| Author | Affiliation |
|---|---|
| Ruhee Shah, BS | Icahn School of Medicine at Mount Sinai, New York, New York |
| Alessandra Della Porta, BS | University of Miami Miller School of Medicine, Miami, Florida |
| Sherman Leung, BS | Icahn School of Medicine at Mount Sinai, New York, New York |
| Margaret Samuels-Kalow, MD | Massachusetts General Hospital/Harvard Medical School, Department of Emergency Medicine, Boston, Massachusetts |
| Elizabeth M. Schoenfeld, MD | University of Massachusetts Medical School-Baystate, Department of Emergency Medicine, Springfield, Massachusetts |
| Lynne D. Richardson, MD | Icahn School of Medicine at Mount Sinai, Department of Emergency Medicine, New York, New York; Icahn School of Medicine at Mount Sinai, Department of Population Health Science and Policy, New York, New York; Icahn School of Medicine at Mount Sinai, Institute for Health Equity Research, New York, New York |
| Michelle P. Lin, MD, MPH, MS | Icahn School of Medicine at Mount Sinai, Department of Emergency Medicine, New York, New York; Icahn School of Medicine at Mount Sinai, Department of Population Health Science and Policy, New York, New York; Icahn School of Medicine at Mount Sinai, Institute for Health Equity Research, New York, New York |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Social emergency medicine (EM) is an emerging field that examines the intersection of emergency care and social factors that influence health outcomes. We conducted a scoping review to explore the breadth and content of existing research pertaining to social EM to identify potential areas where future social EM research efforts should be directed.
Methods
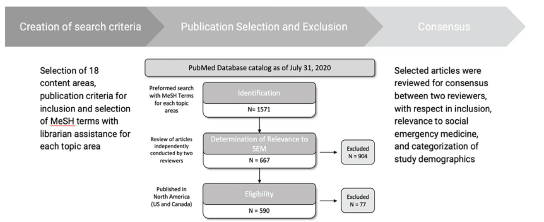
We conducted a comprehensive PubMed search using Medical Subject Heading terms and phrases pertaining to social EM topic areas (e.g., “homelessness,” “housing instability”) based on previously published expert consensus. For searches that yielded fewer than 100 total publications, we used the PubMed “similar publications” tool to expand the search and ensure no relevant publications were missed. Studies were independently abstracted by two investigators and classified as relevant if they were conducted in US or Canadian emergency departments (ED). We classified relevant publications by study design type (observational or interventional research, systematic review, or commentary), publication site, and year. Discrepancies in relevant publications or classification were reviewed by a third investigator.
Results
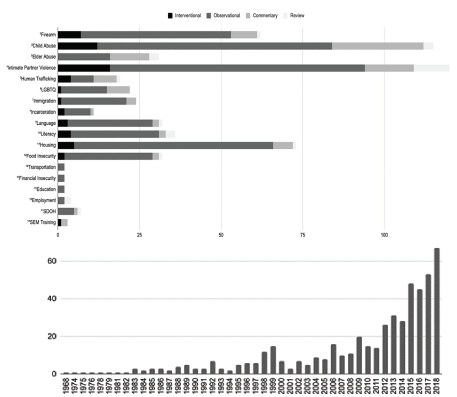
Our search strategy yielded 1,571 publications, of which 590 (38%) were relevant to social EM; among relevant publications, 58 (10%) were interventional studies, 410 (69%) were observational studies, 26 (4%) were systematic reviews, and 96 (16%) were commentaries. The majority (68%) of studies were published between 2010–2020. Firearm research and lesbian, gay, bisexual, transgender, and queer (LGBTQ) health research in particular grew rapidly over the last five years. The human trafficking topic area had the highest percentage (21%) of interventional studies. A significant portion of publications — as high as 42% in the firearm violence topic area – included observational data or interventions related to children or the pediatric ED. Areas with more search results often included many publications describing disparities known to predispose ED patients to adverse outcomes (e.g., socioeconomic or racial disparities), or the influence of social determinants on ED utilization.
Conclusion
Social emergency medicine research has been growing over the past 10 years, although areas such as firearm violence and LGBTQ health have had more research activity than other topics. The field would benefit from a consensus-driven research agenda.
INTRODUCTION
Background and Importance
In 1848 Rudolph Virchow declared social problems to be “largely within the jurisdiction” of physicians.1,2 Emergency physicians serve as safety net providers and are often on the front line of epidemics, natural disasters, and civil unrest.3 The emergency department (ED) is a unique place to identify and intervene in social issues, as patients often present with complaints directly influenced by social determinants of health (SDOH),4 and EDs serve patients who have limited access to care.5 As a result, the field of social emergency medicine (EM) has developed to examine and influence social factors in the context of acute healthcare needs. The scope of social EM is immense, including domains from housing insecurity to substance use, to gun and intimate partner violence, and many others. Many domains within social EM are known to influence emergency care utilization and health outcomes.
Goals of This Investigation
While prior systematic reviews have examined the existing literature with a specific focus on material needs, there is a need to characterize the literature examining the broader field of social factors, including non-material factors – such as language, exposure to violence, and immigration status – known to influence emergency care and outcomes.6 The primary aims of this scoping review were to understand and map the breadth of current literature for various social EM topics and categorize the type of research that exists for each topic, in order to identify potential areas where future social EM research efforts should be directed.
METHODS
This review was informed by the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines for scoping reviews. We identified 11 content areas based on a previously published systematic review of patients’ social and economic needs, including housing needs, employment needs, education and literacy, financial insecurity, personal safety (including intimate partner violence, human trafficking, firearms, child abuse, and elder abuse), and food insecurity.7 Additional topic areas were added based on author consensus, including lesbian, gay, bisexual, transgender, and queer (LGBTQ) health, language, immigration, incarceration, and transportation needs. Two final search terms (“social determinants of health” and “social emergency medicine training”), were added in consultation with a research librarian to ensure inclusion of publications that address more than one topic, as well as educational research.
We conducted a comprehensive literature search using a combination of Medical Subject Heading (MeSH) terms and phrases pertaining to topic areas (eg, “homelessness,” “housing instability”). We restricted studies to those conducted in the US or Canada. Given the focus on social EM, we included the MeSH terms (((“Emergency Service, Hospital”[Majr]) OR (emergency (room[Title] OR department[Title] OR medicine[Title] OR care[Title] OR visit[Title])))). A full list of search terms can be found in Appendix A.
We used the PubMed database for our searches, with the exception of the “Social Emergency Medicine Training” search, which also used the MedEd Portal database. For searches that yielded fewer than 100 total publications, we used the PubMed “similar publications” tool to expand the search and ensure no relevant publications were missed. Criteria for inclusion were as follows: (1) published in English; (2) conducted in the US or Canada through July 31, 2020; and (3) deemed relevant to social EM. Studies were considered relevant to social EM if they focused on social factors in the context of acute healthcare needs; therefore, we included the following criteria: 1) the study population consisted of ED patients or emergency clinicians; 2) the study or intervention occurred in the ED; or (3) ED utilization or outcomes were defined as a primary outcome.
Once a publication was deemed to meet inclusion criteria we extracted additional information such as title, PubMed ID, year of publication, and study design type (original observational or interventional research, systematic review, or commentary) into a standardized data collection form. We further catalogued observational and interventional publications by setting (single center, multicenter regional, and multicenter national). For each publication, study objectives (eg, defining prevalence, evaluating an educational intervention) were also recorded. For search results in each topic area, two co-investigators independently assessed each study for inclusion and relevance to social EM, Any discrepancies in relevance or categorization were reviewed and reconciled by a third reviewer. We also classified publications classified as relating to pediatric populations if they included children or adolescents (≤ 21 years) or if they were conducted in pediatric EDs.
RESULTS
Our search strategy identified 1571 publications, of which 590 publications in 18 categories were classified as relevant to social EM. Depiction of search strategy and classification process are in Figure 1. The study designs of included publications were as follows: 58 (10%) interventional publications; 410 (69%) observational publications; 26 (4%) systematic reviews; and 96 (16%) commentaries. Publication years ranged from 1968 to 2020, with 402 (68%) eligible articles published since 2010. Results are summarized in Figure 2. Study objectives within each topic are summarized in the Table.
| Topic area (590) | Study objectives |
|---|---|
| Firearms (62) | PrevalencePatient characteristicsRisk factors for violence SeverityScreening Psychiatric (Lethal means counseling)Patient and provider perspectives towards discussing firearm safety |
| Child abuse (114) | PrevalencePatient characteristicsInjury patternsSexual assaultScreeningProvider knowledge/trainingEducational interventions |
| Elder abuse (31) | Prevalence Patient characteristicsScreening ED utilizationInjury patterns Provider knowledge |
| Intimate partner violence (120) | PrevalenceScreeningPatient characteristicsRisk factorsPsychiatric (substance use/mental health)Patient and provider perspectives on IPV screeningEducational interventions |
| Human trafficking (19) | Patient characteristicsScreeningEducational interventions |
| Lesbian, gay, bisexual, transgender, and queer health (22) | Prevalence of IPVCare of transgender patientsPatient and provider attitudes towards sexual orientation and gender identity data collectionCompetency trainingEducational intervention |
| Immigration (24) | ED utilizationPreventative care intervention |
| Incarceration (11) | ED utilization (post-release)Models of Care (interventional) |
| Language (32) | Aspects of ED care (triage, HPI, management of care, interpreter utilization, ED resource utilization, length of stay, discharge, follow-up care)Effectiveness of bilingual triage/medical history (interventional) |
| Literacy (34) | Screening (literacy and health literacy)Understanding discharge instructionsED utilizationCommunication toolsEducational interventions (parents of pediatric patients) |
| Housing/homelessness (73) | ED utilizationPatient characteristicsPsychiatric (substance use and mental health)Patient and provider perspectivesCase management interventions |
| Food insecurity (29) | Prevalence ED utilizationScreeningCost of careHealth effects of food insecurityDiabetesSNAP and chronic illnessFood access intervention |
| Transportation (2) | ED accessPsychiatric patients |
| Financial insecurity (2) | Financial burden of specific chief complaints |
| Education (2) | ED utilizationPain management |
| Employment (3) | ED utilization |
| Social determinants of health (8) | ED utilization |
| SEM training (3) | Educational Intervention |
ED, emergency department, IPV, intimate partner violence; HPI, history of present illness.
ED, emergency department; SNAP, Supplemental Nutrition Assistance Program; SEM, social emergency medicine.
Figures 3A through 3D show study type by year for select topics with the largest number of studies (firearms, intimate partner violence, child abuse, and housing/homelessness).
