| Author | Affiliation |
|---|---|
| Stephanie Stokes-Buzzelli, MD | Henry Ford Health System, Detroit, MI |
| Jennifer M. Peltzer-Jones, RN, PsyD | Henry Ford Health System, Detroit, MI |
| Gerard B. Martin, MD | Henry Ford Health System, Detroit, MI |
| Maureen M. Ford, MD | Henry Ford Health System, Detroit, MI |
| Andrew Weise, MD | Henry Ford Health System, Detroit, MI |
ABSTRACT
Introduction:
To determine if the effective use of Health Information Technologies (HIT) and the Electronic Medical Record (EMR) affects emergency department (ED) usage in a complicated frequently presenting patient population.
Methods:
A retrospective, observational study of 45 patients enrolled in our Frequent User Program called Community Resources for Emergency Department Overuse (CREDO) between June 2005 and July 2007. The study was conducted at an urban hospital with greater than 95,000 annual visits. Patients served as their own historical controls. In this pre-post study, the pre-intervention control period was determined by the number of months the patient had been enrolled in the program. The pre- and post-intervention time periods were the same for each patient but varied between patients. The intervention included using HIT to identify the most frequently presenting patients and creating individualized care plans for those patients. The care plans were made available through the EMR to all healthcare providers. Study variables in this study intervention included ED charges, lab studies ordered, number of ED visits, length of stay (LOS), and Total Emergency Department Contact Time (TEDCT), which is the product of the number of visits and the LOS. We analyzed these variables using paired T-tests. This study was approved by the institutional review board.
Results:
Forty-five patients were enrolled, but nine were excluded for no post enrollment visits; thus, statistical analysis was conducted with n=36. The ED charges decreased by 24% from $64,721 to $49,208 (p=0.049). The number of lab studies ordered decreased by 28% from 1847 to 1328 (p=0.04). The average number of ED visits/patient decreased by 25% from 67.4 to 50.5 (p=0.046). The TEDCT decreased by 39% from 443.7 hours to 270.6 hours (p=0.003).
Conclusion:
In this pre-post analysis of an intervention targeting ED frequent users, the use of HIT and the EMR to identify patients and store easily accessible care plans significantly reduced ED charges, labs ordered, number of ED visits, and the TEDCT.
INTRODUCTION
The effective and efficient management of frequently presenting emergency department (ED) patients is a challenge for many EDs.1–12 This group of patients is among the most complicated as they generally have complex medical and social maladies.1,3–5,7,10,11,13–21 Frequently presenting ED patients have higher incidences of chronic medical conditions, higher overall mortality rates, incur higher healthcare costs, and are admitted more frequently than the overall ED population.5,6,9,11,14,15,21–25 An extreme example is a report of nine frequently presenting ED patients in Texas who accounted for approximately 2700 emergency room visits and $9,000,000 in healthcare charges over a six-year period.26 As ED volumes rise and the national debate on healthcare reform continues, appropriate and efficient care of the frequently presenting ED patient has become a priority.11,21,27–30
Previous care models include intensive case management 1,4,11 and care plan implementation strategies.7,12,19,30,31 These models have demonstrated varying degrees of improved patient care and have varied greatly in terms of staff time and support needed for program success. The effective use of Health Information Technologies (HIT) and Electronic Medical Record (EMR) systems provide EDs new opportunities for more consistent identification and management of frequently presenting patients.32
Our approach to this problem was the development of a multidisciplinary, volunteer group. The Community Resources for Emergency Department Overuse (CREDO) committee consisted of an ED attending physician, ED medical social worker, ED mental health social worker, ED psychologist, ED resident, ED clinical nurse specialists, and a student healthcare volunteer. The CREDO team met twice per month to review current and potential patients to refine and create their care plans. CREDO expanded previous care management models by incorporating HIT into the program. Once created and refined, care plans were uploaded into the EMR, allowing universal 24/7 access and guidance for all healthcare providers treating CREDO patients. CREDO patients were “flagged” in the ED Information System (EDIS) to enable immediate implementation of their care plan.
