| Author | Affiliation |
|---|---|
| Nicole Browne, MD | Resurrection Medical Center, Department of Emergency Medicine, Chicago, IL |
ABSTRACT
Repeat visits to an emergency department (ED) within a short period of time for recurring or continuing abdominal pain should make physicians suspicious for relapsing or episodic disease processes. I present a case of a 17-year-old female with cecal volvulus found only after multiple ED visits.
INTRODUCTION
Cecal volvulus is a surgical emergency caused by the axial twist of the cecum, distal ileum, and proximal colon in the absence of normal cecal fixation.1 While it is rare and accounts for only 1% of mechanical bowel obstructions, it is associated with significant morbidity and mortality, which increase with delay in diagnosis.2
Evaluating adolescent females with lower abdominal pain can prove to be a diagnostic challenge for clinicians, particularly if the symptoms are nonspecific and intermittent. Repeat visits to an emergency department (ED) within a short period of time for recurring or continuing abdominal pain should make physicians suspicious for relapsing or episodic disease processes.
CASE REPORT
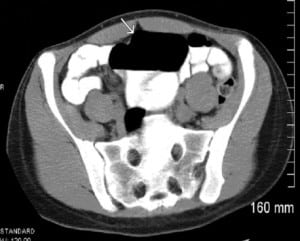
A 17-year-old female presented to the ED with one day of dull, intermittent, 6/10 abdominal pain originating in the periumbilical region and migrating to the right lower quadrant. She complained of nausea and decrease in appetite but no vomiting or diarrhea. She reported she had not had a bowel movement in three days, a normal pattern for her. She denied fever, chills or dysuria. Her medical history was positive for depression and shellfish allergy. Family history and review of systems were negative. Vital signs were normal, and the only pertinent physical exam finding was moderate tenderness in the right lower quadrant with voluntary guarding without rebound. Laboratory data revealed a normal white blood count (WBC), urinalysis, electrolytes, blood urea nitrogen and creatinine and a negative urine pregnancy test. Computed tomography (CT) of the abdomen and pelvis showed no evidence of appendicitis nor renal, hepatic, adrenal, pancreatic or bladder abnormalities. The radiologist noted a low-lying cecum dilated to 8cm but no evidence of obstruction (Figure 1). A pelvic ultrasound revealed two 1.5cm right ovarian cysts. With time the patient reported pain relief, and re-examination of her abdomen was unremarkable. She was discharged with instructions to follow up with her pediatrician and gynecologist.
The patient returned to the ED 11 hours later reporting recurring abdominal pain. The pain had increased in intensity from the previous day and was now associated with vomiting. Physical exam was significant for tenderness in the right lower quadrant with voluntary guarding. The patient refused a pelvic examination during her first visit, and the exam now failed to reveal any cervical motion tenderness, adnexal masses or tenderness. Complete blood count and chemistry profile were again normal and the patient was discharged once her pain improved with a diagnosis of abdominal pain secondary to ovarian cysts.
The patient returned to the ED 27 hours after the second visit reporting severe abdominal pain in the right lower quadrant, nausea, vomiting, and no bowel movement in four days. Her abdominal exam revealed decreased bowel sounds, distention and tenderness in the right lower quadrant with voluntary guarding. WBC was elevated (13.6) and a repeat CT showed marked dilatation of the cecum up to 10.5 cm with a transition point in the right lower quadrant suspicious for obstruction and cecal volvulus (Figure 2).

The patient was taken to the operating room for laparatomy and reduction of cecal volvulus. Surgical findings revealed a mobile cecum with serosal tears and marked distention, and the patient underwent a right hemicolectomy. Pathologic findings of the surgical specimen revealed markedly dilated ileum and cecum with evidence of ischemic necrosis. The remainder of the patient’s hospital course was unremarkable, and she was discharged on post-operative day five.