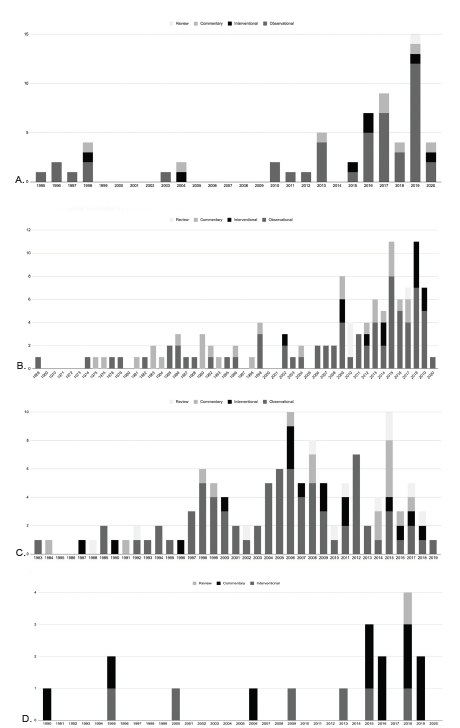
Firearms
We identified 62 relevant publications 8-69: 46 observational studies; seven interventional studies18,38,55,60,64,66,67; one systematic review15; and eight commentaries (Figure 3A).22,23,33,46,56,62,65,69 Two-thirds of these publications were published between 2015–2020. Of the observational studies, nine (20%) publications focused on psychiatric issues; specifically, they focused on lethal means counseling and access to firearms among patients presenting with suicidal ideation.10,11,25,26,37,38,45,50,63 Twenty-four publications attempted to characterize firearm violence, studying the prevalence of firearm access (2%)51 and injuries (15%),24,27,41,44,48,57,68 behavioral risk factors for firearm violence (11%),9,12,13,31,42 characteristics of patients presenting for firearm injuries (24%),14,17,21,30,36,39,40,52-54,58 and the severity of firearm injuries (4%).34,35 Two studies (4%) looked into developing screening tools to predict future risk of firearm violence,22,31 and five (11%) assessed patient and provider attitudes toward asking about firearm access and safety in the ED.19,20,45,47,50 Forty-two percent of publications focused on pediatric ED patients. A plurality of interventional studies (43%) focused on lethal means counseling.38,55,66
Child Abuse
We identified 114 relevant publications: 71 observational studies70-141; 12 interventional studies142-153; three review publications154-156; and 28 commentary publications (Figure 3B).157-184 There were several common objectives among the observational studies. Twenty-two (31%) observational publications focused on determining incidence/prevalence of child abuse in different settings (single EDs, specific geographic areas, nationwide), and characterizing cases of child abuse.70,76,82,83,88,93,95,97,98,102,113,116,119,120,124,125,127,129,131,132,136,138 Child abuse cases were often categorized by demographic characteristics, such as age, gender, race, and insurance status, as well as injury patterns. Nineteen (26%) studies focused specifically on injury patterns of abused children, and the likelihood of child abuse among patients presenting with fractures, head trauma, and oral injuries.71,75,81,82,86,91,95,97,99,101,107,109-111,113,115,117,119,127 About 22 (31%) studies focused specifically on child sexual assault cases,70,79,80,96,98,106,112,116,118,120,123,125,130,132,133,141 with six of these studies looking at sexually transmitted infection (STI) and pregnancy testing, STI prophylaxis, and the use of sexual assault nurse examiners.77,78,121,122,140,150 Two of three review publications focused on screening,154,155 with one publication focusing on improving the ED workflow for suspected or confirmed child abuse cases.156
Other common study objectives included examining and amending the ED workflow for child abuse cases, developing screening protocols, and understanding provider knowledge and training with regard to child abuse in the ED. A plurality (42%) of the interventional studies involved evaluations of educational interventions for ED providers meant to improve child abuse screening and recognition.142,144,147,149,152 Three (25%) interventional studies focused on child sexual assault.142,144,150
Elder Abuse
We identified 31 relevant publications: 16 observational studies185-215; three review publications187,212,214; and 12 commentary publications.185,186,192,195,197,198,200,201,205,210,211,215 Common objectives among the observational studies included the following: developing and testing screening tools (N = 5, 31%)194,196,202,204,206; ED utilization by abused patients (N = 2, 13%)190,207; injury patterns among abused patients (13%)191,208,213; patient characteristics (N = 2, 13%)202,209; provider awareness and perspectives on elder abuse (N = 2, 13%)188,203; and prevalence of elder abuse (N = 1, 6%).189 There was a lack of interventional studies regarding educational interventions or the use of screening tools. All 12 commentary publications from the 1990s to 2019 served to raise awareness about elder abuse in the ED and ways to identify and combat it.
Intimate Partner Violence
We identified 120 relevant publications: 78 observational studies216-293; 16 interventional studies294-309; 11 review publications310-320 ; and 15 commentary publications (Figure 3C).321-335 The most prevalent objectives among original research studies were intimate partner violence (IPV) screening (N = 20, 26%)218,226,229,230,237,240,242,245,246,258,259,261,264,270,273,278,281,293,300,306; characteristics and risk factors (N = 15, 19%)220,221,223,227,228,231,233,242,247,249,262,263,279,284,292; substance use and mental health associations (N = 14, 18%)216,217,224,225,228,238,239,241,250,255,268,282,283,302; prevalence of IPV (N = 12, 15%)219,221,222,236,242,245,257,263,271,276,284,286; provider perspectives on IPV screening and protocols (N = 8, 10%)232,235,251,252,254,256,265,267; and patient perspectives on the acceptability of IPV screening and discussion in the ED (N=9, 12%).242,243,252,265,267,269,272,277,289 Five studies focused specifically on IPV screening for caregivers of pediatric patients (6%).242,248,266,298,303 There were also three studies focused on perpetrators of IPV.234,253,290
Of the 16 interventional studies, nine (56%) were related to screening,294,296-298,300,303,304,306,308 three (19%) were related to addressing substance use among patients with co-existing IPV,299,302,307 and two (13%) were educational interventions for ED staff.303,309
Human Trafficking
We identified 19 relevant publications: four interventional studies336-339; seven observational studies79,340-345; one systematic review346; and seven commentary publications.347-353 All publications were published after 2012. Of the seven observational studies, three (43%) related to screening tools to identify patients experiencing sex trafficking.340,342,344 Two (25%) focused on patient characteristics,79,345 one was a case report (13%),343 and the other study focused on emergency nurses’ perspectives (13%).341 All four interventional studies looked at the efficacy of educational modules on ED staff in better understanding the issue of human trafficking in the ED and being better able to identify human trafficking victims in the ED. The systematic review was of existing human trafficking screening tools in the ED. Seven studies (37%) focused specifically on child sex trafficking victims in the ED.340,344-346,352,353
Lesbian, Gay, Bisexual, Transgender, and Queer Health
We identified 22 relevant publications: 14 observational studies354-367; one interventional study368; and seven369-375 commentary publications. Of these, 21 (95%) were published after 2014. Of the observational studies, five (36%) focused on patient provider attitudes toward sexual orientation and gender identity data collection in the ED,354,355,361,362,365 and six (43%) focused on the care of transgender patients in the ED,356,358-360,367,370 with many surveying experiences of discrimination among transgender patients.358,360,363,367 Four (29%) observational publications focused on LGBTQ health competency training by emergency care providers.356,364,366,368,373 One (7%) publication broke down intimate partner violence prevalence in the ED by the sexual orientation of patients.357 The commentary publications centered on the same themes.
The single interventional publication used pre/post data to evaluate the efficacy of an ED competency training in LGBTQ health.368
Immigration
We identified 24 relevant publications:376-399 20 observational studies376-395; one interventional study399; and three commentary publications.396-398 All observational publications investigated ED utilization in immigrant vs non-immigrant groups, with some specifically assessing Latino populations. Two publications (10%) studied the fear of ED utilization among Latino populations.376,386 The single interventional study assessed a texting-based intervention of Latino families as a means to reduce ED utilization while increasing well-care and vaccine adherence.399
Incarceration
We identified 11 relevant publications: eight observational studies400-407; two interventional studies408,409; and one commentary publication.410 Of the observational studies, five (63%) publications centered on ED utilization after release from prison.400,403-405,407 Both interventional publications focused on models of care for recently released prisoners. Of all publications, three (38%) focused on pediatric populations.401,402,404
Language
We identified 32 relevant publications 411-442; 26 observational studies411-436; three interventional studies437-439; one review publication; and two commentary publications. The observational research spanned a broad range of topic areas covering many parts of ED care, including triage (8%),419,438 history of present illness collection (4%),416 management of care (4%),411 interpreter utilization and need (12%),415,428,429 ED resource utilization (15%),423,424,431,433 length of stay (8%),427,430 the discharge process (15%),417,420-422 and follow-up care (8%).432,435 Of the interventional studies, one examined the role of the patient’s preferred language in the success of a drinking intervention.437 Another looked at the efficacy and efficiency of a bilingual, kiosk-based self-triage system compared to a nurse.438 The third publication investigated the effectiveness of a bilingual medical history questionnaire.439 The review and commentary pieces described the language barriers patients face in the ED440 and utilization of interpreter services.441,442 Of all publications, 12 (38%) focused on pediatric populations.411,417,420-422,425-427,430,431,433,438
Literacy
We identified 34 relevant publications443-475: 25 observational studies443-466; four interventional studies467-470; three review publications473-475; and two commentary publications.471,472 Of the observational studies, 11 (41%) examined health literacy screening and patients’ understanding of discharge instructions,443,445,451-453,461-463,466,474,476 eight (30%) investigated the relationship between health literacy and ED utilization,447,448,455,457,458,460,469,473 and 10 (37%) focused on the literacy of the parents of pediatric patients.446,448,454,457,458,467-469,473,475 One study focused on ways to improve a patient’s understanding of the clinical encounter with improved communication tools for physicians or teach-back strategies with patients.450 All four of the interventional studies involved educational interventions for parents of pediatric patients.467-470
Housing/Homelessness
We identified 73 relevant publications4,477-548: 61 observational studies4,477-536; five interventional studies537-541; six commentary publications,542-547; and one review publication (Figure 3D).548 Twenty-eight (46%) observational studies focused on ED utilization, including factors predicting ED utilization and characteristics of homeless patients that frequently used the ED.4,478,479,487,492,499,501-503,505-508,510,511,513,514,519,521,524,527-533 Another common study objective (16%) included the effect of substance use and mental illness on ED utilization of homeless patients.480,484,488,493,494,500,509,526,535,539 Four (7%) observational studies looked into ED provider perspectives,515,520,523 and two looked into homeless patient perspectives on ED services.482,483 A few studies focused on specific sub-populations of homeless patients, including veterans,492,519,524,528 older adults,499,501 and pediatric patients.485,486,507,534 Two (40%) interventional studies centered on analyzing the effect of case management interventions on ED utilization.537,541
Food Insecurity
We identified 29 relevant publications 25 observational studies549-574; two interventional studies,575,576; and two commentary publications.577,578 Objectives among observational studies included the following: food insecurity prevalence (27%)555,560-562,564,565,567; ED utilization (19%)549,550,552,570,571; screening (8%),553,572; and cost of care (12%).550,559,561 Four (15%) publications explored the health consequences of food insecurity.561,565-567 Five (19%) publications focused the intersection between diabetic patients, food insecurity, and presentation to the ED.552,554,559,563,568 Three publications (12%) also focused specifically on Supplemental Nutrition Assistance Program benefits running out near the end of the month,569 and the impact on patients with diabetes568 and hypertension.556 Nine (35%) observational studies focused on pediatric populations.549,553-555,560,562,566,573,574 One interventional study was a randomized controlled trial of two screening methods,576 and the other was a program to improve access to food for pediatric ED patients.575
Transportation
Two relevant publications were identified,579,580 both of which were observational and published in 2019. One publication compared proximity of freestanding EDs and hospital EDs to public transit in three different metro areas.579 The second discussed ridesharing services as alternative options to ambulances for stable psychiatric patients to reach the emergency department.580
Financial Insecurity
We identified two relevant publications, both of which were observational.581,582 Both publications focused on the financial burden for patients of specific chief complaints in the ED, including atopic dermatitis and orthopedic injuries. One publication looked specifically at the pediatric population.582
Education
Two relevant publications were identified, both of which were observational studies. One publication explored the association between educational attainment and patterns of ED use in patients with sickle cell disease,583 and the other focused on the relationship between educational attainment and likelihood of receiving opioids for pain management in the ED.584
Employment
We identified three relevant publications: two observational studies585,586; and one systematic review.587 The systematic review broadly examined social and demographic characteristics influencing ED use, and included unemployment as one of many variables. Of the observational studies, one correlated unemployment rates and trauma admissions in New Orleans,586 and the other correlated ED visits with areas experiencing “economic hazard,” which included unemployment rate.585
Social Determinants of Health (SDOH)
We identified seven relevant publications3,6,555,588-593: five observational studies3,588-590,593; one review publication6; and one commentary publication.592 There were no interventional studies. Three (60%) of the observational publications focused on the SDOH of specific populations – dialysis patients,588 patients with sickle cell disease,589 and patients who inject intravenous drugs593 – and the relationship with ED utilization. Another publication focused on predicting ED visits using SDOH measures.590 Two publications (29%) focused on pediatric populations.555,590
Social Emergency Medicine Training
A total of three relevant publications were identified: one educational intervention594; and two commentary publications.591,595 The education intervention assessed the impact of a longitudinal curriculum for fourth-year medical students on their EM clerkship rotation.594 The commentary publications discussed the incorporation of SDOH into various aspects of EM training.