The American Recovery and Reinvestment Act of 2009 (ARRA) has described expectations for increased HIT use throughout healthcare practice. Additionally, the ARRA has called for “multidisciplinary research on system challenges to healthcare delivery” with emphasis on “the measurement of the impact of HIT on the quality and productivity of healthcare”.33 Previous adaptation of HIT has demonstrated improved healthcare quality and productivity.5, 23, 34–36Frequent ED users present a healthcare delivery challenge, and because of their mixed medical and social problems, require the input of a multidisciplinary team. Although much more money is spent on these patients, the quality of care they receive may not be optimal. Use of HIT for this patient population is not only directly in line with the goals of the ARRA but also may be the only way to effectively manage this population. By using HIT for our CREDO program, we avoided the use of antiquated paper charts. Problems associated with paper charts include a lack of universal access, a potential for lost information, difficulties in updating, poor security of information, and inconsistent recognition that a plan exists for particular patients. HIT can overcome all these problems, as it has a centralized location, multi-user functionality, immediate access, consistent and easy updating, and can be password protected. Additionally, use of HIT allowed consistency in a large volume (>95,000 visits) urban ED setting. The CREDO initiative, similar to other case management models, relied on care plans devised to manage the needs of frequently presenting ED patients. Through the use of HIT and the EMR, this small committee was unique in that it was able to provide quality, cost-effective care on a more consistent basis than previous models. Our project focused on the rapid identification and availability of their care plan in the EMR. This paper describes our experience using this program and provides outcome measures to reflect its efficacy.
METHODS
This study of 45 patients enrolled in the CREDO program between June 2005 and July 2007 was conducted at an urban, inner city hospital ED with greater than 95,000 annual visits. It was approved by the hospital Institutional Review Board. We determined patient selection through a quarterly query of the EDIS, EmSTAT (Allscripts, Chicago, IL). The query noted the 100 patients with the most ED visits. Patients older than 18 years old and with the highest number of visits were considered appropriate for enrollment in CREDO. We excluded frequent users with sickle cell anemia since they were managed in a separate and distinct program.
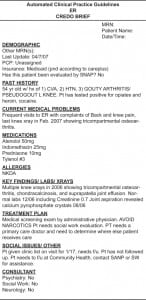
After a patient was selected for the program, a member of the CREDO committee created the CREDO brief. This was a summary of pertinent past medical and social history, including significant laboratory and testing results. It also included individualized specific treatment guidelines as to how to best care for this unique patient. The CREDO brief was then uploaded into the patient’s EMR (CarePlus, HFHS) and made available to all patient care providers. All patients in CREDO were reviewed at least monthly (more frequently if necessary) and their CREDO brief was updated. All CREDO patients were “flagged” in the EDIS to communicate this status to providers in the ED.
The study was a retrospective, observational study of ED use. The intervention was the enrollment in CREDO, which included “flagging” patient in the EDIS and creating a CREDO brief in the EMR. Patients who were enrolled in the program served as their own historical controls.
The pre- and post-intervention time period was the same for each patient but varied between patients. The pre-intervention control period was determined by the number of months the patient had been enrolled in the program as of July 2007. For example, a patient enrolled in January 2007 had six months of CREDO activity. The pre-intervention control time period for this patient included the six months prior to enrollment, i.e. July–December 2006.
Demographic data, as well as key medical and social history, were obtained through retrospective chart review. For each patient the pre- and post-intervention end points analyzed were total ED charges, the number of laboratory studies ordered, average length of stay (LOS), total number of visits, and total emergency department contact time (TEDCT). The TEDCT is the product of the number of visits and the LOS. It represents the total amount of time that each patient was in the ED.
We analyzed pre- and post-intervention data using paired t-tests with a p value of <0.05 considered significant. Ninety-five percent confidence intervals (CI) are reported.
