberts I. Interventions for preventing injuries in problem drinkers. Cochrane Database Syst Rev. 2000;(2):CD001857. [PubMed]
31. Sise MJ, Sise CB, Kelley DM, Simmons CW, Kelso DJ. Implementing screening, brief intervention, and referral for alcohol and drug use: the trauma service perspective. J Trauma. 2005;59:S112–133. [PubMed]
32. Maio RF, Shope JT, Blow FC, et al. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emerg Med. 2005;45:420–429. [PubMed]
33. Neumann T, Neuner B, Weiss-Gerlach E, et al. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. J Trauma. 2006 Oct;61(4):805–814. [PubMed]
34. Blow FC, Barry KL, Walton MA, et al. The efficacy of two brief intervention strategies among injured, at-risk drinkers in the emergency department: impact of tailored messaging and brief advice. J Stud Alcohol. 2006 Jul;67(4):568–578. [PubMed]
35. Hungerford DW, Pollock DA. Emergency department services for patients with alcohol problems: research directions. Acad Emerg Med. 2003 Jan;10(1):79–84. [PubMed]
36. Pascual FB, McGinley EL, Zanardi LR, Cortese MM, Murphy TV. Tetanus surveillance–United States, 1998–2000. MMWR Surveill Summ. 2003 Jun 20;52(3):1–8. [PubMed]
37. Gentilello LM, Donato A, Nolan S, et al. Effect of the Uniform Accident and Sickness Policy Provision Law on alcohol screening and intervention in trauma centers. J Trauma.2005;59:624–631. [PubMed]
38. Ensuring Solutions to Alcohol Problems. Detailed Information About Coding for SBI Reimbursement [Electronic] [Accessed April 12, 2005]. Available at:http://www.ensuringsolutions.org/moreresources/moreresources_show.htm?doc_id=385559.