DISCUSSION
We identified 590 publications in 18 categories relevant to social EM, demonstrating a high degree of interest in social EM topics. Despite the large and growing number of relevant publications across categories, only 58 publications (10%) were interventional studies. In most topic areas, observational studies have already done a thorough job of describing and characterizing disparities by social identity and circumstance. For example, while a large number of studies looked at ways to effectively screen patients for things like interpersonal violence, health literacy, and human trafficking, there were few publications following up on outcomes for patients who screened positive. Even fewer interventional studies examined patient-oriented outcomes; most interventional studies were educational in nature, with outcomes such as clinician awareness and effectiveness of screening. The dearth of interventional studies examining patient outcomes underscores a need for funding to support testing and dissemination of potential interventions, given that observational studies are more feasible and less resource-intensive than interventional studies.
Topics with the most published research included gun violence, child abuse, intimate partner violence, and housing/homelessness; these four categories combined constituted 63% of all relevant publications. There were several topic areas in which the literature base has grown rapidly in recent years, including gun violence and LGBTQ health. Topics such as elder abuse and incarceration have been the topic of few publications in the last five years, suggesting possible stagnation in these areas. About one third of the relevant publications included were related to the pediatric ED. We found very little research in the following eight topic areas: transportation, financial insecurity, education, employment, incarceration, racism, and legal needs, possibly because they may have been traditionally perceived as less directly related to clinical care and may thus have received less attention.
Prior literature has examined the scope of EM research focused on material needs; our study also examines non-material social risk factors for health outcomes. While the acknowledgment of the interplay between social factors and patients’ acute health care needs and outcomes has existed in medical literature for decades, terminology such as “social emergency medicine” is more recent and has increased following a consensus conference about the field.7
LIMITATIONS
There were several limitations to our review. First, we largely used only the PubMed database, which may have left out relevant publications; however, we systematically searched PubMed, and a majority of biomedical publications are indexed in PubMed. All our search terms were specific to EM, which may have also left out research relevant to EM conducted in related settings or fields. We limited our search to “title only” rather than “title and abstract,” which may have also omitted relevant publications; however, after attempting both “title only” and “title and abstract” searches, we found “title only” searches to have much higher relevance. We also did not conduct a detailed analysis of publication quality, given that we set out to complete a scoping review rather than a systematic review; however, publication quality would have been difficult to assess across the diversity of topic areas given the vast array of topics and study designs. We maximized reliability by using two independent reviewers for each topic area, with a third reviewer who reconciled any differences in opinion regarding relevance or publication inclusion.
CONCLUSION
Social emergency medicine research has accelerated in recent years. Numerous observational studies and commentary publications have defined and characterized problems relevant to social EM, and several educational interventions have demonstrated ways to improve provider awareness of different social EM topics. However, based on our review, there is a dearth of social EM research focused on patient-centered interventions. A consensus-driven research agenda should be pursued to accelerate patient-centered interventions aimed at social factors that influence acute healthcare and outcomes.
Footnotes
Section Editor: Tony Zitek, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Michelle P. Lin, MD, MPH, MS, Icahn School of Medicine at Mount Sinai, Department of Emergency Medicine, 1 Gustave L. Levy Place Box 1620, New York, NY, 10029. Email: michelle.lin@mountsinai.org. 11 / 2021; 22:1360 – 1368
Submission history: Revision received January 7, 2021; Submitted April 12, 2021; Accepted April 14, 2021
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. MPL received funding from the National Heart, Lung, Blood Institute of the National Institutes of Health under award number K23 HL143042. There are no conflicts of interest.
REFERENCES
1. Virchow RC. Report on the typhus epidemic in Upper Silesia. 1848. American journal of public health. 2006;96(12):2102-2105.
2. Lee PR. The future of social medicine. J Urban Health. 1999;76(2):229-236.
3. Anderson ES, Hsieh D, Alter HJ. Social Emergency Medicine: Embracing the Dual Role of the Emergency Department in Acute Care and Population Health. Ann Emerg Med. 2016;68(1):21-25.
4. Rodriguez RM, Fortman J, Chee C, et al. Food, shelter and safety needs motivating homeless persons’ visits to an urban emergency department. Annals of emergency medicine. 2009;53(5):598-602.
5. Fahimi J, Goldfrank L. Principles of Social Emergency Medicine. Annals of emergency medicine. 2019;74(5S):S6-S10.
6. Malecha PW, Williams JH, Kunzler NM, et al. Material Needs of Emergency Department Patients: A Systematic Review. Acad Emerg Med. 2018;25(3):330-359.
7. Gottlieb LM, Wing H, Adler NE. A Systematic Review of Interventions on Patients’ Social and Economic Needs. Am J Prev Med. 2017;53(5):719-729.
8. Jones M, Kistamgari S, Smith GA. Nonpowder Firearm Injuries to Children Treated in Emergency Departments. Pediatrics. 2019;144(6).
9. Carter PM, Mouch CA, Goldstick JE, et al. Rates and correlates of risky firearm behaviors among adolescents and young adults treated in an urban emergency department. Preventive medicine. 2020;130:105891.
10. Katz C, Bhaskaran J, Bolton JM. Access to Firearms Among People Assessed by Psychiatric Services in the Emergency Department. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2019;64(11):770-776.
11. Naganathan S, Mueller KL. Physician Documentation of Access to Firearms in Suicidal Patients in the Emergency Department. The western journal of emergency medicine. 2019;20(5):818-821.
12. Goldstick JE, Carter PM, Heinze JE, et al. Predictors of transitions in firearm assault behavior among drug-using youth presenting to an urban emergency department. J Behav Med. 2019;42(4):635-645.
13. Abaya R, Atte T, Herres J, et al. Characteristics and behavioral risk factors of firearm-exposed youth in an urban emergency department. J Behav Med. 2019;42(4):603-612.
14. Cutler GJ, Zagel AL, Spaulding AB, et al. Emergency Department Visits for Pediatric Firearm Injuries by Trauma Center Type. Pediatric emergency care. 2019.
15. Hink AB, Bonne S, Levy M, et al. Firearm injury research and epidemiology: A review of the data, their limitations, and how trauma centers can improve firearm injury research. The journal of trauma and acute care surgery. 2019;87(3):678-689.
16. Patel SJ, Badolato GM, Parikh K, et al. Regional Differences in Pediatric Firearm-Related Emergency Department Visits and the Association With Firearm Legislation. Pediatric emergency care. 2019.
17. Coupet E, Huang Y, Delgado MK. US Emergency Department Encounters for Firearm Injuries According to Presentation at Trauma vs Nontrauma Centers. JAMA Surg. 2019;154(4):360-362.
18. Betz ME, Bebarta VS, DeWispelaere W, et al. Emergency Physicians and Firearms: Effects of Hands-on Training. Annals of emergency medicine. 2019;73(2):210-211.
19. Boge LA, Dos Santos C, Burkholder JD, et al. Patients’ Perceptions of the Role of Physicians in Questioning and Educating in Firearms Safety: Post-FOPA Repeal Era. South Med J. 2019;112(1):34-38.
20. Wolf LA, Delao AM, Perhats C, et al. Emergency Nurses’ Perceptions of Risk for Firearm Injury and its Effect on Assessment Practices: A Mixed Methods Study. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2019;45(1):54-66.e52.
21. de Anda H, Dibble T, Schlaepfer C, et al. A Cross-Sectional Study of Firearm Injuries in Emergency Department Patients. Mo Med. 2018;115(5):456-462.
22. Assessing Risk for Future Firearms Violence in Young People Who Present to ED. ED management : the monthly update on emergency department management. 2017;29(6):65-66.
23. Scarlet S, Rogers SO. What Is the Institutional Duty of Trauma Systems to Respond to Gun Violence?. AMA J Ethics. 2018;20(5):483-491.
24. Jiang Y, Ranney ML, Sullivan B, et al. Can Statewide Emergency Department, Hospital Discharge, and Violent Death Reporting System Data Be Used to Monitor Burden of Firearm-Related Injury and Death in Rhode Island?. J Public Health Manag Pract. 2019;25(2):137-146.
25. Runyan CW, Brooks-Russell A, Tung G, et al. Hospital Emergency Department Lethal Means Counseling for Suicidal Patients. Am J Prev Med. 2018;54(2):259-265.
26. Betz ME, Kautzman M, Segal DL, et al. Frequency of lethal means assessment among emergency department patients with a positive suicide risk screen. Psychiatry Res. 2018;260:30-35.
27. Gani F, Sakran JV, Canner JK. Emergency Department Visits For Firearm-Related Injuries In The United States, 2006–14. Health Aff (Millwood). 2017;36(10):1729-1738.
28. Carter PM, Walton MA, Goldstick J, et al. Violent firearm-related conflicts among high-risk youth: An event-level and daily calendar analysis. Preventive medicine. 2017;102:112-119.
29. Freeman JJ, Bachier-Rodriguez M, Staszak J, Feliz A. A comparison between non-powder gun and powder-gun injuries in a young pediatric population. Injury. 2017;48(9):1951-1955.
30. Carter PM, Cook LJ, Macy ML, et al. Individual and Neighborhood Characteristics of Children Seeking Emergency Department Care for Firearm Injuries Within the PECARN Network. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2017;24(7):803-813.
31. Goldstick JE, Carter PM, Walton MA, et al. Development of the SaFETy Score: A Clinical Screening Tool for Predicting Future Firearm Violence Risk. Ann Intern Med. 2017;166(10):707-714.
32. Lale A, Krajewski A, Friedman LS. Undertriage of Firearm-Related Injuries in a Major Metropolitan Area. JAMA Surg. 2017;152(5):467-474.
33. Ranney ML, Fletcher J, Alter H, et al. A Consensus-Driven Agenda for Emergency Medicine Firearm Injury Prevention Research. Annals of emergency medicine. 2017;69(2):227-240.
34. Feldman KA, Tashiro J, Allen CJ, et al. Predictors of mortality in pediatric urban firearm injuries. Pediatr Surg Int. 2017;33(1):53-58.
35. Sauaia A, Gonzalez E, Moore HB, et al. Fatality and Severity of Firearm Injuries in a Denver Trauma Center, 2000–2013. Jama. 2016;315(22):2465-2467.
36. Monuteaux MC, Mannix R, Fleegler EW, et al. Predictors and Outcomes of Pediatric Firearm Injuries Treated in the Emergency Department: Differences by Mechanism of Intent. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2016;23(7):790-795.
37. Betz ME, Miller M, Barber C, et al. Lethal Means Access and Assessment among Suicidal Emergency Department Patients. Depress Anxiety. 2016;33(6):502-511.
38. Runyan CW, Becker A, Brandspigel S, et al. Lethal Means Counseling for Parents of Youth Seeking Emergency Care for Suicidality. The western journal of emergency medicine. 2016;17(1):8-14.
39. Russo R, Fury M, Accardo S, et al. Economic and Educational Impact of Firearm-Related Injury on an Urban Trauma Center. Orthopedics. 2016;39(1):e57-61.
