| Author | Affiliation |
|---|---|
| Brandon H. Backlund, MD | Harborview Medical Center, Department of Emergency Medicine, Seattle, Washington; University of Washington School of Medicine, Division of Emergency Medicine, Seattle, Washington |
| Emily Hopkins | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado |
| John L. Kendall, MD | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado University of Colorado School of Medicine, Department of Emergency Medicine, Denver, Colorado |
ABSTRACT
Introduction:
To survey emergency physicians (EP) regarding the frequency of use of ultrasound guidance for placement of central venous catheters (UGCVC) and to assess their perceptions regarding the technique and barriers to its implementation.
Methods:
A 25-question Web-based survey was e-mailed to all members of the Colorado chapter of the American College of Emergency Physicians with a listed e-mail address. A total of 3 reminders were sent to nonresponders.
Results:
Responses were received from 116 out of 330 invitations. Ninety-seven percent (n = 112) of respondents indicated they have an ultrasound machine available in their emergency department, and 78% indicated they use UGCVC. Seventy-seven percent (n = 90) agreed with the statement, “Ultrasound guidance is the preferred method for central venous catheter placement in the emergency department.” However, 23% of respondents stated they have received no specific training in UGCVC. Twenty-six percent (n = 28) of respondents stated they felt “uncomfortable” or “very uncomfortable” with UGCVC, and 47% cite lack of training in UGCVC as a barrier to performing the technique.
Conclusion:
Although the majority of surveyed EPs feel UGCVC is a valuable technique and do perform it, a significant percentage reported receiving no training in the procedure and also reported being uncomfortable performing it. Nearly half of those surveyed cited lack of training as a barrier to more widespread implementation of UGCVC. This suggests that there continues to be a need for education and training of EPs in UGCVC.
INTRODUCTION
There is growing consensus in the medical literature that ultrasound guidance for central venous catheter placement (UGCVC) improves overall success, decreases complications, and shortens the time required to complete the procedure, when compared to anatomic landmark-based techniques.1–5 Consequently, recommendations advocating for the use of UGCVC have been adopted by various professional medical organizations and government agencies.6–10 Despite this support, it is unknown how widespread adoption of this technique is among emergency physicians (EP). Additionally, the perceptions of EPs regarding the utility and practicality of this technique are unknown, and to what degree these perceptions affect acceptance and implementation of UGCVC is unclear.
The goals of this study were to survey EPs in Colorado to obtain information about their practice and perceptions with regards to UGCVC. Secondarily, we sought to identify perceived barriers to widespread utilization of ultrasound guidance for central vascular access.
METHODS
Study Design
This was a cross-sectional, anonymous, Internet-based survey of EPs practicing in the state. Survey questions were pilot tested by a group of EPs at the authors’ institution with experience in emergency ultrasound and/or research design. Questions were then modified according to feedback received during pilot testing.
Survey questions were converted to electronic format using a Web site (zoomerang.com), which specifically provides a platform to design and deploy online surveys. Respondents answered up to 25 questions; skip logic is incorporated into the survey design, which directs respondents to answer certain questions and skip others depending on previous responses.
Selection of Participants
Special permission was obtained for this study from the Colorado chapter of the American College of Emergency Physicians (COACEP) to access a list of all members with an e-mail contact. An invitation to complete the survey, along with a hyperlink directly to the survey, was sent by e-mail to all those on the list using the survey Web site’s secure server. Three additional reminders were sent over the study period. As stipulated by COACEP, no more than 3 reminders were sent, and no other attempts at personal contact were made, such as telephone or mail. To maintain respondents’ anonymity, no identifiable data were collected in the survey responses. Data were collected over a 3-month period from August to October of 2008.
Survey data were compiled by Zoomerang and exported to the investigators as an electronic database (Excel, Microsoft Corporation, Redmond, Washington).
This study was approved by the Colorado Multiple Institutional Review Board.
Statistical Analysis
Data were transferred electronically as an Excel spreadsheet and transferred into SAS format using translational software (dfPower/DBMS Copy, DataFlux Corporation, Cary, North Carolina). All statistical analyses were performed using SAS Version 9.2 (SAS Institute Inc, Cary, North Carolina). All data are reported using descriptive statistics; differences between continuous variables are expressed as medians with 95% confidence intervals (CI), and categorical variables are expressed as percentages with 95% CIs. Statistical significance between comparisons was determined by 95% CIs and P values (P < 0.05).
