| Author | Affiliation |
|---|---|
| Luke Hermann | Mt. Sinai School of Medicine |
| Evelyn Chow | Mt. Sinai School of Medicine |
| W. Lane Duvall | Mt. Sinai School of Medicine |
ABSTRACT
We report a case of iatrogenic claudication as a result of a misplaced percutaneous arterial closure device (PACD) used to obtain hemostasis after cardiac catheterization. The patient presented one week after his procedure with complaints suggestive of right lower extremity claudication. Computed tomographic angiography demonstrated a near total occlusion of the right common femoral artery from a PACD implemented during the cardiac catheterization. The use of PACD’s to obtain rapid hemostasis is estimated to occur in half of all cardiac catheterizations. Ischemic complications as a result of these devices must be considered when evaluating post procedural patients with extremity complaints.
CASE REPORT
A 44 year-old-male with a history of coronary artery disease and recent cardiac catheterization presented to the emergency department complaining of right lower extremity pain and numbness associated with ambulation. The symptoms began the day after the catheterization was performed and had progressively worsened. On presentation, the patient’s vital signs were normal and he appeared comfortable. Examination of the arterial puncture site demonstrated a well-healing wound with no appreciable mass, hematoma or surrounding erythema noted. Strong femoral pulses without bruit were present bilaterally; however, pulses were decreased distal to the femoral artery puncture site. The right lower extremity was warm to the touch without pallor or mottling and with no appreciable sensory deficit.
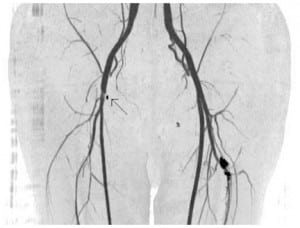
A doppler ultrasound of the right groin demonstrated normal flow in the right common femoral artery and vein with no evidence of a pseudoaneurysm. Subsequently, computed tomography (CT) angiography of the lower extremities was performed. The CT angiography demonstrated near total occlusion of the right common femoral artery just above the bifurcation and extending into the right profunda femoral artery associated with a percutaneous arterial closure device (PACD)[Figures 1 and 2].

The patient was admitted to the hospital and scheduled for surgical repair of the stenosis the following day. At the time of surgery, a flap from a Perclose PACD, along with a large blood clot underneath it, were found in the femoral artery. These were removed with return of equal and normal distal pulses.
DISCUSSION
PACD have been proposed as an alternative to manual compression to achieve hemostasis at the arterial puncture site following cardiac catheterization.1,3 It is estimated that PACDs are used to achieve hemostasis in 50% of all percutaneous coronary procedures.1 Commonly used devices employ either collagen plugs or suture-mediated closure of the arterial puncture site. The potential benefits of these devices over standard manual compression include decreased time to hemostasis, earlier ambulation and ultimately, earlier discharge of patients post catheterization.1,3
The commonly reported complications of closure devices include pseudoaneurysm, arteriovenous fistula, hematoma, femoral artery thrombosis and bleeding.1,2,3 Ischemia resulting from suture-mediated devices being deployed within the artery and arterial stenosis from suture-mediated devices are less often encountered, reported in approximately 0.2% of cases in one study of over 4,500 patients.4
The largest case series to specifically evaluate claudication secondary to PACD in percutaneous intervention patients suggests a similar incidence.5 In this single center study that evaluated approximately 4,000 patients over a one-year period, nine cases of iatrogenic claudication as a result of PACD placement were identified.6 Although pain consistent with claudication in the affected extremity was the most common presenting complaint, patients also presented with primary complaints of numbness, extremity fatigue and groin pain, complicating early diagnosis. Additionally, Arterial Brachial Index (ABI) measurements were normal in two patients in the group, suggesting that ABIs at rest are not sensitive enough to rule out the diagnosis. This is likely a reflection of the proximal location of the stenosis, particularly in patients with otherwise normal circulation whose collateral blood flow may be enough to provide adequate perfusion at rest.5 It has been suggested that performing ABIs after exercise in this group of patients would demonstrate a stenosis of clinical significance.5
Definitive diagnosis of post procedural arterial stenosis can be made accurately with duplex ultrasound, demonstrating increased turbulence and velocity of the affected artery in comparison to the unaffected side.5 Alternately, magnetic resonance or CT angiography allows adequate visualization to identify an obstructive lesion.5
Identification of clinically significant arterial stenosis is important as surgical intervention or possibly percutaneous balloon angioplasty is required to relieve the obstruction.5,6
CONCLUSION
The use of PACD to obtain hemostasis following cardiac catheterization is increasingly common. Given the complications associated with their use, ischemia from improperly placed closure devices should be considered in the differential diagnosis of all patients presenting with lower extremity pain or numbness after femoral artery cannulation.
Footnotes
Supervising Section Editor: Shahram Lotfipour, MD, MPH
Submission history: Submitted May 13, 2009; Revision Received August 26, 2009; Accepted May 24, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Luke Hermann MD, Director Chest Pain Unit, Associate Professor, Department of Emergency Medicine, The Mount Sinai School of Medicine, One Gustave Levy Place, New York, NY 10029
Email : luke.hermann@mssm.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Koreny M, Riedmuller E, Nikfardjam M, et al. Arterial puncture closing devices compared with standard manual compression after cardiac catheterization: systematic review and meta-analysis.JAMA. 2004;291:350–7. [PubMed]
2. Shammas NW, Rajendran VR, Alldredge SG, et al. Randomized comparison of Vasoseal and Angioseal closure devices in patients undergoing coronary angiography and angioplasty. Catheter Cardiovasc Interv. 2002 Apr;55(4):421–5. [PubMed]
3. Nikolsky E, Mehran R, Halkin A, et al. Vascular complications associated with arteriotomy closure devices in patients undergoing percutaneous coronary procedures: a meta-analysis. J Am Coll Cardiol. 2004 Sep 15;44(6):1200–9. [PubMed]
4. Applegate RJ, Grabarczyk MA, Little WC, et al. Vascular Closure Devices in Patients Treated With Anticoagulation and IIb/IIIa receptor Inhibitors During Percutaneous Revascularization. J Am Coll Cardiol. 2002 Jul;40(1: ):78–83. [PubMed]
5. Jang JJ, Kim M, Gray B, et al. Claudication secondary to Perclose use after percutaneous procedures. Catheter Cardiovasc Interv. 2006 May;67(5):687–95. [PubMed]
6. Dregelid E, Jensen G, Daryapeyma A. Complications associated with the Angio-Seal arterial puncture closing device: intra-arterial deployment and occlusion by dissected plaque. J Vasc Surg.2006 Dec;44(6):1357–9. [PubMed]


