| Author | Affiliation |
|---|---|
| Sameer K. Khan, MRCSEd | Trauma and Orthopaedics, University Hospitals of Leicester, Leicester, UK |
| Srinivas Thati, MRCSEd | Trauma and Orthopaedics, Derriford Hospital, Plymouth, UK |
| Charles Gozzard, FRCS | Trauma and Orthopaedics, Derriford Hospital, Plymouth, UK |
ABSTRACT
A young man presented with a painful and swollen thigh, without any history of trauma, illness, coagulopathic medication or recent exertional exercise. Preliminary imaging delineated a haematoma in the anterior thigh, without any fractures or muscle trauma. Emergent fasciotomies were performed. No pathology could be identified intra-operatively, or on follow-up imaging. A review of thigh compartment syndromes described in literature is presented in a table. Emergency physicians and traumatologists should be cognisant of spontaneous atraumatic presentations of thigh compartment syndrome, to ensure prompt referral and definitive management of this limb-threatening condition.
INTRODUCTION
Compartment syndromes are orthopedic emergencies. Although extensively described in legs, their occurrence in the thigh has been rare. However, the past decade has seen a surge in thigh presentations being diagnosed and managed.1,2 Because there is usually an etiological basis for it in the patient’s history, it would be an unlikely diagnosis in a patient presenting without a suggestive history or mechanism of injury.2 Given this clinical suspicion, a prompt clinical decision can prove limb-saving.
Case Presentation
A 27-year-old man presented to the emergency department (ED) with severe pain in his left thigh. This ED is part of a Level I trauma center in the southwest of England that sees 68,000 patients annually.
The patient, who worked at a food retail shop, was normally fit and well and did not take any medication routinely. He used to run half-marathons, but had not run for at least four months. He had gone out with friends a week earlier, but could not recall any incidental trauma. He did not lie on his bed awkwardly that night, but woke up with a dull ache in his left thigh the next morning. This pain did not inhibit him from going to work over the next week and he was able to bear all his weight through both legs.
The pain worsened dramatically on the night of ED presentation, such that he was unable to weight-bear and required copious amounts of analgesics, with limited effect. He was examined by the on-call orthopedic resident at 11PM, nearly an hour after he presented to ED. He looked in distress and complained of a severe “bursting” pain, despite having had 10 mg of intravenous (IV) morphine, 1 gm of paracetamol and 50 mg of diclofenac in the preceding hour. He was afebrile, with a pulse rate of 90/min, blood pressure of 145/90 mmHg. He was tachypneic (respiratory rate 26/min), but a cardiovascular and pulmonary examination was otherwise unremarkable. His abdomen was soft and non-tender in all quadrants, with no palpable masses.
On local examination, there was no obvious wound or bruising over the left thigh. It was swollen, with a mid-thigh circumference 12 cm larger than on the right side. It was exquisitely tender as well, with an extremely tense anterior compartment. The swelling was non-pulsatile with no audible bruit. He displayed hyperesthesia in the thigh anterolaterally, with preserved sensorimotor function and pulses distally in the limb. Straight-leg raise was possible to 30 degrees, with no palpable gap in the quadriceps mechanism. Passive hip and knee movements were possible but limited by pain.
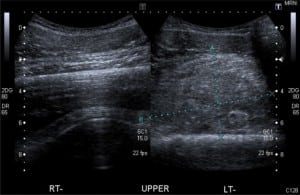
Routine blood test results revealed a low hemoglobin (10.1 g/dl, with lab range 13.0 – 17.5 g/dl), normal white cell count 9.3 x 109/L, Prothrombin time 13 sec (with lab range 12–15 sec), and APTT 32 sec (with range 26–40 sec). Urinalysis and electrocardiogram were unremarkable. Biplanar radiographs showed a soft tissue swelling anterior to the femur but no fracture. An urgent ultrasound revealed a large heterogeneous mass between the intact femoral cortex and the quadriceps muscles, with minimal internal vascularity and normal color flow in the surrounding femoral vessels, thereby ruling out a true or false aneurym (Figure). By now, the patient had been started on IV morphine via patient-controlled analgesia, but he reported no pain relief with it.