RESULTS
The database provided by COACEP contained e-mail contacts for all its members for whom they had this information available in their records. There were 330 e-mail addresses on the list. All were invited to complete the survey as described earlier. One hundred sixteen responses were received for a response rate of 35%.
Demographics—Hospital Characteristics
Descriptors of the respondents’ practice environments are presented in the Table. Eighty-five percent (n = 99) of respondents reported primarily practicing in an urban or suburban area with a population greater than 50,000. The majority (59%) practice in a private or community hospital. With respect to trauma designation, 63% work in a Level 1 or Level 2 center. The median number of annual visits was 50,000 (IQR 38,000–60,000). The majority of respondents (65%) do not work in an emergency department (ED) that is affiliated with an emergency medicine (EM) residency program. To assess whether we were sampling physicians from a diversity of EDs, we asked the respondents to indicate the postal zip code for their primary practice site; 56 different zip codes within Colorado and the surrounding region were reported.
Responder Characteristics
The majority of respondents (76%) were board certified in EM, either by the American Board of Emergency Medicine or the American Osteopathic Board of Emergency Medicine. Twelve percent (n = 14) of respondents indicated they were still in residency training. The median number of years in practice postresidency was 10.5 (IQR 5.5–20).
Ninety-seven percent (n = 113) of respondents stated they have access to an ultrasound machine in their ED; 78% (n = 88) of respondents indicated that they perform UGCVC. The median overall percentage of CVCs placed using UGCVC was 75% (IQR 50–90%).
The 78% of respondents who stated that they use UGCVC indicated that they place a median of 1.9 CVCs per week (IQR 0.5–2). The 22% of respondents who stated they do not use UGCVC place a median of 0.5 central venous catheters (CVC) per week (difference: 1.4, 95% CI [0.8–1.4], P < 0.0001).
Of the 35% of respondents affiliated with a residency program, 95% use UGCVC. Of the 65% of respondents not affiliated with a residency program, 65% use UGCVC. This difference is statistically significant (difference: 30%, 95% CI [14–40%], P < 0.0009).
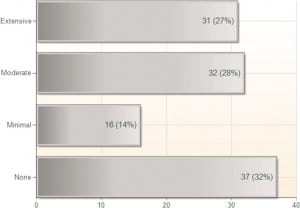
The portion of respondents in our study who said they had received minimal or no training in emergency bedside ultrasound (EBUS) during their residency was 46% (Figure 1). Although 98% of respondents said they have received some training in general EBUS, suggesting that they have pursued some form of education outside of their residency training, 23% of respondents stated they have received no specific training in UGCVC.
Of those who stated they have not received any specific training in UGCVC, 59% stated they do not perform this technique. Of those who stated they have received training in UGCVC, only 10% stated they do not use it (difference: 50%, 95% CI [31–71%], P < 0.00001).
Perceptions Regarding UGCVC
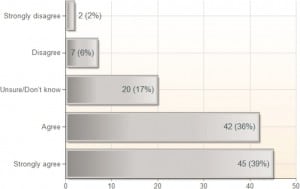
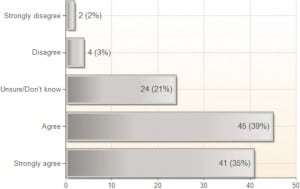
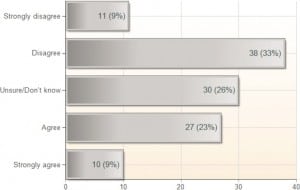
Seventy-seven percent (n = 90) of respondents indicated agreement with the statement, “Ultrasound guidance is the preferred method for central venous catheter placement in the emergency department”; 10% indicated disagreement. For the statements that UGCVC results in a higher success rate and fewer complications, the percentages of respondents indicating agreement were 75% and 74%, respectively (Figures 2 and 3). However, regarding the statement that UGCVC takes less time than the landmark-based approach, only 32% agreed, whereas 42% disagreed (Figure 4).
