| Author | Affiliation |
|---|---|
| John L. Kendall, MD | Denver Health Medical Center, Department of Emergency Medicine |
| Jeffrey Faragher, MD | Providence Everett Medical Center, Department of Emergency Medicine |
| Gwendolyn J. Hewitt, MD | Lutheran Medical Center, Department of Emergency Medicine |
| Gregory Burcham, MD | Swedish Medical Center, Department of Emergency Medicine |
| Jason S. Haukoos, MD, MSc | University of Colorado at Denver and Health Sciences Center, Department of Preventative Medicine and Biometrics |
ABSTRACT
Introduction:
To estimate the sensitivity and specificity of emergency department (ED) ultrasound for the detection of solid organ injury following blunt abdominal trauma.
Methods:
A prospective cohort study performed in the ED of an urban Level I trauma center on patients who sustained blunt abdominal trauma. Following initial standard trauma evaluation, patients underwent a secondary ultrasound examination performed specifically to identify injury to the liver or spleen, followed by computed tomography (CT) scan of the abdomen. Ultrasound examinations were performed by emergency medicine residents or attending physicians experienced in the use of ultrasound for detecting hemoperitoneum. Ultrasonographers prospectively determined the presence or absence of liver or spleen injury. CT findings were used as the criterion standard to evaluate the ultrasound results.
Results:
From July 1998 through June 1999, 152 patients underwent secondary ultrasound examination and CT. Of the 152 patients, nine (6%) had liver injuries and 10 (7%) had spleen injuries. Ultrasound correctly detected only one of the liver injuries for a sensitivity of 11% (95% CI: 0%–48%) and a specificity of 98% (95% CI: 94%–100%). Ultrasound correctly detected eight spleen injuries for a sensitivity of 80% (95% CI: 44%–98%) and a specificity of 99% (95% CI: 95%–100%).
Conclusion:
Emergency ultrasound is not sensitive or specific for detecting liver or spleen injuries following blunt abdominal trauma.
INTRODUCTION
Ultrasound is a rapid, portable, real-time study that has become integral to the emergency department (ED) management of blunt trauma. A number of studies have demonstrated that the Focused Assessment with Sonography for Trauma (FAST) examination can effectively detect hemoperitoneum and expedite appropriate patient disposition.1–4
A reported limitation of ultrasound in the setting of blunt trauma is poor specificity for determining the source of hemoperitoneum, as well as a limited ability to detect solid organ injury (SOI) in the absence of free fluid.5 Several studies in the emergency medicine, radiology, and surgery literature have attempted to determine the utility of ultrasound in this setting, but the results have been difficult to evaluate. For example, one study reported sensitivities as low as 41% for the detection of SOI5 while another documented sensitivities of greater than 90%.6 Most authors attribute these discrepancies to the sonographer’s experience, the affected organ being visualized, the severity of injury, which criterion standard was used for determining the presence of SOI, and when the ultrasound was performed relative to the timing of the injury.
Many of the prior studies also had variable methods, which may account for their conflicting results. Unfortunately, this has made their extrapolation to patient management difficult. To address these issues, we devised a prospective study to control many of the aforementioned variables. The education of the emergency sonographers was standardized, the timing of the ultrasound examination relative to the criterion test was explicitly stated, and the imaging study used for comparison to the ultrasound examination was predetermined. The objective of this study was to estimate the sensitivity of ultrasound performed by emergency physicians for the detection of liver and spleen injuries in patients who suffered blunt abdominal trauma.
METHODS
This study was approved by the Research Committee and the Institutional Review Board from our institution and met criterion for exemption of informed consent.
Study Design and Setting
This was a prospective cohort study performed in the ED at an urban level I trauma center. The annual ED census is approximately 55,000 visits, and the annual major trauma census is approximately 2,500.
Study Population
A convenience sample of patients who presented to the ED following blunt abdominal trauma and who subsequently received computed tomography (CT) scans of the chest or abdomen during their evaluations were included. Following initial trauma evaluation, which includes a four-view ultrasound examination to detect hemoperitoneum or pericardial effusion, eligible patients underwent a secondary ultrasound examination while awaiting CT. The specific purpose of the secondary ultrasound was to evaluate the liver and splenic parenchyma for SOI. The secondary ultrasound consisted of long- and short-axis scans through both organs. Hard-copy images of representative views and any injuries were saved. Studies were performed using a Toshiba SSH-140A (Toshiba, San Francisco, CA) with a 3.75 MHz phased array transducer. Patients were excluded from the study if they were transferred from another facility with known SOI, if the CT was interrupted or not completed, if performing the secondary ultrasound would delay necessary patient care, or if the trauma was not a blunt mechanism.