DISCUSSION
Features of cecal volvulus include the colicky nature of the patient’s pain, localization to the right lower quadrant and the low lying, dilated cecum on initial CT. The most common presenting symptoms are pain and distention, with some patients exhibiting cycles of recurring pain relieved by flatus or a bowel movement. During this patient’s first visit, she reported improvement of her pain at various intervals and at times was found to be sleeping and pain-free. These episodic events result from the mobile segment of bowel twisting and untwisting. In one study, the patients with cecal volvulus had their symptoms for a median of two days (range 1–12) before hospital admission and treatment.3
Anatomic predisposing factors, such as a mobile segment of large bowel and a fixed focal point of torsion, are usually present in these cases.4 Retroperitoneal fixation of the cecum and ascending colon fails in 10%–15% of the population,5 yet cecal volvulus remains rare, especially in childhood.6This discrepancy suggests that contributing factors, such as chronic constipation, bowel distention, pregnancy and weight loss, are likely present when a patient progresses to a volvulus. Chronic constipation and a mobile cecum found at surgery may have been significant contributing factors in this patient’s cecal volvulus. She reported she routinely only had bowel movements once every three days.
Radiographic diagnosis can often be challenging prior to definitive volvulus with obstruction due to the episodic nature of the disease, but some radiographic clues may be present. Abdominal CT has become an increasingly useful tool in diagnosing intestinal volvulus and the “whirl sign” has been well described in radiology literature.7 The whirl sign represents CT findings of intestinal twisting and the clockwise or counter clockwise direction of the volvulus. This patient did not initially have the whirl sign on her CT as her volvulus had likely spontaneously resolved at the time of her initial scan. The radiologic clue to her diagnosis on her initial CT was her dilated, low lying cecum. This, in conjunction with her colicky episodes of severe pain, could have pointed to an earlier suspicion for cecal volvulus and not ovarian cysts as the cause of her pain and possibly earlier surgical consultation or observation for serial abdominal examinations, especially on her second visit to the ED that required narcotic pain medication for relief.
Treatment of cecal volvulus involves surgical intervention, and colon resection is thought to be mandatory in the presence of cecal necrosis or perforation.2 In the absence of gangrene, the treatment is controversial but may include detorsion and/or cecopexy.8 The risk of bowel ischemia, perforation and sepsis increases with time from onset of volvulus.
CONCLUSION
Emergency physicians regularly face the challenge of identifying the source of a patient’s abdominal pain. Recognizing patients at risk for cecal volvulus based on their history, pattern of pain cycles, associated physical exam findings and radiographic findings may expedite the diagnosis and prevent further complications. This case illustrates the importance of clear communication in discharging patients with abdominal pain and their need to return if pain continues or if symptoms worsen. It also highlights the treating physician’s need for a broader differential diagnosis for patients with episodic abdominal pain and subtle radiographic findings.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted August 6, 2009; Revision Received December 1, 2009; Accepted January 11, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Nicole Browne, MD, Department of Emergency Medicine, Resurrection Medical Center, 7435 W. Talcott Ave., Chicago, IL 60631
Email: nicolebrowne@sbcglobal.net
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Rabinovici R, Simansky DA, Kaplan O, et al. Cecal Volvulus. Dis Colon Rectum. 1990 Sep;33(9):765–9. [PubMed]
2. Rogers RL, Harford FJ. Mobile Cecum Syndrome. Dis Colon Rectum. 1984 Jun;27(6):399–402.[PubMed]
3. Hiltunen KM, Syrja H, Matikainen M. Colonic Volvulus. Diagnosis and Treatment. Eur J Surg. 1992 Nov–Dec;158(11–12):607–11. [PubMed]
4. Kirks RK, Swischuk LE, Merten DF, et al. Cecal Volvulus in Children. Am J Radiology. 1981 Feb;136:419–22.
5. McGraw JP, Kremen AJ, Rigler LG. The roentgen diagnosis of volvulus of the cecum. Surgery.1948;24:793–804. [PubMed]
6. Samuel M, Boddy SA, Nicholls E, et al. Large bowel volvulus in childhood. Aust N Z J Surg. 2000 Apr;70(4):258–62. [PubMed]
7. Delabrousse E, Sarlieve P, Sailley N, et al. Cecal Volvulus: CT findings and correlation with pathophysiology. Emerg Radiol. 2007 Nov;14(6):411–5. [PubMed]
8. Meyers JR, Heifetz CJ, Baue AE. Cecal volvulus. Arch Surg. 1972;104:594–9. [PubMed]


