| Author | Affiliation |
|---|---|
| Rebekah Heckmann, MD | University of Washington, Division of Emergency Medicine, Seattle, Washington |
| Francisco Alexander de la Fuente, MD | University of Washington, Division of Emergency Medicine, Seattle, Washington |
| Jason D. Heiner, MD | University of Washington, Division of Emergency Medicine, Seattle, Washington; PeaceHealth Peace Island Medical Center, Department of Emergency Medicine, Friday Harbor, Washington |
An 11-year-old healthy female presented to the emergency department with three days of worsening suprapubic pain, urinary retention, and constipation. She was afebrile with normal vital signs. Her physical examination was notable for suprapubic distention and bulging pink vaginal tissue at the introitus. Bedside ultrasound suggested a distended bladder. Placement of a Foley catheter returned 550mL of urine with improvement of the patient’s discomfort, but repeat ultrasound visualized a persistent hypoechoic mass adjacent to the newly decompressed bladder (Figure). The obstructive cause of her abdominal pain and urinary retention was revealed by magnetic resonance imaging (MRI) of the pelvis, which confirmed distal vaginal agenesis with uterine distention from hematometrocolpos (Figure). A Foley catheter was temporarily left in place, and after pediatric and gynecological consultation and operative intervention, she was later free of obstructive symptoms after surgical correction of her vaginal agenesis and hematometrocolpos.
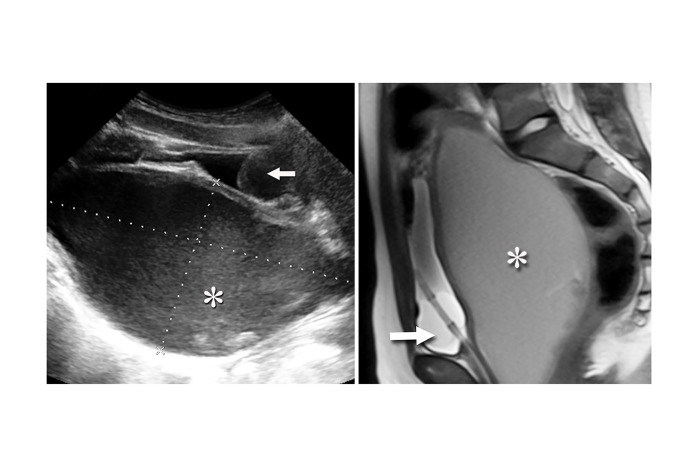
Müllerian duct abnormalities, such as imperforate hymen, transverse vaginal septum, and vaginal agenesis, may be associated with abdominal pain or other symptoms of pelvic outlet obstruction, hematocolpos, and amenorrhea in the early adolescent years.1-4 While the prevalence of congenital uterine anomalies is estimated at 6.7%, Müllerian agenesis with lack of vaginal or uterine development is thought to only occur in one out of every 4,000–10,000 females.1,2 These errors in development are strongly associated with a number of other congenital anomalies including urinary tract abnormalities such as renal agenesis in an estimated 18–40% of patients, particularly when a hymen is absent.3-5 Visualization of vaginal-appearing tissue on physical examination instead of bulging bluish tissue more indicative of an imperforate hymen may suggest vaginal agenesis, but both ultrasound and MRI are recommended to adequately characterize pelvic and neighboring anatomy.6
Footnotes
Section Editor: Sean O. Henderson, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jason Heiner, MD, University of Washington Medical Center, Division of Emergency Medicine, 1959 NE Pacific Street, Box 356123, Seattle, WA 98195. Email: jheiner@uw.edu. 5 / 2015; 16:418 – 419
Submission history: Revision received January 9, 2015; Submitted January 25, 2015; Accepted January 29, 2015
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Saravelos SH, Cocksedge KA, Li T-C. Prevalence and diagnosis of congenital uterine anomalies in women with reproductive failure: a critical appraisal. Hum Reprod Update. 2008;14(5):415-29.
2. Committee on Adolescent Health Care. Committee opinion: no. 562: müllerian agenesis: diagnosis, management, and treatment. Obstet Gynecol. 2013;121(5):1134-7.
3. Li S, Qayyum A, Coakley FV, et al. Association of renal agenesis and mullerian duct anomalies. J Comput Assist Tomogr. 2000;24(6):829-34.
4. Salvatore CA, Lodovicci O. Vaginal agenesis: an analysis of ninety cases. Acta Obstet Gynecol Scand. 1978;57(1):89-94.
5. Kimberley N, Hutson JM, Southwell BR, et al. Vaginal agenesis, the hymen, and associated anomalies. J Pediatr Adolesc Gynecol. 2012;25(1):54-8.
6. Dursun I, Gunduz Z, Kucukaydin M, et al. Distal vaginal atresia resulting in obstructive uropathy accompanied by acute renal failure. Clin Exp Nephrol. 2007;11(3):244-46.