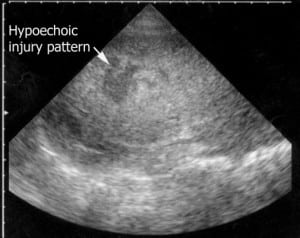
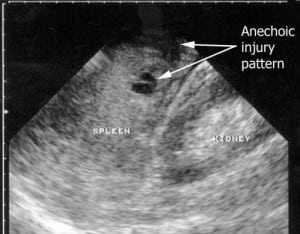
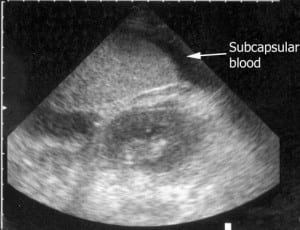
Resident and attending physicians performed all secondary ultrasound examinations. Both groups had previously completed a standardized eight-hour didactic and practical trauma ultrasound curriculum. This entailed a one-hour lecture on physics and instrumentation, a two-hour lecture on abdominal ultrasound for trauma, and a one-hour lecture on echocardiography. Following this, each participant completed four hours of hands-on instruction. Within the didactic portion of the curriculum, participants were instructed on additional transducer views needed to detect SOI and the appearance of normal and abnormal solid organ architecture. Additionally, each month when new ED residents began their clinical rotations at the study site, they reviewed representative ultrasound images and videotaped examinations of SOI. Solid organ injury was defined as a hyperechoic or hypoechoic region within the organ parenchyma (Figure 1), disruption of organ architecture (Figure 2), or a subcapsular fluid collection (Figure 3).7 The secondary ultrasound was performed just prior to the patient being transported to the CT suite.
Data Collection
Upon completion of the secondary ultrasound, the physician who performed the examination completed a standardized data collection instrument. Recorded information included: patient age and sex; medical record number; mechanism of trauma; initial vital signs; presence of liver or spleen injury or fluid collection; total number of FAST exams performed by the physician; the length of time to complete the examination; and the presence and location of hemoperitoneum. The criterion diagnostic standard was made using CT. All CT interpretations were performed by attending radiologists who were blinded to the results of the secondary ultrasound examination.
Data Management and Statistical Analyses
All data were entered into an electronic database (MS Excel, Microsoft Corporation, Richmond, WA) and translated in native SAS format using translational software (dfPower/DBMS Copy, Dataflux Corporation, Cary, NC). All statistical analyses were performed using SAS Version 9.1 (SAS Institute, Inc., Cary, NC) or Stata Version 9 (Stata Corporations, College Station, TX). Descriptive statistics were performed for all variables. Continuous variables are reported as medians and interquartile ranges (IQRs) and categorical variables are reported as percentages and 95% confidence intervals (CIs). Sensitivities, specificities, positive predictive values (PPV) and negative predictive values (NPV) are reported, where appropriate.
RESULTS
During the one-year study period, 164 patients were enrolled. Of these, six (4%) had incomplete medical records, two (1%) sustained stab wounds, and one (0.6%) was a non-trauma patient. One (0.6%) patient was transferred after laparotomy from an outside facility with known SOI, and one (0.6%) had a known splenic laceration from a previous ED visit. Lastly, one (0.6%) patient went directly to the operating room and did not receive a CT scan. These patients were excluded from analysis, leaving 152 (92%) patients, which constitute our study sample.
The median age of this cohort was 34 (IQR 25–47, range 6–91 years). Ninety-five (63%) of the patients were male. Of the 152 patients, 98 (65%) were involved in motor vehicle crashes, three (2%) were involved in motorcycle crashes, 21 (14%) suffered falls, 11 (7%) were assaulted, 11 (7%) were involved in auto-pedestrian accidents, and four (2.7%) were involved in bicycle accidents. All but 10 of the secondary ultrasound exams were performed in less than 10 minutes. The experience level of the ultrasound examiner ranged from 27 (20%) having performed 0–25 trauma ultrasounds, 30 (22%) performed 26–50, 18 (13%) performed 51–75, 23 (17%) performed 76–100, and 36 (27%) had performed greater than 101 trauma ultrasounds previously.
