| Author | Affiliation |
|---|---|
| Rick A. McPheeters, DO | Kern Medical Center, Department of Emergency Medicine, Bakersfield, CA |
| Sommer White, MD | Kern Medical Center, Department of Emergency Medicine, Bakersfield, CA |
| Adria Winter, MD | Kern Medical Center, Department of Emergency Medicine, Bakersfield, CA |
A 31-year-old male presented to the emergency department with a chief complaint of headache after being assaulted with a baseball bat to the head. He denied loss of consciousness, nausea or vomiting. Past medical and surgical history was unremarkable. On physical examination, vitals signs included elevated blood pressure (167/92 mm Hg) and tachycardia (132 bpm). He was somnolent but easily arousable. Head examination revealed abrasions and ecchymosis to the right fronto-temporal scalp and bilateral periorbital ecchymosis (Figure 1). Neurologic examination was nonfocal. There was no hemotympanum or postauricular ecchymosis. Computed tomography (CT) scan of the head revealed a cerebral contusion and subarachnoid hemorrhage. There was an air-fluid level within the left maxillary sinus and a fracture of the left nasal bone; however, a basal skull fracture (BSF) was not radiographically apparent.

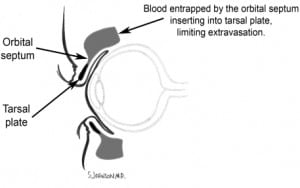
BSF are often missed on CT and plain skull x-rays. Clinical signs are usually more sensitive.1 Signs of BSF may take several hours to develop and include cerebrospinal fluid (CSF), otorrhea or rhinorrhea, hemotympanum, laceration of the external auditory canal, postauricular ecchymosis (Battle’s sign) and periorbital ecchymosis with tarsal plate sparing (Raccoon eyes). Battle’s sign and unilateral blepharohematoma have the highest predictive value.2 Tarsal plate sparing is due to an anatomic structure called the orbital septum, which limits extravasation of blood beyond the tarsal plate (Figure 2). Indirect radiographic findings that suggest BSF include pneumocephalus and air-fluid levels within, or opacification of, an air sinus.
In and of themselves, most BSF’s do not require treatment.1 However, conditions potentially associated with BSF that may require specific management include traumatic aneurysms, posttraumatic carotid-cavernous fistula, cerebrospinal fluid fistula, meningitis, cerebral abscess, cosmetic deformities and posttraumatic facial palsy.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted July 27, 2009; Revision Received July 28, 2009; Accepted August 17, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Rick A. McPheeters, DO, Depart. of Emergency Medicine, Kern Medical Center, 1700 Mt. Vernon Ave., Bakersfield, Ca 93306
Email mcpheetr@kernmedctr.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Mark S. Handbook of Neurosurgery. New York, NY: Thieme; 2006. Greenberg.
2. Pretto FL, De Almeida CS, Casulari LA. Positive predictive values of selected clinical signs associated with skull base fractures. J of Neurosurgical Sciences. 2000;44:77–82.