RESULTS
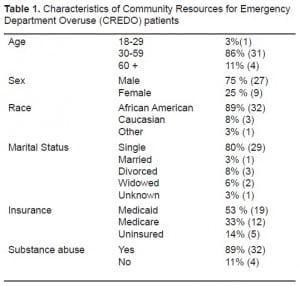
Forty-five patients were enrolled in the CREDO program between June 2006 and July 2007. Nine patients with no post-enrollment visits were excluded from the pre- and post-intervention analysis. The demographic data, as well as key medical and social history, were reported for the 36 patient in the final analysis.
Demographic data is presented for these patients in Table 1. The patients in this study were predominantly male, African-American, and single. Most of the patients (84%) had some type of insurance, with only 16% uninsured. The mean age was 48 years with a range 21 to 71 years. The majority had substance abuse problems (89%). Mental illnesses, including depression, schizophrenia, and/or bipolar disorder, were present in 72%. The patients also had a variety of medical co-morbidities including asthma/COPD (44%), diabetes (25%), seizures (28%), and hypertension (64%).
Length of enrollment in CREDO ranged from three to 23 months with an average of 13.0 ± 7.4 months. The results of the CREDO enrollment on the selected endpoints are depicted in Table 2. Using ED charges (not reimbursement) as an indicator, enrollment in the program decreased the costs associated with these patients. There was a statistically significant reduction of $15,513 in the ED charges per patient before and after enrollment (p=0.049, 95% CI –$30943 to – $83). Also shown in Table 2, the number of laboratory studies ordered on each patient decreased from a mean of 1847/patient to 1328/patient after enrollment in the program (p=0.04, 95% CI −1252 to −26).
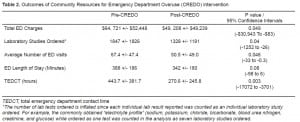
Although the mean LOS prior to enrollment was 388 minutes and decreased by 46 minutes to 342 minutes after enrollment, this decrease did not achieve statistical significance (p=0.08, 95% CI −98 to 6 minutes). The mean number of ED visits/patients decreased from 67.4 to 50.5 after enrollment in the program (p=0.046, 95% CI −33 to −0.3)
The mean TEDCT pre-enrollment was 443.7 hours and decreased 39% to 270.6 hours (p=0.003, 95% CI −17072 to −3701). The mean decrease in TEDCT represents 173.1 hours or a mean of 7.21 days less in the ED.
DISCUSSION
The demographic characteristics, medical histories, and social problems of patients enrolled in this study are similar to those previously reported for frequently presenting patients.1, 5, 11, 14–17, 21We used a multidisciplinary team approach to create individualized care plans that were readily available in an EMR. Previous studies have used a similar approach but most have lacked the benefit of using the EMR and the EDIS to identify, facilitate, and manage these patients. This approach had a positive effect on the use of ED resources. Together these interventions resulted in a 24% reduction in ED charges, a 28% reduction in labs ordered, and a 25% reduction in the number of ED visits by this group of patients. The 12% reduction in ED LOS did not reach statistical significance. Of particular note was the 39% reduction in TEDCT.
TEDCT represents the total amount of contact time that ED providers have with a patient and thus to some extent reflects the efficiency of care. ED overcrowding leads to resource and supply mismatch and has been recognized as having a negative impact on patient care in the ED.17,27,32,37–42 Since all patients in the ED are consuming resources to a variable extent, decreasing the TEDCT increases the amount of resources that can be used for other patients. Frequent users can be demanding and difficult to manage and are disproportionate consumers of ED resources.32 In addition, “flagging” patients at time of registration via the electronic triage system allows the ED staff more consistency in the delivery of care as they can immediately identify these patients as frequent users who have care plans, and then find the care plans in the EMR.12 The easy identification and accessibility of the CREDO brief led to prompt, efficient care of these patients.
