| Author | Affiliation |
|---|---|
| Richard Bamford, MRCS(Eng) | St George’s Hospital and Medical School, Department of Surgery, London, United Kingdom |
| Gurpreet Singh-Ranger, MS, FRCS(Eng) | William Harvey Hospital, Department of Surgery, Ashford, Kent, United Kingdom |
ABSTRACT
Internuclear ophthalmoplegia is a rare condition caused by injury to the medial longitudinal fasciculus in the brainstem. It usually occurs in conditions such as stroke or multiple sclerosis and is extremely rare after head injury. We report a case of unilateral internuclear ophthalmoplegia, which occurred after a minor head injury in a young male. His only symptoms were headache and diplopia. He was treated conservatively, and his symptoms settled after 3 months.
A 17-year-old male was admitted to our emergency unit after a head injury. He described running, and hitting the front of his head on a lamppost, with brief loss of consciousness.
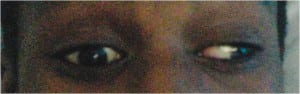
On admission, he had complaints of a generalized headache and double vision, but no other symptoms. On examination, vital signs and Glasgow Coma Scale were normal, but he was unable to adduct his right eye, and had double vision in the neutral position, worse on looking toward the left (Figure 1). Findings from the cranial nerve examination were otherwise normal, and there were no other neurologic deficits or injuries found. An initial computed tomography (CT) result was reported as normal, but a subsequent magnetic resonance imaging (MRI) revealed small bilateral frontal lobe contusions (Figure 2). He was admitted, managed conservatively, and after neurosurgical review, discharged with analgesia and an eye patch. Subsequent review at 3 months showed complete resolution of his diplopia.
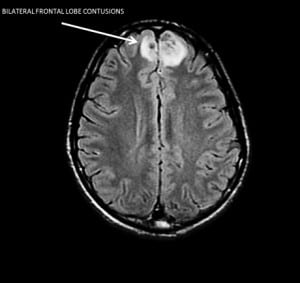
Unilateral internuclear ophthalmoplegia usually occurs in patients with multiple sclerosis or vascular disease1 and is extremely rare after head injury.2 It results from trauma to the medial longitudinal fasciculus (MLF), bundles of nerve fibres in the brainstem, connecting nuclei of the cranial nerves controlling head movement and directional gaze. Injury to the MLF is characterized by inability to adduct 1 eye in lateral gaze, and monocular fast-phase nystagmus of the abducting eye. It is important to note that CT imaging findings are frequently normal, and MRI is the imaging modality of choice.3 Symptoms usually resolve with conservative management after a few months, but sometimes can persist for more than a year.2
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted June 19, 2010; Revision received July 26, 2011; Accepted August 1, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.8.6595
Address for Correspondence: Gurpreet Singh-Ranger, MS
William Harvey Hospital, Department of Surgery, Kennington Rd, Willesborough, Ashford, Kent, United Kingdom, TN24 0LZ
E-mail: gsinghranger@yahoo.co.uk
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. de Andrade DC, Lucato LT, Yamamoto FI, et al. Isolated bilateral internuclear ophthalmoplegia after ischemic stroke. J Neuroophthalmol. 2007;27:125–126. [PubMed]
2. Constantoyannis C, Tzortzidis F, Papadakis N. Internuclear ophthalmoplegia following minor head injury: a case report. Br J Neurosurg. 1998;12:377–379. [PubMed]
3. Obuchowska I, Mariak Z. Internuclear ophthalmoplegia—causes, symptoms and management. Klin Oczna. 2009;111:165–167. [PubMed]