40. Fahimi J, Larimer E, Hamud-Ahmed W, et al. Long-term mortality of patients surviving firearm violence. Inj Prev. 2016;22(2):129-134.
41. Williams M, Ballard DH, DeLeonardis C, et al. Pediatric unintentional firearm injuries: a Northwestern Louisiana trauma center analysis. The American surgeon. 2015;81(6):653-654.
42. Carter PM, Walton MA, Roehler DR, et al. Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics. 2015;135(5):805-815.
43. Carter PM, Walton MA, Newton MF, et al. Firearm possession among adolescents presenting to an urban emergency department for assault. Pediatrics. 2013;132(2):213-221.
44. Sauaia A, Miller JI, Moore EE, et al. Firearm injuries of children and adolescents in 2 Colorado trauma centers: 2000–2008. Jama. 2013;309(16):1683-1685.
45. Betz ME, Miller M, Barber C, et al. Lethal means restriction for suicide prevention: beliefs and behaviors of emergency department providers. Depress Anxiety. 2013;30(10):1013-1020.
46. Ranney ML, Sankoff J, Newman DH, et al. A call to action: firearms, public health, and emergency medicine. Annals of emergency medicine. 2013;61(6):700-702.
47. Price JH, Thompson A, Khubchandani J, et al. Perceived roles of Emergency Department physicians regarding anticipatory guidance on firearm safety. The Journal of emergency medicine. 2013;44(5):1007-1016.
48. Allareddy V, Nalliah RP, Rampa S, et al. Firearm related injuries amongst children: estimates from the nationwide emergency department sample. Injury. 2012;43(12):2051-2054.
49. Pelucio M, Roe G, Fiechtl J, et al. Assessing survey methods and firearm exposure among adolescent emergency department patients. Pediatric emergency care. 2011;27(6):500-506.
50. Betz ME, Barber CW, Miller M. Firearm restriction as suicide prevention: variation in belief and practice among providers in an urban emergency department. Inj Prev. 2010;16(4):278-281.
51. Loh K, Walton MA, Harrison SR, et al. Prevalence and correlates of handgun access among adolescents seeking care in an urban emergency department. Accid Anal Prev. 2010;42(2):347-353.
52. Wiebe DJ. Sex differences in the perpetrator-victim relationship among emergency department patients presenting with nonfatal firearm-related injuries. Annals of emergency medicine. 2003;42(3):405-412.
53. Cherry D, Annest JL, Mercy JA, et al. Trends in nonfatal and fatal firearm-related injury rates in the United States, 1985–1995. Annals of emergency medicine. 1998;32(1):51-59.
54. Cummings P, LeMier M, Keck DB. Trends in firearm-related injuries in Washington State, 1989–1995. Annals of emergency medicine. 1998;32(1):37-43.
55. Fendrich M, Kruesi MJ, Wislar JS, et al. Implementing means restriction education in urban EDs. The American journal of emergency medicine. 1998;16(3):257-261.
56. ED physicians take action to promote firearm safety, curtail gun violence. ED management : the monthly update on emergency department management. 1998;10(5):57-60.
57. Coben JH, Dearwater SR, Forjuoh SN, et al. A population-based study of fatal and nonfatal firearm-related injuries. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1997;4(4):248-255.
58. Ary RD, Waldrop RD, Harper DE. The increasing burden of pediatric firearm injuries on the emergency department. Pediatric emergency care. 1996;12(6):391-393.
59. Coben JH, Dearwater SR, Garrison HG, et al. Evaluation of the emergency department logbook for population-based surveillance of firearm-related injury. Annals of emergency medicine. 1996;28(2):188-193.
60. Carter PM, Walton MA, Zimmerman MA, et al. Efficacy of a Universal Brief Intervention for Violence Among Urban Emergency Department Youth. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2016;23(9):1061-1070.
61. Beard JH, Resnick S, Maher Z, et al. Clustered Arrivals of Firearm-Injured Patients in an Urban Trauma System: A Silent Epidemic. J Am Coll Surg. 2019;229(3):236-243.
62. Flaherty MR, Klig JE. Firearm-related injuries in children and adolescents: an emergency and critical care perspective. Curr Opin Pediatr. 2020;32(3):349-353.
63. Diurba S, Johnson RL, Siry BJ, et al. Lethal Means Assessment and Counseling in the Emergency Department: Differences by Provider Type and Personal Home Firearms. Suicide Life Threat Behav. 2020.
64. Richmond TS, Schwab CW, Riely J, Branas CC, et al. Effective trauma center partnerships to address firearm injury: a new paradigm. The Journal of trauma. 2004;56(6):1197-1205.
65. Ranney ML, Betz ME, Dark C. #ThisIsOurLane – Firearm Safety as Health Care’s Highway. N Engl J Med. 2019;380(5):405-407.
66. Miller M, Salhi C, Barber C, et al. Changes in Firearm and Medication Storage Practices in Homes of Youths at Risk for Suicide: Results of the SAFETY Study, a Clustered, Emergency Department-Based, Multisite, Stepped-Wedge Trial. Annals of emergency medicine. 2020;76(2):194-205.
67. Stempniak M. HANDLING WITH CARE. New approach treats victims of gun violence like substance abusers. Hosp Health Netw. 2015;89(11):19.
68. Annest JL, Mercy JA, Gibson DR, et al. National estimates of nonfatal firearm-related injuries. Beyond the tip of the iceberg. Jama. 1995;273(22):1749-1754.
69. Richmond TS, Branas CC, Schwab CW. Trauma center-community partnerships to address firearm injury: it can be done. LDI Issue Brief. 2004;10(1):1-4.
70. Bentivegna K, Durante A, Livingston N, et al. Child Sexual Abuse identified in Emergency Departments Using ICD-9-CM, 2011 to 2014. The Journal of emergency medicine. 2019;56(6):719-726.
71. Lavin LR, Penrod CH, Estrada CM, et al. Fractures in the Pediatric Emergency Department: Are We Considering Abuse?. Clinical pediatrics. 2018;57(10):1161-1167.
72. Tiyyagura G, Gawel M, Koziel JR, et al. Barriers and Facilitators to Detecting Child Abuse and Neglect in General Emergency Departments. Annals of emergency medicine. 2015;66(5):447-454.
73. Henry MK, Wood JN, Metzger KB, et al. Relationship between Insurance Type and Discharge Disposition From the Emergency Department of Young Children Diagnosed with Physical Abuse. The Journal of pediatrics. 2016;177:302-307.e301.
74. Wheeler KK, Shi J, Xiang H, et al. Child maltreatment in U.S. emergency departments: Imaging and admissions. Child abuse & neglect. 2017;69:96-105.
75. Kondis JS, Muenzer J, Luhmann JD. Missed Fractures in Infants Presenting to the Emergency Department With Fussiness. Pediatric emergency care. 2017;33(8):538-543.
76. Blatz AM, Gillespie CW, Katcher A, et al. Factors Associated With Nonaccidental Trauma Evaluation Among Patients Below 36 Months Old Presenting With Femur Fractures at a Level-1 Pediatric Trauma Center. Journal of pediatric orthopedics. 2019;39(4):175-180.
77. Deutsch SA, Benyo S, Xie S, et al. Addressing Human Papillomavirus Prevention During Pediatric Acute Sexual Assault Care. Journal of forensic nursing. 2018;14(3):154-161.
78. Schilling S, Samuels-Kalow M, Gerber JS, et al. Testing and Treatment After Adolescent Sexual Assault in Pediatric Emergency Departments. Pediatrics. 2015;136(6):e1495-1503.
79. Hornor G, Sherfield J. Commercial Sexual Exploitation of Children: Health Care Use and Case Characteristics. Journal of pediatric health care : official publication of National Association of Pediatric Nurse Associates & Practitioners. 2018;32(3):250-262.
80. Hassan M, Gary FA, Hotz R, et al. Young Victims Telling their Stories of Sexual Abuse in the Emergency Department. Issues in mental health nursing. 2015;36(12):944-952.
81. Yu YR, DeMello AS, Greeley CS, et al. Injury patterns of child abuse: Experience of two Level 1 pediatric trauma centers. Journal of pediatric surgery. 2018;53(5):1028-1032.
82. Tiyyagura G, Christian C, Berger R, et al. Occult abusive injuries in children brought for care after intimate partner violence: An exploratory study. Child abuse & neglect. 2018;79:136-143.
83. Hunter AA, Bernstein B. Identification of Child Maltreatment-Related Emergency Department Visits in Connecticut, 2011 to 2014. Clinical pediatrics. 2019;58(9):970-976.
84. Webb T, Valvano T, Nugent M, et al. Child abuse pediatric consults in the pediatric emergency department improve adherence to hospital guidelines. WMJ : official publication of the State Medical Society of Wisconsin. 2013;112(5):206-210.
85. Rhodes AE, Boyle MH, Bethell J, et al. Child maltreatment and onset of emergency department presentations for suicide-related behaviors. Child abuse & neglect. 2012;36(6):542-551.
86. Woolf SM, Leventhal JM, Gaither JR, et al. Oral injuries in children less than 24 months of age in a pediatric emergency department. Child abuse & neglect. 2019;89:70-77.
87. Somji Z, Plint A, McGahern C, et al. Diagnostic coding of abuse related fractures at two children’s emergency departments. Child abuse & neglect. 2011;35(11):905-914.
88. Pless IB, Sibald AD, Smith MA, et al. A reappraisal of the frequency of child abuse seen in pediatric emergency rooms. Child abuse & neglect. 1987;11(2):193-200.
89. Choo EK, Spiro DM, Lowe RA, et al. Rural-urban disparities in child abuse management resources in the emergency department. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2010;26(4):361-365.
90. Starling SP, Heisler KW, Paulson JF, et al. Child abuse training and knowledge: a national survey of emergency medicine, family medicine, and pediatric residents and program directors. Pediatrics. 2009;123(4):e595-602.
91. Shaikh H, Wrotniak BH, Mazur PM. Occult Head Injury in Children Less Than 2 Years With Suspected Child Abuse in the Emergency Department. Pediatric emergency care. 2019;35(9):596-599.
92. Roberts YH, Huang CY, Crusto CA, et al. Health, emergency department use, and early identification of young children exposed to trauma. The Journal of emergency medicine. 2014;46(5):719-724.
93. King AJ, Farst KJ, Jaeger MW, et al. Maltreatment-Related Emergency Department Visits Among Children 0 to 3 Years Old in the United States. Child maltreatment. 2015;20(3):151-161.
94. Spivey MI, Schnitzer PG, Kruse RL, et al. Association of injury visits in children and child maltreatment reports. The Journal of emergency medicine. 2009;36(2):207-214.
95. Keshavarz R, Kawashima R, Low C. Child abuse and neglect presentations to a pediatric emergency department. The Journal of emergency medicine. 2002;23(4):341-345.
96. Floyed RL, Hirsh DA, Greenbaum VJ, et al. Development of a screening tool for pediatric sexual assault may reduce emergency-department visits. Pediatrics. 2011;128(2):221-226.
97. Pandya NK, Baldwin K, Wolfgruber H, et al. Child abuse and orthopaedic injury patterns: analysis at a level I pediatric trauma center. Journal of pediatric orthopedics. 2009;29(6):618-625.
98. Hassan M, Killion C, Lewin L, et al. Gender-related sexual abuse experiences reported by children who were examined in an emergency department. Archives of psychiatric nursing. 2015;29(3):148-154.
99. Oral R, Blum KL, Johnson C. Fractures in young children: are physicians in the emergency department and orthopedic clinics adequately screening for possible abuse?. Pediatric emergency care. 2003;19(3):148-153.
100. Peterson C, Xu L, Florence C, et al. Annual Cost of U.S. Hospital Visits for Pediatric Abusive Head Trauma. Child maltreatment. 2015;20(3):162-169.
