| Author | Affiliation |
|---|---|
| Eric R Schmitt, MD, MPH | Harbor–UCLA Medical Center, Department of Emergency Medicine, Torrance, California |
| Michael D Burg, MD | Kaweah Delta Medical Center, Department of Emergency Medicine, Visalia, California |
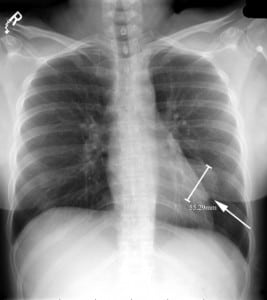
A 32-year-old female presented to the emergency department after a motor vehicle collision with complaints of thoracic back pain. Further history was not obtainable owing to marked ethanol intoxication. Vital signs and physical examination were unremarkable except for a mild tachycardia, which resolved with intravenous fluids. A chest radiograph was obtained (Figure 1). Medical records’ review revealed that the same abnormality had been noted 17 months earlier (Figure 2).

DIAGNOSIS
Most pericardial cysts are congenital, forming during embryogenesis from a persistent parietal recess.1 They are uncommon, with an estimated prevalence of 1 in 100,000 population.1,2Approximately 1 in 6 patients are symptomatic with complaints of chest pain or dyspnea.2Pericardial cysts may cause cardiac compression and may enlarge over time.1 They are easily seen on routine chest radiographs and may be an incidental finding as in our case. Diagnosis is confirmed with computed tomography or magnetic resonance imaging, and surgical treatment is indicated for symptomatic patients.1,2 Watchful observation may be feasible for asymptomatic patients, but outcome data are lacking and thus preventive resection may be preferred.2
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted April 4, 2011; Accepted April 11, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.4.2275
Address for Correspondence: Eric R. Schmitt, MD, MPH
Harbor–UCLA Medical Center, Department of Emergency Medicine, 1000 W Carson St, Box 21, Torrance, CA 90509
E-mail: ericrschmitt@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest. 2005;;128:2893–2909.[PubMed]
2. Takeda S, Miyoshi S, Minami M, et al. Clinical spectrum of mediastinal cysts. Chest.2003;;124:125–132. [PubMed]