A clinical diagnosis of impending compartment syndrome due to an idiopathic hematoma was made. Worsening pain precluded any further imaging or confirmation by compartment manometry. Three hours after ED presentation, he was taken to surgery for an emergency fasciotomy and decompression of his thigh under a general anaesthetic. A lateral incision was made from the greater trochanter to the lateral femoral condoyle. The fascia lata was cut in line with the skin incision, and the vastus muscles bulged out under tension.
Beneath the muscles, a large hematoma extended into the medial compartment as well. A separate medial incision was made and the medial compartment was decompressed further through it. The posterior compartment was decompressed by dissecting through the lateral intermuscular septum. The whole hematoma was promptly evacuated. Detailed inspection showed no discontinuity, hypoperfusion or necrosis in the muscle mass. No obvious bleeding vessels could be identified. The thigh was thoroughly lavaged and dressed.
When reviewed post-operatively in the recovery bay, the patient admitted significant pain relief and was satisfied with having been offered immediate surgical evacuation. The fasciotomy wounds were washed out and closed 48 hours later, without the need for plastics intervention. He was observed closely for redevelopment of compartment syndrome, but recovered uneventfully. He was able to ambulate unaided, bearing his full weight through both legs. His wounds healed nicely and there was no recurrence of the hematoma on a repeat ultrasound six weeks later. He returned to his normal duties after that, and was asymptomatic with excellent hip and knee function, when reviewed later.
DISCUSSION
Mubarak et al3 classically described compartment syndrome due to increased pressure within a closed fascial space compromising the circulation to the nerves and muscles within the involved compartment. Compartment syndrome in the thigh is associated with significant morbidity, with long-term functional deficits reported in the literature.4,5
Unlike leg compartment syndromes, there are no true figures for the presentations in the thigh. Suzuki et al6 encountered thigh compartment syndrome in eight out of 3,658 cases of blunt trauma over a period of eight years (incidence 0.027% per year). The past decade has seen a surge in the number of cases reported globally. Most of these have been in the setting of acute musculoskeletal trauma. Ojike et al1 review of nine case series found blunt trauma to be the etiological mechanism in 90% of cases, mostly in the setting of motor vehicle accidents (34% of all cases). Forty-four percent of cases had associated femoral fractures. Femoral fractures can bleed significantly and lead to increased compartment pressures. This has been observed in both closed and open fractures, and even post-operatively after intramedullary femoral nailing.5,7–9 Gee10 reported gluteal compartment syndrome due to superior gluteal artery bleed after pelvic fracture.
Trauma without any concomitant fractures can also cause sufficient muscular damage to cause intra-compartmental hemorrhage and resultant hypertension. Muscular disruption can involve the rectus femoris, vastus intermedius, quadriceps tendon, biceps femoris and hamstrings tendon.11–16
Suzuki et al6 performed arteriograms in five out of eight thighs with compartment syndromes due to blunt trauma, and found evidence of definite arterial injury in four. Blunt trauma without any intra-operatively identifiable vascular damage has been implicated in a few other case reports.17–21 Best et al22 and Gilooly et al23 reported thigh compartment syndrome after penetrating injury with vascular damage Non-traumatic causes of thigh compartment syndrome include post-operative side effects, tumor infiltration, exercise-induced, snakebite, drug-induced, anticoagulant use and coagulopathy due to systemic comorbidity. These are summarized in Table 1.