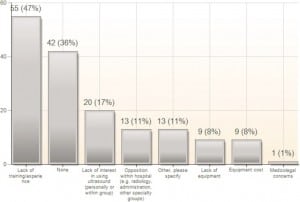
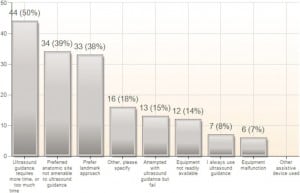
Forty-seven percent (n = 55) of all respondents cite lack of training as a barrier to implementing EBUS at their institution (Figure 5). In EDs with the capability of performing UGCVC, the top 3 reasons given for not performing it were: a perception that ultrasound guidance is more time consuming (39%), a perception that the preferred anatomic site was not amenable to ultrasound guidance (30%), and a preference for the landmark approach (29%) (Figure 6).
Overall, 26% (n = 28) of respondents stated they felt “uncomfortable” or “very uncomfortable” with UGCVC. Of those who stated they had not been trained in UGCVC, 59% (95% CI: 39–78%) stated they were “uncomfortable” or “very uncomfortable” with the technique. Of those who had been trained in UGCVC, 13% (95% CI: 7–22%) reported being “uncomfortable” or “very uncomfortable” with the technique (P < 0.0001).
DISCUSSION
There is an established and growing body of literature demonstrating superior safety and improved success using ultrasound guidance to place CVCs, as compared to traditional anatomic landmark-based techniques.1–5 In 2001, UGCVC was endorsed by the Agency for Healthcare Research and Quality as one of 11 safety practices that was “. . . most highly rated. . . in terms of strength of the evidence supporting more widespread implementation. . .”7 The following year, the British National Health Service published a similar recommendation, stating that “. . . two-dimensional. . . imaging ultrasound is recommended as the preferred method for insertion of central venous catheters. . . into the internal jugular vein. . . in adults and children. . .”8 In 2008, the American College of Surgeons issued a statement supporting “. . . the uniform use of real-time ultrasound guidance for the placement of CVCs in all patients. . .”9 The Canadian Association of Emergency Physicians endorses UGCVC,10 and ACEP has included UGCVC in its ultrasound guidelines since 2001.6,11,12
Despite these endorsements, the use of UGCVC by EPs is not uniform. In our survey, 97% of respondents had access to an ultrasound (US) machine, and 78% used UGCVC. This differs considerably from a 2006 survey by Moore et al, in which only 34% of ultrasound community EDs reported using EBUS in some form.13 Similarly, a survey by Stein et al of academic and community EDs in California found a 34% rate of use of EBUS.14 Neither of these surveys specifically investigated UGCVC, however. This difference may reflect variations in regional conditions; California’s population is larger than that of Colorado, with more hospitals and EDs, and whereas there are currently 14 EM residency programs in California alone,15 there is only 1 EM residency program in our state, with an EBUS curriculum since 1998 and an EM ultrasound fellowship since 2006.
Factors Affecting Use of UGCVC
Training
Education regarding UGCVC appears to be a very important factor influencing its use. In this survey, 47% of EPs cited lack of training in EBUS as a barrier to implementing it in their practice (Figure 1). This is similar to the survey by Moore et al13 in which lack of training was cited as the most significant barrier to implementation of EBUS. Additionally, a 2008 survey of pediatric EDs found that the most significant barrier to implementation of EBUS was lack of adequately trained EPs.16 In our survey, just under 1 in 4 responding EPs stated that they have received no specific training in UGCVC. A significantly higher percentage of physicians who had not been trained in UGCVC reported being uncomfortable with the procedure, as compared with those who had been trained. We also found significantly higher utilization of UGCVC among those who had been trained in the technique; 90% reported using it in this group, compared to 41% of those who had not been trained.
