| Author | Affiliation |
|---|---|
| Omar K Danner, MD | Morehouse School of Medicine, Department of Surgery, Atlanta, Georgia |
| Kenneth L Wilson, MD | Morehouse School of Medicine, Department of Surgery, Atlanta, Georgia |
| Sheryl Heron, MD, MPH | Emory University School of Medicine, Department of Emergency Medicine, Atlanta, Georgia |
| Yusuf Ahmed, MD | King Saud University, Department of Epidemiology, College of Pharmacy, Riyadh, Kingdom of Saudi Arabia |
| Travelyan M Walker, MD | Morehouse School of Medicine, Department of Surgery, Atlanta, Georgia |
| Debra Houry, MD, MPH | Emory University School of Medicine, Department of Emergency Medicine, Atlanta, Georgia |
| Leon L Haley, Jr, MD, MHSA, CPE | Emory University School of Medicine, Department of Emergency Medicine, Atlanta, Georgia |
| Leslie Ray Matthews, MD | Morehouse School of Medicine, Department of Surgery, Atlanta, Georgia |
ABSTRACT
Introduction:
Although national guidelines have been published for the management of critically injured traumatic cardiopulmonary arrest (TCPA) patients, many hospital systems have not implemented in-hospital triage guidelines. The objective of this study was to determine if hospital resources could be preserved by implementation of an in-hospital tiered triage system for patients in TCPA with prolonged resuscitation who would likely be declared dead on arrival (DOA).
Methods:
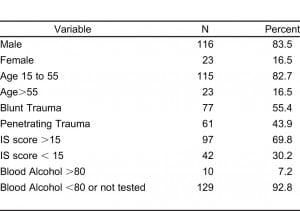
We conducted a retrospective analysis of 4,618 severely injured patients, admitted to our Level I trauma center from December 2000 to December 2008 for evaluation. All of the identified patients had sustained life-threatening penetrating and blunt injuries with pre-hospital TCPA. Patients who received cardiopulmonary resuscitation (CPR) for 10 minutes were assessed for survival rate, neurologic outcome, and charge-for-activation (COA) for our hospital trauma system.
Results:
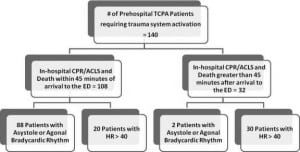
We evaluated 4,618 charts, which consisted of patients seen by the MSM trauma service from December 2001 through December 2008. We identified 140 patients with severe, life-threatening traumatic injuries, who sustained pre-hospital TCPA requiring prolonged CPR in the field and were brought to the emergency department (ED). Group I was comprised of 108 patients sustaining TCPA (53 blunt, 55 penetrating), who died after receiving < 45 minutes of ACLS after arrival. Group II, which consisted of 32 patients (25 blunt, 7 penetrating), had resuscitative efforts in the ED lasting > 45 minutes, but all ultimately died prior to discharge. Estimated hospital charge-for-activation for Group I was approximately $540,000, based on standard charges of $5000 per full-scale trauma system activation (TSA).
Conclusion:
Full-scale trauma system activation for patients sustaining greater than 10 minutes of prehospital TCPA in the field is futile and economically depleting.
INTRODUCTION
Injury and trauma-related disease remains the leading cause of death of individuals under 45 years of age in the United States.1,2 The overall cost of managing these critically injured trauma patients continues to place a significant burden upon modern trauma systems.2 Multiple reviews have demonstrated pre-hospital resuscitation efforts lasting more than 10 minutes in the field without re-establishment of adequate perfusion portend a dismal prognosis.3–7
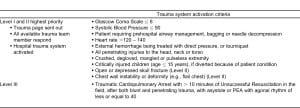
Although national guidelines for triaging the pre-hospital Traumatic Cardiac Arrest (TCPA) patients have been established by the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma (see Tables 1 and 2 for guidelines)1, not all centers have implemented out-of-hospital or in-hospital triage management protocols for termination of resuscitation (TOR). Reasons include concern regarding accuracy of history obtained at the scene, and reliability of physiologic data during transport.8–10
However, the decision to terminate resuscitation attempts in the field or to withhold resuscitation upon arrival to the emergency department (ED) remains a difficult one. A number of strategic adjustments could help to reduce the required human and material resources without significantly impairing appropriate level of trauma care.11 Moreover, some of the higher trauma care costs in the U.S. may be reduced through improvements in triaged-related practices in trauma centers.2 Improving the efficiency of trauma care delivery is particularly important as we teach the next generation of physicians the ACGME core competence of system-based practice.12 Our hypothesis is that changing to a tiered system for trauma activation, and limiting futile resuscitation practices for unquestionably moribund patients in prolonged TCPA, would decrease costs and improve the efficiency of trauma care.