Selection bias has been intrinsic to some previously published reports of frequent user programs.1,4,7,11,23 In these studies, patients were “referred” to programs in a less objective and more subjective (physician/RN referral) method. Because our program chose patients solely based on number of visits as indicated by the EDIS, selection bias by ED staff is prevented. This also affords a better understanding of the multiple patient issues of this group, as opposed to focusing on problematic patients thought to be medication seeking, homeless etc. Several patients were referred by ED practitioners for inclusion into the program but were not included because they did not meet criteria. However, the use of the quarterly review of EDIS enabled the rapid identification and creation of care plans for patients who suddenly became eligible for the program.
Patient registries and individualized care plans have been used with success in the care of patients with a variety of medical conditions, including congestive heart failure and diabetes.43,44 The use of such plans as part of the EMR and EDIS in the care of ED frequent users is unique and should be part of the future strategy to manage these patients.
LIMITATIONS AND FURTHER QUESTIONS
A major limitation to our study is the relatively small sample size. While 45 patients were initially enrolled, 20% had no post-enrollment visits. The data presented here are the result of our initial program attempts to combine HIT with managed care plans. The program has continued to expand with over 150 patients currently enrolled.
A second limitation of this study may be related to the natural tendency for ED frequent users to decrease their use over time regardless of intervention.1,5,11,12,15,17,19,28 This may have contributed to our reduction in number of visits. However, recent data from our institution indicates a certain subset of the frequent user population remain frequent users over a ten year period (G. Martin, M.D., personal communication, April 30, 2010). Future investigations may elucidate differences in ED use patterns within the group of frequent users.
A related issue is that definition of a frequent user varies across the literature. 3,5,6,9,14,16,19,21,45While terms such as “super user” and “high frequency user” have been used in the past to describe ED patients, 8 there is no distinct cut-off point to define these categories. Recent studies have used >5 visits / year as criteria for a frequent user, and patients with > 20 visits/yr have been termed “super users” or high frequency users. A consistent approach to the identification of these patients using unbiased objective determinants will aid in their future study and management.
Another limitation is that we collected data only at a single ED, while frequent ED users have a tendency to use multiple EDs within their region.3, 11,15,17,23 The decrease in number of visits to our institution may have led to increased visits to other institutions. A future goal of the CREDO program is to collaborate with neighboring hospitals to study our enrolled patients’ use of other facilities.
The study demonstrated a decrease in ED charges for this group of patients for the study time period. We simply performed a rudimentary cost analysis of total ED charges, not accounting for any changes in supply cost or actual reimbursement. True cost savings cannot be ascertained at this time.
This paper presumes that shorter workups and less repetitive testing of frequent patients are cost effective and thus desirable outcomes. Most would agree with this reasoning. Since we did not follow up with outside institutions, there is a chance that diagnoses were missed due to truncated workups and shortened ED LOS. However, our patients were not only discussed in depth by our multidisciplinary group but also seen multiple times in our ED. As a result, we think the possibility that a significant diagnosis was missed is low.
A final limitation of our study is that the content of the CREDO brief in the EMR served as a treatment recommendation, not a mandate, for providers caring for CREDO patients. While the information was readily available and easily accessible to all providers, we cannot be certain how many providers referenced and followed the briefs’ recommendations when caring for the CREDO patients. Future surveys from care providers regarding the use of the care plans may illuminate the reasons why recommendations were/were not followed.
CONCLUSION
In this pre-post analysis of an intervention targeting ED frequent users, the EMR allowed for easy efficient identification of frequent users and then provided the healthcare team with a pre-designed care plan for them to follow. The combination of HIT with managed care plans significantly reduced total ED charges, total labs ordered, total number of ED visits, and TEDCT for these patients. It did not have a significant change on ED LOS. The impact of our committee creating care plans on provider and patient satisfaction, or frequency of visits to neighboring ED, remains to be determined.
Footnotes
In addition to the authors of this paper, special acknowledgements are given to Christi Pelot MSW, Walter Knysz MD, William Dobson, James Yang PhD, and the entire ED staff who supported this project and helped take care of these patients. Further acknowledgement is given to the McGaw Prize, Department of Philanthropy, Henry Ford Health System, One Ford Place, Detroit, MI 48202 for financial support.