Training remains a challenge for currently practicing EPs. The advent of emergency-physician-performed bedside ultrasound has occurred relatively recently, and training in EBUS was not a mandated part of the EM residency curriculum until 2001.12 In a survey in 2003 by Counselman et al,17 95% of EM residency programs reported that they provided instruction in EBUS. However, only 21% included specific instruction in UGCVC at that time. Therefore, many EPs currently practicing did not receive training in EBUS during their residency and may not have received specific training in the technique of UGCVC. In our survey, 100% of those currently in residency (n = 14, 12%) stated they have received specific training in UGCVC, and all rated their training in EBUS as either “extensive” (79%) or “moderate” (21%). However, 88% of the respondents were not residents, and 52% of this group said they had received minimal or no training in EBUS during residency. Although 98% of all respondents said they have subsequently received some training in EBUS, indicating that they have pursued some form of education outside of their residency training, still 23% remain who indicated they have not been trained in UGCVC.
Training Centers
A significantly higher percentage of those who work with residents use UGCVC than those who do not. It appears that, in this study population, physicians at EM training centers use UGCVC more frequently than those practicing in nontraining centers.
Frequency of Procedure
Those who do not use UGCVC place significantly fewer catheters on a weekly basis than those who do. It may be that those who do not perform CVC placement as frequently do not perceive that the magnitude of the benefits of UGCVC with regard to patient safety are significant enough to make adopting the technique worthwhile.
Physician Perceptions
We included questions in the survey designed to assess the respondents’ awareness and acceptance of the consensus in the literature regarding higher success rates and fewer complications using UGCVC. Approximately three quarters of respondents agreed that UGCVC reduces complications and increases success rates and that UGCVC is the preferred method for placement of CVCs in the ED. However, the majority disagreed with the statement that UGCVC requires less time to successfully complete the procedure. This would appear to demonstrate incomplete awareness of the current literature pertaining to UGCVC (as compared to the anatomic landmark technique) among the surveyed EPs, as the benefits of higher success rates, fewer complications, and the equivalent of less time required to completion have been consistently reported.1–5 The impact of physician perception on ultrasound implementation has been shown previously, as well. Baka et al18 surveyed the use of focused assessment with sonography for trauma (FAST) among EPs and trauma surgeons who treat pediatric trauma patients, finding that the implementation of FAST was lower among those who rated the perceived utility of FAST as lower, despite contrary medical literature demonstrating its usefulness.
We feel our results underscore the need for continued EP education in UGCVC, not only as part of required EM residency training, but with regards to increasing the availability of training opportunities for practicing EPs postresidency, as well. The technique has been demonstrated in multiple studies to have advantages regarding success rates and patient safety and is advocated by governmental agencies concerned with healthcare quality. Despite this, a considerable percentage of EPs in our study still are not fully aware of the evidence-based support for the technique and either have not been trained in performing it or have not had sufficient experience with the technique to feel comfortable performing it. Our results suggest that EPs who have been trained in UGCVC become more comfortable with the technique and are more likely to perform it.
LIMITATIONS
This study has several limitations. First, the response rate was 35%. This raises the possibility that the survey sample may not be representative of all EPs in Colorado. We were limited by the constraints imposed upon us regarding access to the database, which did not include mailing addresses or telephone numbers. It is probable that if we had been able to do follow-up telephone contact and/or postal mailings, our response rate would have been higher. Also included in the database were a few incorrect or outdated e-mail addresses, which were undeliverable and decreased our response rate. We did not use an incentive or reward for completing the survey, which likely would also have increased the response rate.
We specifically surveyed members of the ACEP chapter in our state. The responses therefore could possibly represent a regional bias that would not be present in another state. This is particularly important when trying to generalize our results to other regions that may not have an established residency program or a developed ultrasound curriculum or where conditions may be otherwise different. It may also be that EPs who are not members of ACEP would respond differently to a similar survey. Further research is needed to determine how the findings of this study compare to other populations where EM is practiced. To our knowledge, there were no data available in the published medical literature regarding the frequency of use of UGCVC among EPs prior to this study. These data provide a starting point upon which to base estimates for future studies to refine our understanding of perceptions and practices among EPs regarding UGCVC.
Ninety-seven percent (n = 113) of the respondents reported that they have ultrasound available. It is possible that EPs who are not as familiar with or who do not use ultrasound were less likely to complete the survey.
Inherent in surveys such as this, in which respondents are asked to self-report regarding past practices, is the risk of recall bias, which may affect the accuracy of the respondents’ estimates.