METHODS
Study Design
We conducted a retrospective analysis of 4,618 critically injured patients, admitted to Grady Memorial Hospital (GMH), Atlanta, GA, a Level I trauma center, from December 2001 to December 2008. The Morehouse School of Medicine (MSM) Institutional Review Board and the Grady Research Outcome Committee approved this study. We retrospectively queried the Grady trauma registry (GTR) for the patients presenting in cardiopulmonary arrest (TCPA).
Setting
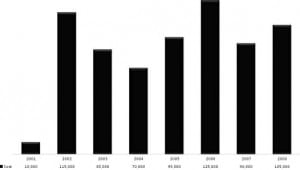
In our major metropolitan region of over approximately 5 million citizens, GMH was the only Level I trauma center during the study period, which saw 108,000 ED patients annually. Approximately 3,500 major trauma activations occur annually, of which over 2,800 are entered into the GTR annually.
Protocol
We obtained the data from the GTR, which is part of the National Trauma Registry as maintained through the American College of Surgeons. We included patients if they sustained life-threatening penetrating and blunt injuries resulting in TCPA in the field. Trauma patients who required pre-hospital advanced cardiopulmonary resuscitation (CPR) but failed to regain spontaneous perfusion after initiation of ACLS were evaluated for survival rate, neurologic outcome, and the charge-for-activation by our system. We stratified patients into two groups. Group I was comprised of 108 patients who died after 1 to 45 minutes of ACLS in the ED. Group II consisted of patients who required ACLS/CPR lasting longer than 45 minutes prior to expiration.
Data Analysis
A baseline charge of $5,000 is assessed for Level I or Level II trauma activation, which covers equipment usage, and readiness of radiology, pharmacy, laboratory, and social services. The hospital trauma-service-readiness-charge does not include x-rays, computer-assisted tomography, medications, fluids, blood, procedures or physician fees, which are estimated to be $2,588 per patient. We statistically analyzed the data using PSS 16.0 software SPSS, Chicago, IL. Data was summarized as means plus or minus standard deviation and proportion (percentages) for continuous and qualitative data, respectively. We considered a p-value < 0.5 statistically significant.
RESULTS
One hundred forty patients with severe, life-threatening traumatic injuries, who sustained pre-hospital TCPA requiring prolonged CPR in the field, were brought to the emergency department (ED). Group I was comprised of 108 patients sustaining TCPA (53 blunt, 55 penetrating), who died after receiving < 45 minutes [average of 10.2 minutes (range 1 to 45 minutes)] of ACLS after arrival to the ED. Eight-eight patients (81.5%) were asystolic or had bradycardic agonal rhythm upon arrival, and met criteria for the diagnosis of dead-on-arrival. Out of the 30 patients with data available to analyze the period of pre-hospital CPR, the average time was 15.0 minutes for Group 1 [range 1 to 37 minutes]. Group II, which consisted of 32 patients (25 blunt, 7 penetrating), had resuscitative efforts in the ED lasting > 45 minutes (average survival 15.2 hours; range 1–58.5 hours), but all ultimately died prior to discharge. Of the 32 TCPA patients with a survival > 45 minutes, 2 presented to ED in asystole. The full trauma system was activated for all patients. (Figure 1) Based on the baseline cost per activation for our Level I trauma system of $5,000 per occurrence, the estimated minimum charge by our hospital for Group I exceeded $540,000 over 8 years (Figure 2). Given that the average collection rate for ED/Trauma patients is 18%, we would expect that 82% of these charges were not reimbursed.