There were nine (5%) liver injuries detected by CT scan. One patient had no identifiable parenchymal injury; however, subcapsular fluid was detected on CT scan, so the patient was classified as having a SOI. None of the parenchymal abnormalities were detected during the secondary ultrasound exam. One patient was noted to have subcapsular fluid on ultrasound and CT confirmed the fluid, as well as the presence of a stellate liver laceration. Thus, the sensitivity of ultrasound for the detection of hepatic injuries was 11% (95% CI: 0%–48%). In total, there were four ultrasound studies interpreted as having either parenchymal injury or subcapsular fluid. Only one of these patients had SOI confirmed by CT scan, yielding a specificity of 98% (95% CI: 94%–100%).
Of the eight liver injuries ultrasound failed to detect, none required transfusion or operative intervention. All of these patients were observed and discharged from the hospital with no immediate complications.
CT scan identified10 spleen injuries. All had parenchymal injury with seven having corresponding subcapsular fluid. Ultrasound correctly identified eight out of 10 injuries, detecting either the parenchymal abnormality or subcapsular fluid, but not necessarily both. Six out of 10 parenchymal abnormalities were detected during the secondary ultrasound exam. Ultrasound identified five of seven patients with subcapsular fluid collections. There were three patients interpreted by ultrasound to have subcapsular fluid, which was not present on the CT scan. Overall, the sensitivity of ultrasound for detecting either fluid or a parenchymal injury was 80% (95% CI: 44%–98%), and the specificity was 99% (95% CI: 95%–100%).
The two patients with splenic injuries not detected by ultrasound were observed in the hospital and discharged safely. One patient suffered a pulmonary embolus and was successfully anti-coagulated without complications. None required surgery or transfusion.
DISCUSSION
Ultrasound has become an important tool for the management of patients sustaining blunt abdominal trauma. Since the report by Tso et al.,2 many prospective studies have demonstrated the accuracy of ultrasound in detecting hemoperitoneum after blunt trauma. The ability of emergency physicians and surgeons to perform ultrasound quickly, accurately, and reliably has led to its nearly universal acceptance in trauma centers. While ultrasound can reliably detect hemoperitoneum, determining the source of bleeding is a much harder proposition. Similarly confounding is the scenario of SOI without intraperitoneal rupture of blood.
The goal of this study was to define an emergency physician’s ability to detect SOI after a brief training period. While several groups have previously attempted to determine the utility of ultrasound for this indication, many of the studies have yielded mixed results. For instance, Yoshii et al.6 reported sensitivities of 92% and 90% for the ultrasound detection of liver and spleen injuries, respectively. In another study, the same group published data using CT and laparotomy as criterion standard tests to compare interpretations from experienced and inexperienced sonographers.8 In the experienced group, sensitivities for liver and spleen injuries were 87.5% and 85.4%, respectively. In contrast, the inexperienced group had lower sensitivities for detection of liver and spleen injuries at 46.2% and 50%, respectively. One criticism of both studies was the incidence of SOI in the enrolled population was over 30%, which is significantly higher than most United States trauma centers.
Goletti et al.9 demonstrated a slightly lower sensitivity for liver injuries (80%) but a higher sensitivity for spleen injuries (93%). Similar to the previously mentioned studies, Goletti et al. used an unremarkable clinical course and negative repeat ultrasound to define patients without injury, possibly yielding a falsely elevated true negative rate.
In contrast to the prior studies, McGahan et al.10 reported detection rates of 14% for liver injuries and 69% for spleen injuries, which are similar to our results. The same group later demonstrated higher sensitivities for both liver and spleen injuries, but this was most pronounced in injuries that were either Grade III and higher.11,12
Our study suggests that ultrasound, when performed by emergency physicians, is not a sensitive detector of SOI. There are several reasons this may be true. In an ideal setting, the ability to detect SOI by ultrasound is a difficult examination, even for experienced sonographers. Rothlin et al.13 showed a 10% increase in sensitivity for detecting SOI between surgeons who had performed 200 examinations and those who had performed 4,000 examinations. The results of the Yoshii et al.6 study confirm the value of experience in the detection of SOI. Many of the ultrasound examinations in our study were performed by residents or attendings who had relatively little experience with this particular examination (less than 100 prior examinations), which possibly contributed to the low sensitivity of findings.
The ability to detect SOI by ultrasound also relates to the severity of the injury. Grade 4 and 5 liver injuries, for example, are typically easier to visualize than Grade 1 and 2 injuries.11,12 In our study, all of the missed injuries were either Grade 1 or 2. Furthermore, none of the patients with missed injuries received blood transfusions or required operative intervention. This implies that ultrasound did not miss any clinically significant injuries. It is also possible that several patients with easily detectable injuries during the initial trauma ultrasound exam went directly to the operating room or interventional radiology suite secondary to a grossly positive FAST exam or unstable hemodynamic status and therefore they were not enrolled in this study.
