| Author | Affiliation |
|---|---|
| Lisa Reedman, MD | Morristown Memorial Hospital |
| Richard D. Shih, MD | Morristown Memorial Hospital New Jersey Medical School |
| Oliver Hung, MD | Morristown Memorial Hospital |
ABSTRACT
Abrus precatorius seeds contain one of the most potent toxins known to man. However, because of the seed’s outer hard coat the vast majority of ingestions cause only mild symptoms and typically results in complete recovery. If the seeds are crushed and then ingested, more serious toxicity, including death, can occur.
We present a case of a man who survived an intentional ingestion of crushed Abrus seeds after he was treated with aggressive gastric decontamination and supportive care.
INTRODUCTION
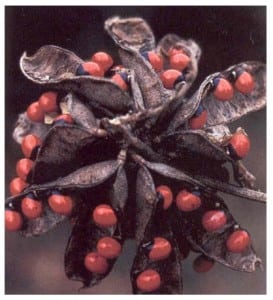
Abrus precatorius is a vine native to India and other tropical and subtropical areas of the world. Since introduction to Florida and the Caribbean, it is now commonly found throughout these areas and in the southern United States.1 It is known by a variety of names, including jequirty bean, rosary pea, prayer bead, crab’s eye, and love bean.2 The vine has pods with oval seeds and a hard glossy shell. The seeds vary in color, from red, black, orange or white with black and white centers (Figure 1). While all parts of the plant are toxic, the highest concentrations are found in the seeds.1 Due to their appearance, the seeds are often used for jewelry, beadwork and ornaments.3
Abrus contains a potent toxin, abrin, along with smaller concentrations of glycyrrhizin, aric acid, and N-methyltryptophal. Abrin is a toxalbumin, composed of two subunits, an A and B chain covalently linked through a disulfide bridge. The toxin’s structure is similar to insulin, ricin, botulinum, cholera and diphtheria toxins.1 The B chain facilitates binding to cell surface receptors, allowing the entry of the A chain into cells.4The A chain acts on the 60s ribosome to inhibit EF-1 and EF-2, preventing protein synthesis and leading to cell death.1,5
Oral ingestion of whole seeds often does not produce serious illness since the shell protects the toxin from digestion.7 Poisonings are more likely in the fall because new crops with immature seeds have a softer shell.6 Conversely, older seeds have brittle shells and also a greater potential for toxin exposure to the gastrointestinal tract. Chewing, grinding, or drilling the seed disrupts the hard shell, exposing more abrin to the GI tract. Most effects of this toxin are limited to local GI symptoms, as digestive enzymes destroy the toxin and limit systemic absorption.
The majority of cases involving abrin are ingestions with whole seeds. These cases often cause few or mild symptoms because the shell remains intact and there is limited toxin exposure. Only one previous case documents the intentional ingestion of Abrus seeds that have been ground or crushed. Our case also involves a suicide attempt involving ingestion of ground Abrus seeds. However, unlike the previous case that led to death, in this case with aggressive GI decontamination and supportive care, the patient survived with no sequelae.
CASE REPORT
A 27-year-old man presented to the emergency department (ED) with multiple episodes of vomiting and liquid black stools. The patient revealed that he had intentionally ingested the powder of 10 ground Abrus precatorius seeds in a suicide attempt approximately 30 minutes prior to ED arrival. The patient had ground up the seeds and mixed the powder with water to make a liquid slurry. After he ingested this liquid slurry, he decided that he did not want to go through with the suicide and self-administered 50 grams of activated charcoal orally just prior to presenting to the ED. Upon arrival, he was awake, alert, and oriented, and initial vital signs revealed a blood pressure of 140/100 mmHg, pulse of 130 beats/minute, respiratory rate of 12 breaths/minute, and a temperature of 99.4°F. Cardiac monitoring showed sinus tachycardia without ectopy or arrhythmias. On physical examination his head, neck, heart, lung, and neurological exams were normal. Abdominal exam revealed normal bowel sounds with diffuse mild tenderness to palpation. Rectal examination revealed black colored stools that were hemocult negative.
Intravenous fluid boluses and anti-emetics were administered. Despite the history of self-administered charcoal, activated charcoal (50 grams) were administered orally in the ED. Laboratory tests revealed: sodium of 143 mEq/L, potassium of 4.0 mEq/L, chloride of 100mEq/L, carbon dioxide of 26mEq/L, urea nitrogen of 16 mEq/L, creatinine of 1.0mg/dL and glucose of 98 mg/dL. Liver function tests and CBC were normal. Salicylate, acetaminophen, and ethanol levels were within normal limits, and urine drug screen was negative.
Upon re-evaluation, the patient continued to have diarrhea but had stopped vomiting. His tachycardia and abdominal tenderness also resolved during his ED evaluation. The patient was medically cleared after ~ 8 hours in the ED for psychiatric evaluation. One month follow-up phone call revealed no further sequelae from his ingestion.
DISCUSSION
Abrus precatourius is one of the most potent plant toxins known to man.6 The toxin, a protein, is poorly absorbed in the digestive tract and rarely, if ever, causes systemic toxicity via the oral ingestion. However, if injected parentally, it can enter the systemic circulation, where it has potent effects on protein synthesis, and even in small amounts can lead to fatalities.
The majority of poisonings involve children who ingest seeds, either from broken pieces of jewelry or off the native plant.10 Despite this, ingesting whole seeds produces few or mild symptoms because the shell insulates the toxin from absorption, and digestive enzymes in the gastrointestinal tract destroy the toxin. However, if the shell has been broken through chewing, drilling or grinding, increased amounts of the toxin are exposed to the digestive system. Although poorly absorbed, the toxin can produce local GI symptoms with large exposures, such as in our case above.