While the diagnosis of compartment syndrome has traditionally been clinical, there is evidence that relying solely on clinical signs can under-diagnose this condition. Ulmer24 showed that the classical clinical signs were at most only 19% sensitive, with a positive predictive value of only 15%. Continuous compartment pressure monitoring can reduce the “miss-rate” in compartment syndromes associated with tibial fractures; however, this practice is not yet routine in most trauma centers in the United Kingdom.25 A recent review has concluded that a combined clinical and invasive (manometry) monitoring of an impending compartment syndrome should be instituted in the early phase after injury.26
Most of the published literature on compartment syndrome pertains to the leg (calf) only. The optimal diagnostic approach to a possible thigh compartment syndrome has not yet been determined. In Ojike’s1 review of thigh presentations in nine series, 26% were diagnosed exclusively on clinical signs, while 22% were diagnosed by compartment manometry only, and 52% by both modalities combined. The leg is more prone to developing compartment syndrome owing to the anatomical arrangement of its osteofascial compartments. Comparatively, the fascia in the thigh is more elastic, and the quadriceps and vastus muscles are voluminous.20 The thigh, therefore, has more potential space to accommodate increased volume and pressure, before circulatory compromise could ensue.27 This could possibly cause the elevated pressures to register some time after significant muscle hypoperfusion has already started to cause local effects.
Despite an exhaustive literature search, we have not found a case of thigh compartment syndrome occurring without a plausible mechanism, i.e., in the absence of any preceding or concurrent skeletal, muscular or vascular trauma, undue exertion, comorbidity or medication. It is also unique in that no obvious causative pathology was identified at surgery, either in the muscles or in the vessels of the thigh compartments. This contrasts with previous case reports where the presentation was “spontaneous,” but not idiopathic, as either muscular or vascular causes were identified at surgery.17,18,21,22
Thigh compartment syndrome is an orthopedic emergency, in which diagnostic delay can be disastrous. It is most likely to happen when the patient presents without a fracture.28 This case report enforces the need for a strong clinical suspicion of a compartment syndrome in the absence of an etiological history, but with indicative symptoms and signs.29
We acknowledge that we did not measure his thigh compartment pressures in the ED. However, the patient’s symptoms and signs betrayed severe distress, and we made the decision to explore and decompress once the large hematoma had been visualized on ultrasound. We believe that while compartment manometry has a role in aiding diagnosis, the decision to fasciotomize should not be delayed in the face of obvious clinical signs. If the signs are subtler, then compartment manometry could be employed swiftly to confirm a diagnosis of compartment syndrome.
Prompt surgical consultation is essential. The ED physicians referred this patient promptly for an orthopedic opinion, and an emergent surgical decompression was performed based on clinical diagnosis, with excellent recovery and functional outcomes.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted December 8, 2009; Revision received April 3, 2010; Accepted May 17, 2010
Reprints available through open access at http://scholarship.org/uc/uciem_westjem
Address for correspondence: Sameer K Khan, 103 Kildale House, Marton Road, Middlesbrough Ts4 3TG, UK.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Ojike NI, Roberts CS, Giannoudis PV. Compartment syndrome of the thigh: a systematic review.Injury. 2010 Feb;41(2):133–6. [PubMed]
2. Verwiebe EG, Kanlic EM, Saller J, et al. Thigh compartment syndrome, presentation and complications. Bosn J Basic Med Sci. 2009 Oct;(9 Suppl 1):28–33. [PubMed]
3. Mubarak SJ, Hargens AR, Owen CA, et al. The wick catheter technique for measurement of intramuscular pressure. A new research and clinical tool. J Bone Joint Surg Am. 1976 Oct;58(7):1016–20. [PubMed]
4. Functional outcome following compartment syndrome of the thigh: a retrospective review. J Thromb Haemost. 2003;1:TR009.
5. Mithoefer K, Lhowe DW, Vrahas MS, et al. Functional outcome after acute compartment syndrome of the thigh. J Bone Joint Surg Am. 2006 Apr;88(4):729–37. [PubMed]
6. Suzuki T, Moirmura N, Kawai K, et al. Arterial injury associated with acute compartment syndrome of the thigh following blunt trauma. Injury. 2005;36:151–9. [PubMed]
7. Choi PD, Rose RK, Kay RM, et al. Compartment syndrome of the thigh in an infant: a case report. J Orthop Trauma. 2007 Sep;21(8):587–90. [PubMed]
8. Bates J, Wamisho BL, Griffin M, et al. Ward round–late presentation of acute compartment syndrome in the thigh. Malawi Med J. 2009 Jun;21(2):85, 87. [PMC free article] [PubMed]
9. Bor N, Rozen N. Acute compartment syndrome in the thigh. Harefuah. 2008 Jan;147(1):1–7. 96.[PubMed]
10. Uzel AP, Steinmann G. Thigh compartment syndrome after intramedullary femoral nailing: possible femoral nerve block influence on diagnosis timing. Orthop Traumatol Surg Res. 2009 Jun;95(4):309–13. [PubMed]
11. Gee MJ, Tolat A, Sinha J. Acute gluteal and thigh compartment syndrome following pelvic fracture and superior gluteal artery bleed. A case report and review of the literature. Eur J Trauma Emerg Surg. 2007;33:188–91.