101. Allareddy V, Asad R, Lee MK, et al. Hospital based emergency department visits attributed to child physical abuse in United States: predictors of in-hospital mortality. PloS one. 2014;9(2):e100110.
102. Bogumil DDA, Demeter NE, Kay Imagawa K, et al. Prevalence of nonaccidental trauma among children at American College of Surgeons-verified pediatric trauma centers. The journal of trauma and acute care surgery. 2017;83(5):862-866.
103. Wright RJ, Wright RO, Farnan L, et al. Response to child abuse in the pediatric emergency department: need for continued education. Pediatric emergency care. 1999;15(6):376-382.
104. Guenther E, Knight S, Olson LM, et al. Prediction of child abuse risk from emergency department use. The Journal of pediatrics. 2009;154(2):272-277.
105. Rhodes AE, Boyle MH, Bethell J, et al. Child maltreatment and repeat presentations to the emergency department for suicide-related behaviors. Child abuse & neglect. 2013;37(2–3):139-149.
106. Makoroff KL, Brauley JL, Brandner AM, et al. Genital examinations for alleged sexual abuse of prepubertal girls: findings by pediatric emergency medicine physicians compared with child abuse trained physicians. Child abuse & neglect. 2002;26(12):1235-1242.
107. Pierce MC, Magana JN, Kaczor K, et al. The Prevalence of Bruising Among Infants in Pediatric Emergency Departments. Annals of emergency medicine. 2016;67(1):1-8.
108. MacNeill EC, Cabey W, Kluge R, et al. Emergency Department Utilization in Children <36 Months Is Not an Independent Risk Factor for Maltreatment. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2016;23(11):1228-1234.
109. Hicks RA, Stolfi A. Skeletal surveys in children with burns caused by child abuse. Pediatric emergency care. 2007;23(5):308-313.
110. Ward A, Iocono JA, Brown S, et al. Non-accidental Trauma Injury Patterns and Outcomes: A Single Institutional Experience. The American surgeon. 2015;81(9):835-838.
111. Son-Hing JP, Deniz Olgun Z. The frequency of nonaccidental trauma in children under the age of 3 years with femur fractures: is there a better cutoff point for universal workups?. Journal of pediatric orthopedics Part B. 2018;27(4):366-368.
112. Gordon S, Jaudes PK. Sexual abuse evaluations in the emergency department: is the history reliable?. Child abuse & neglect. 1996;20(4):315-322.
113. Chang DC, Knight V, Ziegfeld S, et al. The tip of the iceberg for child abuse: the critical roles of the pediatric trauma service and its registry. The Journal of trauma. 2004;57(6):1189-1198.
114. Johnson CF, Apolo J, Joseph JA, et al. Child abuse diagnosis and the emergency department chart. Pediatric emergency care. 1986;2(1):6-9.
115. Hodge D, Ludwig S. Child homicide: emergency department recognition. Pediatric emergency care. 1985;1(1):3-6.
116. Goyal MK, Mollen CJ, Hayes KL, et al. Enhancing the emergency department approach to pediatric sexual assault care: implementation of a pediatric sexual assault response team program. Pediatric emergency care. 2013;29(9):969-973.
117. Leeper CM, Nasr I, McKenna C, et al. Elevated admission international normalized ratio strongly predicts mortality in victims of abusive head trauma. The journal of trauma and acute care surgery. 2016;80(5):711-716.
118. Kivlahan C, Kruse R, Furnell D. Sexual assault examinations in children. The role of a statewide network of health care providers. American journal of diseases of children (1960). 1992;146(11):1365-1370.
119. Xiang J, Shi J, Wheeler KK, et al. Paediatric patients with abusive head trauma treated in US Emergency Departments, 2006–2009. Brain injury. 2013;27(13–14):1555-1561.
120. Seidel JS, Elvik SL, Berkowitz CD, et al. Presentation and evaluation of sexual misuse in the emergency department. Pediatric emergency care. 1986;2(3):157-164.
121. Fajman N, Wright R. Use of antiretroviral HIV post-exposure prophylaxis in sexually abused children and adolescents treated in an inner-city pediatric emergency department. Child abuse & neglect. 2006;30(8):919-927.
122. Bechtel K, Ryan E, Gallagher D. Impact of sexual assault nurse examiners on the evaluation of sexual assault in a pediatric emergency department. Pediatric emergency care. 2008;24(7):442-447.
123. Kupfer GM, Giardino AP. Reimbursement and insurance coverage in cases of suspected sexual abuse in the emergency department. Child abuse & neglect. 1995;19(3):291-295.
124. Saluja G, Marquez V, Cheng TL, et al. Adolescents as victims of familial violence: a hospital based surveillance. International journal of injury control and safety promotion. 2007;14(1):19-23.
125. Shah CP, Holloway CP, Valkil DV. Sexual abuse of children. Annals of emergency medicine. 1982;11(1):18-23.
126. Segal UA, Schwartz S. Factors affecting placement decisions of children following short-term emergency care. Child abuse & neglect. 1985;9(4):543-548.
127. Huang MI, O’Riordan MA, Fitzenrider E, et al. Increased incidence of nonaccidental head trauma in infants associated with the economic recession. Journal of neurosurgery Pediatrics. 2011;8(2):171-176.
128. Friedman SB, Morse CW. Child abuse: a five-year follow-up of early case finding in the emergency department. Pediatrics. 1974;54(4):404-410.
129. Roaten JB, Partrick DA, Nydam TL, et al. Nonaccidental trauma is a major cause of morbidity and mortality among patients at a regional level 1 pediatric trauma center. Journal of pediatric surgery. 2006;41(12):2013-2015.
130. Orr DP. Limitations of emergency room evaluations of sexually abused children. American journal of diseases of children (1960). 1978;132(9):873-875.
131. Holter JC, Friedman SB. Child abuse: early case finding in the emergency department. Pediatrics. 1968;42(1):128-138.
132. Merchant RC, Kelly ET, Mayer KH, et al. Trends of visits to Rhode Island Emergency Departments for Pediatric Sexual Exposures, 1995–2001. Medicine and health, Rhode Island. 2008;91(1):15-19.
133. Orr DP, Prietto SV. Emergency management of sexually abused children. The role of the pediatric resident. American journal of diseases of children (1960). 1979;133(6):628-631.
134. Flannery DD, Stephens CL, Thompson AD. The Impact of High-Profile Sexual Abuse Cases in the Media on a Pediatric Emergency Department. Journal of child sexual abuse. 2016;25(6):627-635.
135. Loiselle JM, Westle RE. Inpatient reports of suspected child abuse or neglect (SCAN): a question of missed opportunities in the acute care setting. Pediatric emergency care. 1999;15(2):90-94.
136. Buehner M, Aden J, Borgman M, et al. A Pediatric Application of the STRAC Regional Hospital Trauma Registry Database: Pediatric Trauma Deaths in South Central Texas During 2004–2013. Texas medicine. 2017;113(1):e1.
137. Shahi N, Phillips R, Meier M, et al. The true cost of child abuse at a level 1 pediatric trauma center. Journal of pediatric surgery. 2020;55(2):335-340.
138. Monuteaux MC, Lee L, Fleegler E. Children injured by violence in the United States: emergency department utilization, 2000–2008. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2012;19(5):535-540.
139. Barnes PD, Robson CD. An unresponsive infant in the emergency room. Seminars in pediatric neurology. 1999;6(3):225-227.
140. Goldenring JM, Hubel P, Ruddy R. Importance of testing for sexually transmitted chlamydial disease in the pediatric emergency room. New York state journal of medicine. 1988;88(3):149-151.
141. Kaplan DM, Moore JL, Hirway P, et al. A Comprehensive Pediatric Acute Sexual Assault Protocol: From Emergency Department to Outpatient Follow-up. Pediatric emergency care. 2018.
142. Hoehn EF, Overmann KM, Fananapazir N, et al. Improving Emergency Department Care for Pediatric Victims of Sexual Abuse. Pediatrics. 2018;142(6).
143. Rumball-Smith J, Fromkin J, Rosenthal B, et al. Implementation of routine electronic health record-based child abuse screening in General Emergency Departments. Child abuse & neglect. 2018;85:58-67.
144. Jordan KS, Steelman SH, Leary M, et al. Pediatric Sexual Abuse: An Interprofessional Approach to Optimizing Emergency Care. Journal of forensic nursing. 2019;15(1):18-25.
145. Riney LC, Frey TM, Fain ET, et al. Standardizing the Evaluation of Nonaccidental Trauma in a Large Pediatric Emergency Department. Pediatrics. 2018;141(1).
146. Powers E, Tiyyagura G, Asnes AG, et al. Early Involvement of the Child Protection Team in the Care of Injured Infants in a Pediatric Emergency Department. The Journal of emergency medicine. 2019;56(6):592-600.
147. Carson SM. Implementation of a Comprehensive Program to Improve Child Physical Abuse Screening and Detection in the Emergency Department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2018;44(6):576-581.
148. Higginbotham N, Lawson KA, Gettig K, et al. Utility of a child abuse screening guideline in an urban pediatric emergency department. The journal of trauma and acute care surgery. 2014;76(3):871-877.
149. Jordan KS, Moore-Nadler M. Children at risk of maltreatment: identification and intervention in the emergency department. Advanced emergency nursing journal. 2014;36(1):97-106.
150. Hornor G, Thackeray J, Scribano P, et al. Pediatric sexual assault nurse examiner care: trace forensic evidence, ano-genital injury, and judicial outcomes. Journal of forensic nursing. 2012;8(3):105-111.
151. Benger JR, Pearce V. Simple intervention to improve detection of child abuse in emergency departments. BMJ (Clinical research ed). 2002;324(7340):780.
152. Guenther E, Olsen C, Keenan H, et al. Randomized prospective study to evaluate child abuse documentation in the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2009;16(3):249-257.
153. Kaye P, Taylor C, Barley K, et al. An emergency department intervention to protect an overlooked group of children at risk of significant harm. Emergency medicine journal : EMJ. 2009;26(6):415-417.
154. Louwers EC, Affourtit MJ, Moll HA, et al. Screening for child abuse at emergency departments: a systematic review. Archives of disease in childhood. 2010;95(3):214-218.
155. Woodman J, Lecky F, Hodes D, et al. Screening injured children for physical abuse or neglect in emergency departments: a systematic review. Child: care, health and development. 2010;36(2):153-164.
156. Newton AS, Zou B, Hamm MP, et al. Improving child protection in the emergency department: a systematic review of professional interventions for health care providers. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2010;17(2):117-125.
157. Jain AM. Emergency department evaluation of child abuse. Emergency medicine clinics of North America. 1999;17(3):575-593.
158. Normandin PA. Hidden Child Abuse Identification in the Emergency Department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2016;42(2):181-182.
159. Leetch AN, Leipsic J, Woolridge DP. Evaluation of child maltreatment in the emergency department setting: an overview for behavioral health providers. Child and adolescent psychiatric clinics of North America. 2015;24(1):41-64.
160. Kini N, Brady WJ, Lazoritz S. Evaluating child sexual abuse in the emergency department: clinical and behavioral indicators. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1996;3(10):966-976.
161. Joint Position Statement: Care of Prepubescent Pediatric Sexual Abuse Patients in the Emergency Care Setting. Journal of forensic nursing. 2017;13(3):150-153.
162. Matkins PP, Jordan KS. Pediatric sexual abuse: emergency department evaluation and management. Advanced emergency nursing journal. 2009;31(2):140-152.
163. Stanley RM, Nigrovic LE. Research priorities for a multi-center child abuse network: Lessons learned from pediatric emergency medicine networks. Child abuse & neglect. 2017;70:414-416.
164. Vo DX, Mitchell KA, Moore EM. Emergency Care of Youth with Social and Environmental Vulnerabilities. Adolescent medicine: state of the art reviews. 2015;26(3):589-618.