DISCUSSION
TCPA continues to portend a poor prognosis, particularly in the prehospital setting.10 Several case series have been presented in the past supporting this assertion. Shimazu et al, in a series of 267 TCPA patients with blunt and penetrating trauma, reported 7 of the 267 survived long term; only 4 returned to their pre-injury level of neurologic function.4 This series reported a 4% survival rate in patients with an arrest due to penetrating trauma and a 2.3% survival rate for blunt TCPA. Furthermore, Batistella et al in their series of 604 patients similarly revealed a mortality rate of 97.4%, with 7 out 16 survivors having severe neurologic devastation. 7 Interestingly, of the 346 patients who presented with either asystole or an agonal rhythm with heart rate less than or equal to 40, there were no survivors.
Despite years of research, controversy still remains surrounding the most plausible clinical criteria to waive initiation of or to terminate resuscitation in the pre-hospital setting, Expeditious restoration of perfusion is critical for survival, and CPR for TCPA lasting more than 10 minutes in the field is almost universally a lethal event.1,3–8 Understandably, the complete and irreversible cessation of life is often difficult to ascertain with complete confidence in the dynamic environment of pre-hospital emergency care. As a result, resuscitation efforts often are initiated and maintained by emergency medical services providers in many futile situations.13–18
In our study, 88 patients were brought to the ED in asystole or PEA with a bradycardic agonal rhythm and never stabilized, similar to studies by Fulton8, Mattox and Feliciano19, and Durham et al.20 Thirty-two patients responded briefly to resuscitative efforts, although they all ultimately died. Ninety-four percent of these brief responders had a heart rate > 40 and most were hypotensive, but were not pulseless or asystolic upon ED arrival. Our findings suggest that patients with sustained traumatic cardiopulmonary arrest en route requiring active, ongoing CPR may be reassessed in 10-minute intervals and stratified into responders and non-responder, based on physiologic data, such as cardiac rhythm, pulses and blood pressure. It is plausible that EM control physicians could be notified, and the trauma system activation could be downgraded to a tier-3 response. Upon reassessment by the emergency physician, ACLS could be continued or discontinued and tier-1 trauma system activation could be instituted.1
Extrapolating the data to the total trauma population triaged during this time, the estimated charges purely for trauma system activation approached $700,000 over this 8-year period. If similar rates and practices of futile triage of dead-on-arrival patients have been observed on other state and/or larger volume trauma services, the potential economic impact could be significant. Using this economic data may help promote the discussion for proper implementation of the national guidelines for withholding or termination of resuscitation for adults sustaining prolonged TCPA, especially in those futile situations in which patients meet criteria to be pronounced dead-on-arrival to hospital EDs. Whether a cost-effectiveness model can be effectively applied to the trauma setting is an area that needs further investigation. In this era of cost-conscious healthcare, it is reasonable to evaluate different triage methods, as well as mechanisms that will ultimately help to reduce and control state and national economic demands for provide quality trauma care.21–25
CONCLUSION
Adult TCPA patients who present in asystole or bradycardic agonal rhythms after 10 minutes of resuscitative efforts have a dismal prognosis. Activating the entire trauma system, as opposed to an initial assessment by the emergency medicine physician/team, in this patient subset is futile and adds significant costs to trauma and healthcare delivery. In the NAEMSP and ACS-COT position statement, “TOR may be considered when there are no signs of life and either the patient is in asystole or there is no return to spontaneous circulation after 10 minutes of CPR”. A more selective or tiered system of trauma activation could potentially result in significant cost savings for the maintenance and administration of state trauma services.26
ACKNOWLEDGMENTS
Special thanks to Dr. Lamar McGinnis for his wisdom, support, critical review of the manuscript, and guidance. Thanks to the Grady Memorial Hospital trauma registry for their support and assistance in gathering the data necessary to bring this project to fruition.
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Submission history: Submitted January 17, 2012; Revision received March 15, 2012; Accepted March 19, 2012
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.11781
Address for Correspondence: Omar K. Danner, MD
Morehouse School of Medicine, Department of Surgery, Atlanta, Georgia.
Email: odanner@msm.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Domeier R.M, McSwain N.E. Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest. J Am Col Surg. 2002;196:106–112.
2. Taheri P.A, Wahl W.L, Butz D.A, et al. Trauma service cost: the real story. Ann Surg.1998;227(5):720–725. [PMC free article] [PubMed]
3. Bailey E.D, Wydro G.C, Cone D.C. Termination of resuscitation in the prehospital setting for adult patients suffering non-traumatic cardiac arrest. National Association of EMS Physicians Standards and Clinical Practice Committee, Prehospital Emergency Care. 2000;4:190–195.