12. Burns BJ, Sproule J, Smyth H. Acute compartment syndrome of the anterior thigh following quadriceps strain in a footballer. Br J Sports Med. 2004 Apr;38(2):218–20. [PMC free article][PubMed]
13. Inoue H, Kumashiro T, Norimatsu T, et al. Anterior compartment syndrome of the thigh following rupture of vastus intermedius. A case report. Orthopaedics and Traumatology. 2000;49(3):741–3.
14. Kuri JA, II, DeFelice GS. Acute compartment syndrome of the thigh following rupture of the quadriceps tendon. A case report. J Bone Joint Surg Am. 2006;88:418–20. [PubMed]
15. Kampa R, Fairbank A. Acute compartment syndrome of the thigh secondary to rupture of the biceps femoris muscle. Injury Extra. 2005;36:228–9.
16. Mallo GC, Stanat SJ, Al-Humadi M, et al. Posterior thigh compartment syndrome as a result of a basketball injury. Orthopedics. 2009 Dec;32(12):923–5. [PubMed]
17. Kwong Y, Patel J. Spontaneous complete hamstring avulsion causing posterior thigh compartment syndrome. Br J Sports Med. 2006;40:723–4. [PMC free article] [PubMed]
18. Mallik K, Diduch DR. Acute Noncontact Compartment Syndrome. J Orthop Trauma.2000;14(7):509–10. [PubMed]
19. Lee AT, Fanton GS. Acute compartment syndrome of the thigh in a football athlete. J Orthop Trauma. 2005;19:748–50. [PubMed]
20. Riede U, Schmid MR, Romero J. Conservative treatment of an acute compartment syndrome of the thigh. Arch Orthop Trauma Surg. 2007;127:269–75. [PubMed]
21. Joglekar SB, Rehman S. Delayed onset thigh compartment syndrome secondary to contusion.Orthopaedics. 2009;32(8):II.
22. Best IM, Bumpers HL. Thigh compartment syndrome after acute ischemia. Am Surg.2002;68(11):996–8. [PubMed]
23. Gilooly JJ, Hacker A, Patel V. Compartment syndrome as a complication of a stab wound to the thigh: a case report and review of the literature. Emerg Med J. 2007;24:780–1. [PMC free article][PubMed]
24. Ulmer T. The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder? J Orthop Trauma. 2002 Sep;16(8):572–7. [PubMed]
25. McQueen MM, Court-Brown CM. Compartment monitoring in tibial fractures. The pressure threshold for decompression. J Bone Joint Surg Br. 1996 Jan;78(1):99–104. [PubMed]
26. Giannoudis PV, Tzioupis C, Pape HC. Early diagnosis of tibial compartment syndrome: continuous pressure measurement or not? Injury. 2009 Apr;40(4):341–2. [PubMed]
27. Schwartz JT, Jr, Brumback RJ, Lakatos R, et al. Acute compartment syndrome of the thigh. A spectrum of injury. J Bone Joint Surg Am. 1989 Mar;71(3):392–400. [PubMed]
28. Hope MJ, McQueen MM. Acute compartment syndrome in the absence of fracture. J Orthop Trauma. 2004;18:220–4. [PubMed]
29. Elliott KGB, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg Br.2003;85:625–32. [PubMed]
30. Boody AR, Wongworawat MD. Accuracy in the measurement of compartment pressures: a comparison of three commonly used devices. J Bone Joint Surg Am. 2005 Nov;87(11):2415–22.[PubMed]