165. Bechtel K. Sudden unexpected infant death: differentiating natural from abusive causes in the emergency department. Pediatric emergency care. 2012;28(10):1085-1089.
166. Glick NP, Lating JM, Kotchick B. Child sexual abuse evaluations in an emergency room: an overview and suggestions for a multidisciplinary approach. International journal of emergency mental health. 2004;6(3):111-120.
167. Hyden PW, Gallagher TA. Child abuse intervention in the emergency room. Pediatric clinics of North America. 1992;39(5):1053-1081.
168. Ricci LR. Child sexual abuse: the emergency department response. Annals of emergency medicine. 1986;15(6):711-716.
169. Monk M. Interviewing suspected victims of child maltreatment in the emergency department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1998;24(1):31-34.
170. Leetch AN, Woolridge D. Emergency department evaluation of child abuse. Emergency medicine clinics of North America. 2013;31(3):853-873.
171. Overly FL, Sudikoff SN, Duffy S, et al. Three scenarios to teach difficult discussions in pediatric emergency medicine: sudden infant death, child abuse with domestic violence, and medication error. Simulation in healthcare : journal of the Society for Simulation in Healthcare. 2009;4(2):114-130.
172. Munkel WI. Innocents abused. A pediatric hospital forms a team to care for sexually maltreated children. Health progress (Saint Louis, Mo). 1989;70(7):46-49.
173. Gill FT. Caring for abused children in the emergency department. Holistic nursing practice. 1989;4(1):37-43.
174. Jones JG, Worthington BC. Children presenting with fractures in an emergency room: child abuse?. The Journal of the Arkansas Medical Society. 2013;109(10):212.
175. Williams L. Providing emergency care for an abused minor who is not a patient. Journal of the American Dental Association (1939). 2014;145(2):197-198.
176. Neuman MI, Kellogg ND. Testing and Treating Sexually Assaulted Adolescents: What Are We Waiting For?. Pediatrics. 2015;136(6):e1600-1601.
177. Bliss A. The emergency department: gateway to help for child abuse. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1976;2(1):10.
178. George JE. Battered-child syndrome and the ED nurse. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1975;1(3):11.
179. Mundie GE. Team management of the maltreated child in the emergency room. Pediatric annals. 1984;13(10):771-776.
180. Todriguez-Trias H. Abused or neglected children in the emergency department. Topics in emergency medicine. 1983;4(4):51-56.
181. Gay-Callahan MM. Child abuse. A nightmarish reality. Kentucky hospitals magazine. 1989;6(3):6-7.
182. Wailes J. Non-accidental injury. Nursing mirror. 1983;157(16):20-22.
183. Shaw A. Don’t be so sure it’s child abuse. Medical economics. 1993;70(5):79-80.
184. Weaver BM, McCarthy P. Sexual misuse of children: an emergency department nursing perspective. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1981;7(2):59-62.
185. Rosen T, Stern ME, Elman A, et al. Identifying and Initiating Intervention for Elder Abuse and Neglect in the Emergency Department. Clin Geriatr Med. 2018;34(3):435-451.
186. Russo A, Reginelli A, Pignatiello M, et al. Imaging of Violence Against the Elderly and the Women. Semin Ultrasound CT MR. 2019;40(1):18-24.
187. Mercier E, Nadeau A, Brousseau AA, et al. Elder Abuse in the Out-of-Hospital and Emergency Department Settings: A Scoping Review. Annals of emergency medicine. 2020;75(2):181-191.
188. Rosen T, Stern ME, Mulcare MR, et al. Emergency department provider perspectives on elder abuse and development of a novel ED-based multidisciplinary intervention team. Emergency medicine journal : EMJ. 2018;35(10):600-607.
189. Evans CS, Hunold KM, Rosen T, et al. Diagnosis of Elder Abuse in U.S. Emergency Departments. Journal of the American Geriatrics Society. 2017;65(1):91-97.
190. Dong X, Simon MA. Association between elder abuse and use of ED: findings from the Chicago Health and Aging Project. The American journal of emergency medicine. 2013;31(4):693-698.
191. Rosen T, Bloemen EM, LoFaso VM, et al. Emergency Department Presentations for Injuries in Older Adults Independently Known to be Victims of Elder Abuse. The Journal of emergency medicine. 2016;50(3):518-526.
192. Bond MC, Butler KH. Elder abuse and neglect: definitions, epidemiology, and approaches to emergency department screening. Clin Geriatr Med. 2013;29(1):257-273.
193. Rosen T, Mehta-Naik N, Elman A, et al. Improving Quality of Care in Hospitals for Victims of Elder Mistreatment: Development of the Vulnerable Elder Protection Team. Jt Comm J Qual Patient Saf. 2018;44(3):164-171.
194. Platts-Mills TF, Dayaa JA, Reeve BB, et al. Development of the Emergency Department Senior Abuse Identification (ED Senior AID) tool. J Elder Abuse Negl. 2018;30(4):247-270.
195. Phelan A. Elder abuse in the emergency department. Int Emerg Nurs. 2012;20(4):214-220.
196. Cannell B, Gonzalez JMR, Livingston M, et al. Pilot testing the detection of elder abuse through emergency care technicians (DETECT) screening tool: results from the DETECT pilot project. J Elder Abuse Negl. 2019;31(2):129-145.
197. Rosen T, Hargarten S, Flomenbaum NE, et al. Identifying Elder Abuse in the Emergency Department: Toward a Multidisciplinary Team-Based Approach. Annals of emergency medicine. 2016;68(3):378-382.
198. Allison EJ, Ellis PC, Wilson SE. Elder abuse and neglect: the emergency medicine perspective. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 1998;5(3):355-363.
199. DeLiema M, Homeier DC, Anglin D, et al. The Forensic Lens: Bringing Elder Neglect Into Focus in the Emergency Department. Annals of emergency medicine. 2016;68(3):371-377.
200. Beach SR, Carpenter CR, Rosen T, et al. Screening and detection of elder abuse: Research opportunities and lessons learned from emergency geriatric care, intimate partner violence, and child abuse. J Elder Abuse Negl. 2016;28(4–5):185-216.
201. Clarke ME, Pierson W. Management of elder abuse in the emergency department. Emergency medicine clinics of North America. 1999;17(3):631-644.
202. Jones J, Dougherty J, Schelble D, et al. Emergency department protocol for the diagnosis and evaluation of geriatric abuse. Annals of emergency medicine. 1988;17(10):1006-1015.
203. Clark-Daniels CL, Daniels RS, Baumhover LA. Abuse and neglect of the elderly: are emergency department personnel aware of mandatory reporting laws?. Annals of emergency medicine. 1990;19(9):970-977.
204. Fulmer T, Paveza G, Abraham I, et al. Elder neglect assessment in the emergency department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2000;26(5):436-443.
205. Uva JL, Guttman T. Elder abuse education in an emergency medicine residency program. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1996;3(8):817-819.
206. Eulitt PJ, Tomberg RJ, Cunningham TD, et al. Screening elders in the emergency department at risk for mistreatment: a pilot study. J Elder Abuse Negl. 2014;26(4):424-435.
207. Lachs MS, Williams CS, O’Brien S, et al. ED use by older victims of family violence. Annals of emergency medicine. 1997;30(4):448-454.
208. Ziminski CE, Phillips LR, Woods DL. Raising the index of suspicion for elder abuse: cognitive impairment, falls, and injury patterns in the emergency department. Geriatr Nurs. 2012;33(2):105-112.
209. Fulmer T, McMahon DJ, Baer-Hines M, et al. Abuse, neglect, abandonment, violence, and exploitation: an analysis of all elderly patients seen in one emergency department during a six-month period. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1992;18(6):505-510.
210. Beck M, Gordon J. A dumping ground for granny. Newsweek. 1991;118(26):64.
211. Gerughty J. Granny dumping. Kentucky hospitals magazine. 1992;9(3):16.
212. Powers JS. Common presentations of elder abuse in health care settings. Clin Geriatr Med. 2014;30(4):729-741.
213. Wong NZ, Rosen T, Sanchez AM, et al. Imaging Findings in Elder Abuse: A Role for Radiologists in Detection. Can Assoc Radiol J. 2017;68(1):16-20.
214. Burgess AW, Watt ME, Brown KM, et al. Management of elder sexual abuse cases in critical care settings. Critical care nursing clinics of North America. 2006;18(3):313-319.
215. Wilber ST. Commentary: Thoughtful practice and the older emergency department patient. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2007;14(6):567-568.
216. Beydoun HA, Williams M, Beydoun MA, et al. Relationship of Physical Intimate Partner Violence with Mental Health Diagnoses in the Nationwide Emergency Department Sample. Journal of women’s health (2002). 2017;26(2):141-151.
217. El-Bassel N, Gilbert L, Witte S, et al. Intimate partner violence and substance abuse among minority women receiving care from an inner-city emergency department. Women’s health issues : official publication of the Jacobs Institute of Women’s Health. 2003;13(1):16-22.
218. Schrager JD, Smith LS, Heron SL, et al. Does stage of change predict improved intimate partner violence outcomes following an emergency department intervention?. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2013;20(2):169-177.
219. Rhodes KV, Kothari CL, Dichter M, et al. Intimate partner violence identification and response: time for a change in strategy. Journal of general internal medicine. 2011;26(8):894-899.
220. Yau RK, Stayton CD, Davidson LL. Indicators of intimate partner violence: identification in emergency departments. The Journal of emergency medicine. 2013;45(3):441-449.
221. Davidov DM, Larrabee H, Davis SM. United States emergency department visits coded for intimate partner violence. The Journal of emergency medicine. 2015;48(1):94-100.
222. Biroscak BJ, Smith PK, Roznowski H, et al. Intimate partner violence against women: findings from one state’s ED surveillance system. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2006;32(1):12-16.
223. Brignone L, Gomez AM. Double jeopardy: Predictors of elevated lethality risk among intimate partner violence victims seen in emergency departments. Preventive medicine. 2017;103:20-25.
224. Lipsky S, Caetano R, Field CA, et al. Is there a relationship between victim and partner alcohol use during an intimate partner violence event? Findings from an urban emergency department study of abused women. Journal of studies on alcohol. 2005;66(3):407-412.
225. Gilbert L, El-Bassel N, Chang M, et al. Substance use and partner violence among urban women seeking emergency care. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2012;26(2):226-235.
226. Snider C, Webster D, O’Sullivan CS, et al. Intimate partner violence: development of a brief risk assessment for the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2009;16(11):1208-1216.
227. Btoush R, Campbell JC, Gebbie KM. Visits coded as intimate partner violence in emergency departments: characteristics of the individuals and the system as reported in a national survey of emergency departments. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2008;34(5):419-427.
228. Caetano R, Cunradi CB, Alter HJ, et al. Drinking and Intimate Partner Violence Severity Levels Among U.S. Ethnic Groups in an Urban Emergency Department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2019;26(8):897-907.
229. McClennan S, Worster A, MacMillan H. Caring for victims of intimate partner violence: a survey of Canadian emergency departments. Cjem. 2008;10(4):325-328.
230. Perciaccante VJ, Carey JW, Susarla SM, et al. Markers for intimate partner violence in the emergency department setting. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2010;68(6):1219-1224.
231. Bazargan-Hejazi S, Kim E, Lin J, et al. Risk factors associated with different types of intimate partner violence (IPV): an emergency department study. The Journal of emergency medicine. 2014;47(6):710-720.
232. Sormanti M, Smith E. Intimate partner violence screening in the emergency department: U.S. medical residents’ perspectives. International quarterly of community health education. 2009;30(1):21-40.
233. Lipsky S, Caetano R, Field CA, et al. Violence-related injury and intimate partner violence in an urban emergency department. The Journal of trauma. 2004;57(2):352-359.