4. Shimazu S, Shatney C.H. Outcomes of trauma patients with no vital signs on hospital admission. J Trauma. 1983;23:213–216. [PubMed]
5. Rosemurgy A.S, Norris P.A, Olson S.M, et al. Prehospital traumatic arrest: the cost of futility. J Trauma. 1993;35:468–473. [PubMed]
6. Stratton S.J, Brickett K, Crammer T. Prehospital pulseless, unconscious penetrating trauma victims: field assessments associated with survival. J Trauma. 1998;45:96–100. [PubMed]
7. Battistella F.D, Nugent W, Owings J.T. et al. Field triage of pulseless trauma patients. Arch Surg.1999;134:742–746. [PubMed]
8. Fulton R.L, Voigt W.J, Hilakos A.S. Confusion surrounding the treatment of traumatic cardiac arrest.J Am Coll Surg. 1995;181:209–214. [PubMed]
9. Pasquale M.D, Rhodes M, Cipolle M.D, et al. Defining “dead on arrival:”: impact on a Level I trauma center. J Trauma. 1996;41:726–730. [PubMed]
10. Aprahamian C, Darin J.C, Thompson B.M. et al. Traumatic cardiac arrest: scope of paramedic services. Ann Emerg Med. 1985;14:583–586. [PubMed]
11. Baumol W. Social wants and dismal science: the curious case of the climbing costs of health care and teaching. Proceedings of the American Philosophical Society. 1993;137(4):612–637.
12. Stewart M.G. Resident core competencies. Accreditation Council for Graduate Medical Education.2001 Available at: http://www.acgme.org/acwebsite/RRC_280/280_corecomp.asp. Accessed March 2011.
13. Maloch M, Baumol W. Further opportunities for reduction of medical costs .J Community Health.2010;35(6):561–71. [PubMed]
14. Conrad D.A. Lessons to Apply to National Healthcare Reform. Am J Manag Care. 2009;15(10 Suppl):S306–21. [PubMed]
15. Jacobs L.M, Sinclair A, Beiser A. et al. Prehospital advanced life support: benefits in trauma. J Trauma. 1984;24:8–13. [PubMed]
16. Smith P, Bodai B.I, Hill A.S. et al. Prehospital stabilization of critically injured patients: a failed concept. J Trauma. 1985;25:65–70. [PubMed]
17. Copass M.K, Oreskovich M.R, Bladergroen M.R, et al. Prehospital cardiopulmonary resuscitation of the critically injured patient. Am J Surg. 1984;148:20–26. [PubMed]
18. Potter D, Goldstein G, Fung S.C, et al. A controlled trial of prehospital advanced life support in trauma. Ann Emerg Med. 1988;17:582–588. [PubMed]
19. Mattox K.L, Feliciano D.V. Role of external cardiac compression in truncal trauma. J Trauma.1982;22:934–936. [PubMed]
20. Durham L.A, Richardson R.J, Wall M.J, et al. Emergency thoracotomy: impact of prehospital resuscitation. J Trauma. 1992;32:775–779. [PubMed]
21. Margolin D.A, Johan D.J, Fallon W.F. Response after out of hospital cardiac arrest in the trauma patient should determine aeromedical transport to a trauma center. J Trauma. 1996;41:721–725.[PubMed]
22. Eccles M, Mason J. How to develop cost-conscious guidelines. Health Tech Assess. 2001;5:1–69.
23. Mason J, Eccles M, Freemantleet N. A framework for incorporating cost-effectiveness in evidence-based clinical practice guidelines. Health Policy. 1999;47:37–52. al. [PubMed]
24. Eddy D.M. A manual for assessing health practices and designing practice policies: the explicit approach. Philadelphia: American College of Physicians; 1992.
25. Manchikanti L, Falco F.J, Boswell M.V, et al. Facts, fallacies, and politics of comparative effectiveness research: part I. basic considerations. Pain Physician. 2010;13(1):E23–54. [PubMed]
26. Sasson C, Forman J, Krass D, et al. A qualitative study to understand the barriers to implementation of national guidelines prehospital termination of unsuccessful resuscitation efforts. Prehosp Emerg Care. 2010;14(2):250–258. [PubMed]