Supervising Section Editor: James P Killeen, MD
Submission history: Submitted January 27, 2010; Revision Received May 10, 2010; Accepted June 22, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Stephanie Stokes-Buzzelli, MD, Henry Ford
E-mail: sbuzzel1@hfhs.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Shumway M, Boccellari A, O’Brien K, et al. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial. Am J Emerg Med. 2008 Feb;26(2):155–64. [PubMed]
2. Milbrett P, Halm M. Characteristics and predictors of frequent utilization of emergency services. J Emerg Nurs. 2009 Jun;35(3):191–8. [PubMed]
3. Wooden MD, Air TM, Schrader GD, et al. Frequent attenders with mental disorders at a general hospital emergency department. Emerg Med Australas. 2009 Jun;21(3):191–5. [PubMed]
4. Pope D, Fernandes CM, Bouthillette F, et al. Frequent users of the emergency department: a program to improve care and reduce visits. Cmaj. 2000 Apr 4;162(7):1017–20. [PMC free article][PubMed]
5. Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department‘s frequent users. Acad Emerg Med. 2000 Jun;7(6):637–46. [PubMed]
6. Ruger JP, Richter CJ, Spitznagel EL, et al. Analysis of costs, length of stay, and utilization of emergency department services by frequent users: implications for health policy. Acad Emerg Med.2004 Dec;11(12):1311–7. [PubMed]
7. Lee KH, Davenport L. Can case management interventions reduce the number of emergency department visits by frequent users? Health Care Manag (Frederick) 2006 Apr–Jun;25(2):155–9.[PubMed]
8. Blank FS, Li H, Henneman PL, et al. A descriptive study of heavy emergency department users at an academic emergency department reveals heavy ED users have better access to care than average users. J Emerg Nurs. 2005 Apr;31(2):139–44. [PubMed]
9. Hunt KA, Weber EJ, Showstack JA, et al. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006 Jul;48(1):1–8. [PubMed]
10. Hackenschmidt A. Should access to emergency departments be limited for “frequent fliers”? J Emerg Nurs. 2003 Oct;29(5):486–8. [PubMed]
11. Okin RL, Boccellari A, Azocar F, et al. The effects of clinical case management on hospital service use among ED frequent users. Am J Emerg Med. 2000 Sep;18(5):603–8. [PubMed]
12. Skinner J, Carter L, Haxton C. Case management of patients who frequently present to a Scottish emergency department. Emerg Med J. 2009 Feb;26(2):103–5. [PubMed]
13. O’Brien GM, Stein MD, Zierler S, et al. Use of the ED as a regular source of care: associated factors beyond lack of health insurance. Ann Emerg Med. 1997 Sep;30(3):286–91. [PubMed]
14. Sandoval E, Smith S, Walter J, et al. A comparison of frequent and infrequent visitors to an urban emergency department. J Emerg Med. 2008 May 5;5:5.