234. Lipsky S, Caetano R. Intimate partner violence perpetration among men and emergency department use. The Journal of emergency medicine. 2011;40(6):696-703.
235. Bair-Merritt MH, Mollen CJ, Yau PL, et al. Health care providers’ opinions on intimate partner violence resources and screening in a pediatric emergency department. Pediatric emergency care. 2006;22(3):150-153.
236. Kramer A, Lorenzon D, Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Women’s health issues : official publication of the Jacobs Institute of Women’s Health. 2004;14(1):19-29.
237. Heron SL, Thompson MP, Jackson E, et al. Do responses to an intimate partner violence screen predict scores on a comprehensive measure of intimate partner violence in low-income black women?. Annals of emergency medicine. 2003;42(4):483-491.
238. Rothman EF, Stuart GL, Winter M, et al. Youth alcohol use and dating abuse victimization and perpetration: a test of the relationships at the daily level in a sample of pediatric emergency department patients who use alcohol. Journal of interpersonal violence. 2012;27(15):2959-2979.
239. Lipsky S, Caetano R. The role of race/ethnicity in the relationship between emergency department use and intimate partner violence: findings from the 2002 National Survey on Drug Use and Health. American journal of public health. 2007;97(12):2246-2252.
240. Halpern LR, Perciaccante VJ, Hayes C, et al. A protocol to diagnose intimate partner violence in the emergency department. The Journal of trauma. 2006;60(5):1101-1105.
241. Lipsky S, Caetano R, Field CA, et al. The role of alcohol use and depression in intimate partner violence among black and Hispanic patients in an urban emergency department. The American journal of drug and alcohol abuse. 2005;31(2):225-242.
242. Newman JD, Sheehan KM, Powell EC. Screening for intimate-partner violence in the pediatric emergency department. Pediatric emergency care. 2005;21(2):79-83.
243. Glass N, Dearwater S, Campbell J. Intimate partner violence screening and intervention: data from eleven Pennsylvania and California community hospital emergency departments. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2001;27(2):141-149.
244. El-Bassel N, Gilbert L, Krishnan S, et al. Partner violence and sexual HIV-risk behaviors among women in an inner-city emergency department. Violence and victims. 1998;13(4):377-393.
245. Schafer SD, Drach LL, Hedberg K, et al. Using diagnostic codes to screen for intimate partner violence in Oregon emergency departments and hospitals. Public health reports (Washington, DC : 1974). 2008;123(5):628-635.
246. Larkin GL, Hyman KB, Mathias SR, et al. Universal screening for intimate partner violence in the emergency department: importance of patient and provider factors. Annals of emergency medicine. 1999;33(6):669-675.
247. Roche M, Moracco KE, Dixon KS, et al. Correlates of intimate partner violence among female patients at a North Carolina emergency department. North Carolina medical journal. 2007;68(2):89-94.
248. Randell KA, Harris D, Stallbaumer-Rouyer J. Immediate and Late Response to Intimate Partner Violence Intervention in the Pediatric Emergency Department: A Case Report. Pediatric emergency care. 2018;34(3):e41-e43.
249. Walton MA, Murray R, Cunningham RM, et al. Correlates of intimate partner violence among men and women in an inner city emergency department. Journal of addictive diseases. 2009;28(4):366-381.
250. Houry D, Kemball RS, Click LA, et al. Development of a brief mental health screen for intimate partner violence victims in the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2007;14(3):202-209.
251. Hollingsworth E, Ford-Gilboe M. Registered nurses’ self-efficacy for assessing and responding to woman abuse in emergency department settings. The Canadian journal of nursing research = Revue canadienne de recherche en sciences infirmieres. 2006;38(4):54-77.
252. Krugman SD, Witting MD, Furuno JP, et al. Perceptions of help resources for victims of intimate partner violence. Journal of interpersonal violence. 2004;19(7):766-777.
253. Ernst AA, Weiss SJ, Morgan-Edwards S, et al. Derivation and validation of a short emergency department screening tool for perpetrators of intimate partner violence: the PErpetrator RaPid Scale (PERPS). The Journal of emergency medicine. 2012;42(2):206-217.
254. Loughlin S, Spinola C, Stewart L, et al. Emergency department staff responses to a protocol of care for abused women. Health education & behavior : the official publication of the Society for Public Health Education. 2000;27(5):572-590.
255. Cunradi CB, Mair C, Ponicki W, et al. Alcohol outlet density and intimate partner violence-related emergency department visits. Alcoholism, clinical and experimental research. 2012;36(5):847-853.
256. Hurley KF, Brown-Maher T, Campbell SG, et al. Emergency department patients’ opinions of screening for intimate partner violence among women. Emergency medicine journal : EMJ. 2005;22(2):97-98.
257. Abbott J, Johnson R, Koziol-McLain J, et al. Domestic violence against women. Incidence and prevalence in an emergency department population. Jama. 1995;273(22):1763-1767.
258. Feldhaus KM, Koziol-McLain J, Amsbury HL, et al. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. Jama. 1997;277(17):1357-1361.
259. Choo EK, Nicolaidis C, Newgard CD, et al. Association between emergency department resources and diagnosis of intimate partner violence. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 2012;19(2):83-88.
260. Edwardsen EA, Morse D. Intimate partner violence resource materials: assessment of information distribution. Journal of interpersonal violence. 2006;21(8):971-981.
261. Yonaka L, Yoder MK, Darrow JB, et al. Barriers to screening for domestic violence in the emergency department. Journal of continuing education in nursing. 2007;38(1):37-45.
262. Kyriacou DN, McCabe F, Anglin D, et al. Emergency department-based study of risk factors for acute injury from domestic violence against women. Annals of emergency medicine. 1998;31(4):502-506.
263. Krishnan SP, Hilbert JC, Pase M. An examination of intimate partner violence in rural communities: results from a hospital emergency department study from Southwest United States. Family & community health. 2001;24(1):1-14.
264. Ernst AA, Weiss SJ, Cham E, et al. Detecting ongoing intimate partner violence in the emergency department using a simple 4-question screen: the OVAT. Violence and victims. 2004;19(3):375-384.
265. Watt MH, Bobrow EA, Moracco KE. Providing support to IPV victims in the emergency department: vignette-based interviews with IPV survivors and emergency department nurses. Violence against women. 2008;14(6):715-726.
266. Wright RJ, Wright RO, Isaac NE. Response to battered mothers in the pediatric emergency department: a call for an interdisciplinary approach to family violence. Pediatrics. 1997;99(2):186-192.
267. Witting MD, Furuno JP, Hirshon JM, et al. Support for emergency department screening for intimate partner violence depends on perceived risk. Journal of interpersonal violence. 2006;21(5):585-596.
268. Lipsky S, Field CA, Caetano R, et al. Posttraumatic stress disorder symptomatology and comorbid depressive symptoms among abused women referred from emergency department care. Violence and victims. 2005;20(6):645-659.
269. Hayden SR, Barton ED, Hayden M. Domestic violence in the emergency department: how do women prefer to disclose and discuss the issues?. The Journal of emergency medicine. 1997;15(4):447-451.
270. Lo Vecchio F, Bhatia A, Sciallo D. Screening for domestic violence in the emergency department. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 1998;5(4):441-444.
271. Mechem CC, Shofer FS, Reinhard SS, et al. History of domestic violence among male patients presenting to an urban emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1999;6(8):786-791.
272. Campbell JC, Pliska MJ, Taylor W, et al. Battered women’s experiences in the emergency department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1994;20(4):280-288.
273. Furbee PM, Sikora R, Williams JM, et al. Comparison of domestic violence screening methods: a pilot study. Annals of emergency medicine. 1998;31(4):495-501.
274. Emergency department response to domestic violence–California, 1992. MMWR Morbidity and mortality weekly report. 1993;42(32):617-620.
275. Wadman MC, Muelleman RL. Domestic violence homicides: ED use before victimization. The American journal of emergency medicine. 1999;17(7):689-691.
276. Isaac NE, Sanchez RL. Emergency department response to battered women in Massachusetts. Annals of emergency medicine. 1994;23(4):855-858.
277. Mayer BW. Female domestic violence victims: perspectives on emergency care. Nursing science quarterly. 2000;13(4):340-346.
278. McLaughlin SA, Crandall CS, Fullerton L, et al. Comparison of intimate partner violence reporting between an emergency department and a clinic setting. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1999;6(12):1292-1295.
279. Billy BJ. Life patterns and emergency care of battered women. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1983;9(5):251-253.
280. Hadley SM. Working with battered women in the emergency department: a model program. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1992;18(1):18-23.
281. McLeer SV, Anwar R. A study of battered women presenting in an emergency department. American journal of public health. 1989;79(1):65-66.
282. Hink AB, Toschlog E, Waibel B, et al. Risks go beyond the violence: Association between intimate partner violence, mental illness, and substance abuse among females admitted to a rural Level I trauma center. The journal of trauma and acute care surgery. 2015;79(5):709-714.
283. Briere J, Zaidi LY. Sexual abuse histories and sequelae in female psychiatric emergency room patients. The American journal of psychiatry. 1989;146(12):1602-1606.
284. Feldhaus KM, Houry D, Kaminsky R. Lifetime sexual assault prevalence rates and reporting practices in an emergency department population. Annals of emergency medicine. 2000;36(1):23-27.
285. Williams JR, Halstead V, Salani D, et al. Intimate Partner Violence Screening and Response: Policies and Procedures Across Health Care Facilities. Women’s health issues : official publication of the Jacobs Institute of Women’s Health. 2016;26(4):377-383.
286. Intimate partner violence injuries–Oklahoma, 2002. MMWR Morbidity and mortality weekly report. 2005;54(41):1041-1045.
287. Hoelle RM, Elie MC, Weeks E, et al. Evaluation of healthcare use trends of high-risk female intimate partner violence victims. The western journal of emergency medicine. 2015;16(1):107-113.
288. Vijayaraghavan M, Tochterman A, Hsu E, et al. Health, access to health care, and health care use among homeless women with a history of intimate partner violence. Journal of community health. 2012;37(5):1032-1039.
289. Randell KA, Bledsoe LK, Shroff PL, et al. Educational interventions for intimate partner violence: guidance from survivors. Pediatric emergency care. 2012;28(11):1190-1196.
290. Coben JH, Friedman DI. Health care use by perpetrators of domestic violence. The Journal of emergency medicine. 2002;22(3):313-317.
291. Pakieser RA, Lenaghan PA, Muelleman RL. Battered women: where they go for help. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1998;24(1):16-19.
292. Boyle DJ, Hassett-Walker C. Individual-level and socio-structural characteristics of violence: an Emergency Department study. Journal of interpersonal violence. 2008;23(8):1011-1026.
293. Sprecher AG, Muelleman RL, Wadman MC. A neural network model analysis to identify victims of intimate partner violence. The American journal of emergency medicine. 2004;22(2):87-89.
294. MacMillan HL, Wathen CN, Jamieson E, et al. Screening for intimate partner violence in health care settings: a randomized trial. Jama. 2009;302(5):493-501.
295. Wolff J, Cantos A, Zun L, et al. Enhanced Versus Basic Referral for Intimate Partner Violence in an Urban Emergency Department Setting. The Journal of emergency medicine. 2017;53(5):771-777.
296. Trautman DE, McCarthy ML, Miller N, et al. Intimate partner violence and emergency department screening: computerized screening versus usual care. Annals of emergency medicine. 2007;49(4):526-534.
297. Bair-Merritt MH, Feudtner C, Mollen CJ, et al. Screening for intimate partner violence using an audiotape questionnaire: a randomized clinical trial in a pediatric emergency department. Archives of pediatrics & adolescent medicine. 2006;160(3):311-316.