Another potential explanation for our reported low sensitivity of ultrasound to detect SOI was how rapidly the ultrasound was performed after the patient’s arrival. All but two of the patients had the secondary ultrasound performed in less than 10 minutes after the patient’s arrival to the ED. Perhaps an ultrasound examination repeated later in the patient’s clinical course would have detected injury and fluid with greater reliability.
LIMITATIONS
There are several limitations of this study. The small number of injuries hinders our ability to make a more accurate determination of sensitivity and positive predictive value. Second, our study initially intended to enroll patients consecutively, but demands of the ED prevented this from occurring regularly. Subsequently, the study population is best described as a convenience sample, thus allowing for possible selection bias. Since we only included patients who were stable enough to complete a CT scan, our study population likely selected a greater number of minor injuries. It should also be noted that the ultrasound equipment used for this study is outdated by current standards. Consequently, our results may underestimate the ability of ultrasound to detect SOI. Lastly, physicians performing the secondary ultrasound were frequently the same physician treating the patient, and therefore they were not blinded to the results of the initial ultrasound. Knowledge of the presence or absence of hemoperitoneum in the initial ultrasound may have biased the interpretation of questionable findings on the secondary study.
CONCLUSION
Our findings suggest that ultrasound, as performed by ED resident and attending physicians, has a low sensitivity for detecting hepatic injuries. Splenic injuries were detected more successfully when visualization of parenchymal injury or subcapsular fluid was considered a positive examination. CT scanning remains the preferable modality to detect SOI.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Submission history: Submitted June 09, 2008; Revision Received August 28, 2008; Accepted September 19, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: John Kendall, MD FACEP. Department of Emergency Medicine, MC 0108, Denver Health Medical Center, 660 Bannock Street, Denver, CO 80204
Email: John.Kendall@dhha.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. McKenney M, Lentz K, Nunez D, Sosa JL, Sleeman D, Axelrad A, Martin L, Kirton O, Oldham C. Can ultrasound replace diagnostic peritoneal lavage in the assessment of blunt trauma? . J Trauma. 1994;37:439–441. [PubMed]
2. Tso P, Rodriguez A, Cooper C, et al. Sonography in blunt abdominal trauma: a preliminary progress report. J Trauma. 1992;33:39–43. discussion 43–34. [PubMed]
3. Boulanger BR, Brenneman FD, McLellan BA, et al. A prospective study of emergent abdominal sonography after blunt trauma. J Trauma. 1995;39:325–330. [PubMed]
4. Ma OJ, Mateer JR, Ogata M, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38:879–885.[PubMed]
5. Poletti PA, Kinkel K, Vermeulen B, et al. Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? . Radiology. 2003;227:95–103. [PubMed]
6. Yoshii H, Sato M, Yamamoto S, et al. Usefulness and limitations of ultrasonography in the initial evaluation of blunt abdominal trauma. J Trauma. 1998;45:45–50. discussion 50–41. [PubMed]
7. Asher WM, Parvin S, Virgillo RW, et al. Echographic evaluation of splenic injury after blunt trauma. Radiology. 1976;118:411–415. [PubMed]
8. Sato M, Yoshii H. Reevaluation of ultrasonography for solid-organ injury in blunt abdominal trauma. J Ultrasound Med. 2004;23:1583–1596. [PubMed]
9. Goletti O, Ghiselli G, Lippolis PV, et al. The role of ultrasonography in blunt abdominal trauma: results in 250 consecutive cases. J Trauma. 1994;36:178–181. [PubMed]
10. McGahan JP, Rose J, Coates TL, et al. Use of ultrasonography in the patient with acute abdominal trauma. J Ultrasound Med. 1997;16:653–662. quiz 663–654. [PubMed]
11. Richards JR, McGahan JP, Pali MJ, et al. Sonographic detection of blunt hepatic trauma: hemoperitoneum and parenchymal patterns of injury. J Trauma.1999;47:1092–1097. [PubMed]
12. Richards JR, McGahan JP, Jones CD, et al. Ultrasound detection of blunt splenic injury. Injury. 2001;32:95–103. [PubMed]
13. Rothlin M, Naf R, Amgwerd M, et al. How much experience is required for ultrasound diagnosis of blunt abdominal trauma? Langenbecks Arch Chir. 1992;377:211–215.[PubMed]