CONCLUSION
The majority of EPs in our survey feel that UGCVC is a valuable technique and do perform it. However, nearly half of those surveyed cited lack of training as a barrier to performing EBUS, and approximately 1 in 4 reported receiving no training in UGCVC. A similar proportion also reported being uncomfortable performing this procedure, suggesting that there still exists a need for training of EPs in this technique.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence
Brandon H. Backlund, MD
University of Washington School of Medicine, Division of Emergency Medicine, Harborview Medical Center
325 9th Ave, 3EC-26, Seattle, WA 98104
E-mail: bbswing@u.washington.edu
REFERENCES
1. Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327:361. [PMC free article] [PubMed]
2. Denys BG, Uretsky BF, Reddy PS. Ultrasound-assisted cannulation of the internal jugular vein—a prospective comparison to the external landmark-guided technique. Circulation. 1993;87:1557–1562.[PubMed]
3. Hrics P, Wilber S, Blanda M, et al. Ultrasound-assisted internal jugular vein catheterization in the ED.Am J Emerg Med. 1998;16:401–403. [PubMed]
4. Miller A, Roth B, Mills T, et al. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the emergency department. Acad Emer Med. 2002;9:800–805.
5. McGee D, Gould M. Preventing complications of central venous catheterization. N Eng J Med.2003;348:1123–1133.
6. American College of Emergency Physicians policy statement: emergency ultrasound guidelines.American College of Emergency Physicians Web site. Available at:http://www.acep.org/WorkArea/DownloadAsset.aspx?id=32878. Accessed July 2, 2010.
7. Shojania K, Duncan B, McDonald K, et al. Making healthcare safer: a critical analysis of patient safety practices. Agency for Healthcare Research and Quality Web site. Available at:http://archive.ahrq.gov/clinic/ptsafety/. Accessed July 2, 2010.
8. British National Health Service, National Institute for Clinical Excellence. Final appraisal determination: ultrasound locating devices for placing central venous catheters. National Institute for Health and Clinical Excellence Web site. Available at: http://www.nice.org.uk:80/guidance/index.jsp?action=article&r=true&o=32460. Accessed July 2, 2010.
9. American College of Surgeons. Statement on recommendations for uniform use of real-time ultrasound guidance for placement of central venous catheters. American College of Surgeons Web site.Available at: http://www.facs.org/fellows_info/statements/st-60.html. Accessed July 2, 2010.
10. Canadian Association of Emergency Physicians. Position statement: emergency department targeted ultrasound: 2006 update. Canadian Association of Emergency Physicians Web site. Available at:http://www.caep.ca/CMS/get_file.asp?id=9da9e78c35ae4fa681b8f98a3bc98794&ext=.pdf&name=Ultrasound_PositionStatement_-_jul21.05.pdf. Accessed July 2, 2010.
11. Hockberger RS, Binder LS, Graber MA, et al. The model of the clinical practice of emergency medicine. Ann Emerg Med. 2001;37:745–770. [PubMed]
12. Heller M, Mandavia D, Tayal V, et al. Residency training in emergency ultrasound: fulfilling the mandate. Acad Emerg Med. 2002;9:835–839. [PubMed]
13. Moore C, Molina A, Lin H. Ultrasonography in community emergency departments in the United States: access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006;47:147–153. [PubMed]
14. Stein JC, River G, Kalika I, et al. A survey of bedside ultrasound use by emergency physicians in California. J Ultrasound Med. 2009;28:757–763. [PubMed]
15. Society for Academic Emergency Medicine. Emergency medicine residency catalog. Available at:http://www.saem.org/saemdnn/TestResidencyPage/California/tabid/781/Default.aspx. Accessed July 2, 2010.
16. Ramirez-Schrempp D, Dorfman DH, Tien I, et al. Bedside ultrasound in pediatric emergency medicine fellowship programs in the United States: little formal training. Pediatr Emerg Care.2008;24:664–667. [PubMed]
17. Counselman FL, Sanders A, Slovis CM, et al. The status of bedside ultrasonography training in emergency medicine residency programs. Acad Emerg Med. 2003;10:37–42. [PubMed]
18. Baka A, Delgado C, Simon H. Current use and perceived utility of ultrasound for evaluation of pediatric compared with adult trauma patients. Pediatr Emerg Care. 2002;18:163–167. [PubMed]