15. Fuda KK, Immekus R. Frequent users of Massachusetts emergency departments: a statewide analysis. Ann Emerg Med. 2006 Jul;48(1):9–16. [PubMed]
16. Byrne M, Murphy AW, Plunkett PK, et al. Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med.2003 Mar;41(3):309–18. [PubMed]
17. Cook LJ, Knight S, Junkins EP, Jr, et al. Repeat patients to the emergency department in a statewide database. Acad Emerg Med. 2004 Mar;11(3):256–63. [PubMed]
18. Olsson M, Hansagi H. Repeated use of the emergency department: qualitative study of the patient’s perspective. Emerg Med J. 2001 Nov;18(6):430–4. [PMC free article] [PubMed]
19. Spillane LLLE, Cobaugh DJ, Wilcox SR, et al. Frequent users of the emergency department: can we intervene? Acad Emerg Med. 1997 Jun;4(6):574–80. [PubMed]
20. Sun BC, Burstin HR, Brennan TA. Predictors and outcomes of frequent emergency department users. Acad Emerg Med. 2003 Apr;10(4):320–8. [PubMed]
21. Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004 Feb;42(2):176–82. [PubMed]
22. Salazar A, Bardes I, Juan A, et al. High mortality rates from medical problems of frequent emergency department users at a university hospital tertiary care centre. Eur J Emerg Med. 2005 Feb;12(1):2–5. [PubMed]
23. Hansagi H, Olsson M, Sjoberg S, et al. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med. 2001 Jun;37(6):561–7.[PubMed]
24. Bernstein SL. Frequent emergency department visitors: the end of inappropriateness. Ann Emerg Med. 2006 Jul;48(1):18–20. [PubMed]
25. Lucas RH, Sanford SM. An analysis of frequent users of emergency care at an urban university hospital. Ann Emerg Med. 1998 Nov;32(5):563–8. [PubMed]
26. 9 patients made nearly 2,700 ER visits in Texas. Associated Press. 2009 Apr 1;
27. Hospital-Based Emergency Care: At the Breaking Point. Institute of Medicine; 2007.
28. Raven MC, Billings JC, Goldfrank LR, et al. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009 Mar;86(2):230–41.[PMC free article] [PubMed]
29. Handel DA, McConnell KJ, Wallace N, et al. How much does emergency department use affect the cost of Medicaid programs? Ann Emerg Med. 2008 May;51(5):614–21. [PubMed]
30. Care plans for frequent flyers save money, cut costs. Hosp Case Manag. 2006 Feb;14(2):22, 30–1.[PubMed]
31. New computer network helps EDs to reduce redundant test orders. ED Manag. 2008 Dec;20(12):133–134. [PubMed]
32. Simon HK, Hirsh DA, Rogers AJ, et al. Pediatric emergency department overcrowding: electronic medical record for identification of frequent, lower acuity visitors. Can we effectively identify patients for enhanced resource utilization? J Emerg Med. 2009 Apr;36(3):311–6. [PubMed]
33. p. 2009. American Recovery and Reinvestment Act of 2009.
34. Bates DW, Kuperman GJ, Rittenberg E, et al. A randomized trial of a computer-based intervention to reduce utilization of redundant laboratory tests. Am J Med. 1999 Feb;106(2):144–50. [PubMed]
35. Khoury A. Finding value in EMRs (electronic medical records) Health Manag Technol. 1997 Jul;18(8):34, 36. [PubMed]
36. Husk G, Waxman DA. Using data from hospital information systems to improve emergency department care. Acad Emerg Med. 2004 Nov;11(11):1237–44. [PubMed]
37. Moskop JC, Sklar DP, Geiderman JM, et al. Emergency department crowding, part 1-concept, causes, and moral consequences. Ann Emerg Med. 2009 May;53(5):605–11. [PubMed]
38. Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000 Jan;35(1):63–8. [PubMed]
39. Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009 Jan;16(1):1–10. [PubMed]
40. Moskop JC, Sklar DP, Geiderman JM, et al. Emergency department crowding, part 2–barriers to reform and strategies to overcome them. Ann Emerg Med. 2009 May;53(5):612–7. [PubMed]
41. Take the lead in helping to remedy ED crowding, diversion, boarding. Hosp Case Manag. 2006 Sep;14(9):129–31. [PubMed]
42. Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008 Aug;52(2):126–36. [PubMed]
43. Toh MP, Leong HS, Lim BK. Development of a diabetes registry to improve quality of care in the National Healthcare Group in Singapore. Ann Acad Med Singapore. 2009 Jun;38(6):546. [PubMed]
44. Shortell SM, Gillies R, Siddique J, et al. Improving chronic illness care: a longitudinal cohort analysis of large physician organizations. Med Care. 2009 Sep;47(9):932–9. [PubMed]
45. Moore L, Deehan A, Seed P, et al. Characteristics of frequent attenders in an emergency department: analysis of 1-year attendance data. Emerg Med J. 2009 Apr;26(4):263–7. [PubMed]