Typical GI symptoms include nausea, vomiting, and diarrhea, resulting in more serious poisonings with severe dehydration and death.1 Clotting time and platelet function appear to be unaffected by the toxin, although non-toxic agglutins are present in the seeds.4 There is no known toxicity level in humans, although there is a steep dose-lethality curve in animals.2 In addition, animals given lethal doses of abrin did not show unusual or unique symptoms when compared to animals given non-lethal doses.9Symptoms can sometimes be delayed for 1–3 days after ingestion, and the clinical course can last up to 10 days.2,6
Due to the delay between ingestion and symptoms, immediate and aggressive treatment may be necessary. Gastric emptying techniques, including induced emesis, activated charcoal, gastric lavage and whole bowel irrigation, may be useful treatment modalities.6 There is no specific antidote for abrin poisoning, and treatment is mainly supportive with intravenous fluids and correction of electrolyte abnormalities.2 In addition, stool and vomitus should not be discarded until the diagnosis is confirmed, as seed remnants may be present within these specimens.6
While poisonings with abrin are potentially life threatening, the majority of cases result in only mild symptoms. These patients require supportive care during the acute phase, and most recover without permanent sequelae. One case reported a four-year-old child who ingested four old and dry seeds. He was treated with induced emesis, activated charcoal, and cathartics. He fully recovered over three days and was discharged home without any sequalae. This case is typical of most abrin exposures, in that it involves ingestion of a few seeds resulting in mild GI symptoms and full recovery.10
Although severe sequelae can occur from oral ingestion of Abrus seeds, it is felt that the seed coating is protective and limits toxicity. Few cases involve the crushing or pulverizing of Abrus seeds, as in the case presented here. There is only one previously published similar case. This involves a 25-year-old male who put 20 Abrus seeds and graphite into a blender, and then drank most of this mixture in a suicide attempt. While he only drank a portion of this mixture, he developed severe nausea, vomiting, and diarrhea. He was brought to the ED four days after the ingestion, later developed cardiac arrhythmias, and died. The mechanism of death in this case is not entirely clear. The crushing of the seeds releases toxin from within the protective outer hard coat of the seeds. This mechanism likely increases the severity of toxicity and decreases the time to onset of symptoms. The classical delay in onset of toxicity associated with the ingestion of intact whole seeds likely does not occur when the seeds have been crushed.
Our case also involves the crushing of the Abrus seeds with oral ingestion in a suicide attempt. Exposure to abrin in this manner most likely increases the toxin exposure in the gastrointestinal tract, as our patient presented with severe vomiting and diarrhea.
However, in our case the patient self-administered activated charcoal prior to ED arrival and received aggressive treatment for dehydration. Outcome in this case was good, in contrast to the previous similar case.
CONCLUSION
The majority of cases of abrin poisoning involve ingestion of a small number of intactAbrus seeds resulting in mild symptoms and full recovery. However, abrin poisoning can be associated with severe GI toxicity, especially when the seeds are pulverized prior to ingestion as in the case presented here. It is believed that early treatment with intravenous fluids and supportive care will lead to good outcome.
Footnotes
Supervising Section Editor: Brandon K. Wills, DO, MS
Submission history: Submitted December 23, 2007; Revision Received March 6, 2008; Accepted March 6, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Richard D. Shih, MD, Morristown Memorial Hospital, 100 Madison Ave, Box #8, Department of Emergency Medicine, Morristown, NJ 07962
Email: Shih100@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Shih RD, Goldfrank LR. Plants. In: Goldfrank LR, Flomenbaum NE, Lewin NA, Weisman RS, Howland MA, Hoffman RS, editors. Goldfrank’s Toxicologic Emergencies. 6. East Norwalk, Connecticut: Appleton and Lange; 1998.
2. Arena JM. Poisoning – toxicology, symptoms and treatments. Springfield, IL: Charles C Thomas; 1986. p. 496.
3. Fernando C. Poisoning due to Abrus precatorius (jequirty bean) Anaesthesia.2001;56:1178–1180. [PubMed]
4. Olsnes S, Refsnes K, Pihl A. Mechanism of action of toxic lectins abrin and ricin. Nature.1974;249:627–631. [PubMed]
5. Benson S, Olsnes S, Pihl A, Skorve J, Abraham AK. On the mechanism of protein-synthesis inhibition by abrin and ricin. Eur J Biochem. 1975;59:573–580. [PubMed]
6. Davies JH. Abrus precatorius (rosary pea). The most common lethal plant poison. J Fla Med Assoc. 1978;65:188–191. [PubMed]
7. Wambebe C, Amosun SL. Some neuromuscular effects of the crude extracts of the leaves of Abrus precatorius. J Ethnopharmacol. 1984;11:49–58. [PubMed]
8. Routh BC, Lahiri SC. Some actions of the seeds of Abrus precatorius. Bulletin of the Calcutta School of Tropical Medicine. 1971;19:46–47. [PubMed]
9. Fodstad O, Johannessen JV, Schjerven L, Pihl A. Toxicity of abrin and ricin in mice and dogs. J Toxicol Envirn Health. 1979;5:1073–1084.
10. Kinamore PA, Jaeger RW, de Castro FJ. Abrus and ricinus ingestion: management of three cases. Clin Toxicol. 1980;17:401–405. [PubMed]
11. Bukhari AQ, Ahmad S, Qureshi S. Oral toxicology of Abrus precatorius linn. J Pak Med Assoc. 1976;26:4–6. [PubMed]
12. Niyogi SK. The toxicology of Abrus precatorius linnaeus. J Forensic Sci. 1970;15:529–536. [PubMed]
13. Olsnes S. Toxic and nontoxic lectins from Abrus precatorius. Methods Enzymol.1978;50:323–330. [PubMed]