298. Scribano PV, Stevens J, Marshall J, et al. Feasibility of computerized screening for intimate partner violence in a pediatric emergency department. Pediatric emergency care. 2011;27(8):710-716.
299. Choo EK, Zlotnick C, Strong DR, et al. BSAFER: A Web-based intervention for drug use and intimate partner violence demonstrates feasibility and acceptability among women in the emergency department. Substance abuse. 2016;37(3):441-449.
300. Hewitt LN, Bhavsar P, Phelan HA. The secrets women keep: intimate partner violence screening in the female trauma patient. The Journal of trauma. 2011;70(2):320-323.
301. Sampsel K, Szobota L, Joyce D, et al. The impact of a sexual assault/domestic violence program on ED care. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2009;35(4):282-289.
302. Rhodes KV, Rodgers M, Sommers M, et al. Brief Motivational Intervention for Intimate Partner Violence and Heavy Drinking in the Emergency Department: A Randomized Clinical Trial. Jama. 2015;314(5):466-477.
303. Knapp JF, Dowd MD, Kennedy CS, et al. Evaluation of a curriculum for intimate partner violence screening in a pediatric emergency department. Pediatrics. 2006;117(1):110-116.
304. Larkin GL, Rolniak S, Hyman KB, et al. Effect of an administrative intervention on rates of screening for domestic violence in an urban emergency department. American journal of public health. 2000;90(9):1444-1448.
305. Hotch D, Grunfeld AF, Mackay K, et al. An emergency department-based domestic violence intervention program: findings after one year. The Journal of emergency medicine. 1996;14(1):111-117.
306. Tilden VP, Shepherd P. Increasing the rate of identification of battered women in an emergency department: use of a nursing protocol. Research in nursing & health. 1987;10(4):209-215.
307. Ngo QM, Eisman AB, Walton MA, et al. Emergency Department Alcohol Intervention: Effects on Dating Violence and Depression. Pediatrics. 2018;142(1).
308. MacMillan HL, Wathen CN, Jamieson E, et al. Approaches to screening for intimate partner violence in health care settings: a randomized trial. Jama. 2006;296(5):530-536.
309. Kurz D. Interventions with battered women in health care settings. Violence and victims. 1990;5(4):243-256.
310. Ahmad I, Ali PA, Rehman S, et al. Intimate partner violence screening in emergency department: a rapid review of the literature. Journal of clinical nursing. 2017;26(21–22):3271-3285.
311. Patch M, Anderson JC, Campbell JC. Injuries of Women Surviving Intimate Partner Strangulation and Subsequent Emergency Health Care Seeking: An Integrative Evidence Review. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2018;44(4):384-393.
312. Choo EK, Gottlieb AS, DeLuca M, et al. Systematic Review of ED-based Intimate Partner Violence Intervention Research. The western journal of emergency medicine. 2015;16(7):1037-1042.
313. Ernst AA, Weiss SJ. Intimate partner violence from the emergency medicine perspective. Women & health. 2002;35(2–3):71-81.
314. Stark L, Ager A. A systematic review of prevalence studies of gender-based violence in complex emergencies. Trauma, violence & abuse. 2011;12(3):127-134.
315. Daugherty JD, Houry DE. Intimate partner violence screening in the emergency department. Journal of postgraduate medicine. 2008;54(4):301-305.
316. Epstein-Ngo QM, Rothman E. Adolescent Dating Violence in the Emergency Department: Presentation, Screening, and Interventions. Adolescent medicine: state of the art reviews. 2015;26(3):675-691.
317. Wu V, Huff H, Bhandari M. Pattern of physical injury associated with intimate partner violence in women presenting to the emergency department: a systematic review and meta-analysis. Trauma, violence & abuse. 2010;11(2):71-82.
318. Morrison LJ. The battering syndrome: a poor record of detection in the emergency department. The Journal of emergency medicine. 1988;6(6):521-526.
319. Sprague S, Goslings JC, Hogentoren C, et al. Prevalence of intimate partner violence across medical and surgical health care settings: a systematic review. Violence against women. 2014;20(1):118-136.
320. Plichta S. The effects of woman abuse on health care utilization and health status: a literature review. Women’s health issues : official publication of the Jacobs Institute of Women’s Health. 1992;2(3):154-163.
321. Ali P, McGarry J, Dhingra K. Identifying signs of intimate partner violence. Emergency nurse : the journal of the RCN Accident and Emergency Nursing Association. 2016;23(9):25-29.
322. Choo EK, Houry DE. Managing intimate partner violence in the emergency department. Annals of emergency medicine. 2015;65(4):447-451.e441.
323. Rhodes KV, Rodgers M, Sommers M, et al. The Social Health Intervention Project (SHIP): protocol for a randomized controlled clinical trial assessing the effectiveness of a brief motivational intervention for problem drinking and intimate partner violence in an urban emergency department. BMC emergency medicine. 2014;14:10.
324. Ballan MS, Freyer MB. Supporting female survivors of intimate partner violence with disabilities: Recommendations for social workers in the emergency department. Social work in health care. 2017;56(10):950-963.
325. Normandin PA. Identifying Maternal Intimate Partner Violence in the Emergency Department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2015;41(5):444-446.
326. Use screening tools, partnerships to improve identification, care of victims of IPV. ED management : the monthly update on emergency department management. 2015;27(2):19-21.
327. Lutwak N. Screening for intimate partner violence at VA EDs: the time is now. Journal of general internal medicine. 2014;29(2):279.
328. Conti CT. Emergency departments and abuse: policy issues, practice barriers, and recommendations. Journal of the Association for Academic Minority Physicians : the official publication of the Association for Academic Minority Physicians. 1998;9(2):35-39.
329. Mayor S. Brief intervention in emergency department does not reduce partner violence in women, US study shows. BMJ (Clinical research ed). 2015;351:h4205.
330. Mackay K. To screen or not to screen: identification of domestic violence in Canadian emergency departments. Cjem. 2008;10(4):329-332.
331. Dienemann J, Trautman D, Shahan JB, et al. Developing a domestic violence program in an inner-city academic health center emergency department: the first 3 years. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 1999;25(2):110-115.
332. Greany GD. Is she a battered woman? A guide for emergency response. The American journal of nursing. 1984;84(6):724-727.
333. Gottlieb AS. Intimate partner violence: a clinical review of screening and intervention. Women’s health (London, England). 2008;4(5):529-539.
334. Amar AF, Cox CW. Intimate partner violence: implications for critical care nursing. Critical care nursing clinics of North America. 2006;18(3):287-296.
335. Randall T. Hospital-wide program identifies battered women; offers assistance. Jama. 1991;266(9):1177-1179.
336. Chisolm-Straker M, Richardson LD, Cossio T. Combating slavery in the 21st century: the role of emergency medicine. Journal of health care for the poor and underserved. 2012;23(3):980-987.
337. Grace AM, Lippert S, Collins K, et al. Educating health care professionals on human trafficking. Pediatric emergency care. 2014;30(12):856-861.
338. Donahue S, Schwien M, LaVallee D. Educating Emergency Department Staff on the Identification and Treatment of Human Trafficking Victims. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2019;45(1):16-23.
339. Egyud A, Stephens K, Swanson-Bierman B, et al. Implementation of Human Trafficking Education and Treatment Algorithm in the Emergency Department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2017;43(6):526-531.
340. Kaltiso SO, Greenbaum VJ, Agarwal M, et al. Evaluation of a Screening Tool for Child Sex Trafficking Among Patients With High-Risk Chief Complaints in a Pediatric Emergency Department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2018;25(11):1193-1203.
341. Long E, Dowdell EB. Nurses’ Perceptions of Victims of Human Trafficking in an Urban Emergency Department: A Qualitative Study. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2018;44(4):375-383.
342. Mumma BE, Scofield ME, Mendoza LP, et al. Screening for Victims of Sex Trafficking in the Emergency Department: A Pilot Program. The western journal of emergency medicine. 2017;18(4):616-620.
343. Gibbons P, Stoklosa H. Identification and Treatment of Human Trafficking Victims in the Emergency Department: A Case Report. The Journal of emergency medicine. 2016;50(5):715-719.
344. Greenbaum VJ, Dodd M, McCracken C. A Short Screening Tool to Identify Victims of Child Sex Trafficking in the Health Care Setting. Pediatric emergency care. 2018;34(1):33-37.
345. Varma S, Gillespie S, McCracken C, et al. Characteristics of child commercial sexual exploitation and sex trafficking victims presenting for medical care in the United States. Child abuse & neglect. 2015;44:98-105.
346. Armstrong S. Instruments to Identify Commercially Sexually Exploited Children: Feasibility of Use in an Emergency Department Setting. Pediatric emergency care. 2017;33(12):794-799.
347. Lamb-Susca L, Clements PT. Intersection of Human Trafficking and the Emergency Department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2018;44(6):563-569.
348. Chisolm-Straker M. Measured Steps: Evidence-based Anti-Trafficking Efforts in the Emergency Department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2018;25(11):1302-1305.
349. Hachey LM, Phillippi JC. Identification and Management of Human Trafficking Victims in the Emergency Department. Advanced emergency nursing journal. 2017;39(1):31-51.
350. Schwarz C, Unruh E, Cronin K, et al. Human Trafficking Identification and Service Provision in the Medical and Social Service Sectors. Health and human rights. 2016;18(1):181-192.
351. Shandro J, Chisolm-Straker M, Duber HC, et al. Human Trafficking: A Guide to Identification and Approach for the Emergency Physician. Annals of emergency medicine. 2016;68(4):501-508.e501.
352. Becker HJ, Bechtel K. Recognizing victims of human trafficking in the pediatric emergency department. Pediatric emergency care. 2015;31(2):144-147.
353. Miller CL. Child sex trafficking in the emergency department: opportunities and challenges. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2013;39(5):477-478.
354. Haider A, Adler RR, Schneider E, et al. Assessment of Patient-Centered Approaches to Collect Sexual Orientation and Gender Identity Information in the Emergency Department: The EQUALITY Study. JAMA network open. 2018;1(8):e186506.
355. Kodadek LM, Peterson S, Shields RY, et al. Collecting sexual orientation and gender identity information in the emergency department : the divide between patient and provider perspectives. Emergency medicine journal : EMJ. 2019;36(3):136-141.
356. Willging C, Gunderson L, Shattuck D, et al. Structural competency in emergency medicine services for transgender and gender non-conforming patients. Social science & medicine (1982). 2019;222:67-75.
357. Harland KK, Peek-Asa C, Saftlas AF. Intimate Partner Violence and Controlling Behaviors Experienced by Emergency Department Patients: Differences by Sexual Orientation and Gender Identification. Journal of interpersonal violence. 2018.
358. Romanelli M, Lu W, Lindsey MA. Examining Mechanisms and Moderators of the Relationship Between Discriminatory Health Care Encounters and Attempted Suicide Among U.S. Transgender Help-Seekers. Administration and policy in mental health. 2018;45(6):831-849.
359. Chisolm-Straker M, Willging C, Daul AD, et al. Transgender and Gender-Nonconforming Patients in the Emergency Department: What Physicians Know, Think, and Do. Annals of emergency medicine. 2018;71(2):183-188.e181.
360. Samuels EA, Tape C, Garber N, et al. “Sometimes You Feel Like the Freak Show”: A Qualitative Assessment of Emergency Care Experiences Among Transgender and Gender-Nonconforming Patients. Annals of emergency medicine. 2018;71(2):170-182.e171.
361. Haider AH, Schneider EB, Kodadek LM, et al. Emergency Department Query for Patient-Centered Approaches to Sexual Orientation and Gender Identity : The EQUALITY Study. JAMA internal medicine. 2017;177(6):819-828.
362. German D, Kodadek L, Shields R, et al. Implementing Sexual Orientation and Gender Identity Data Collection in Emergency Departments: Patient and Staff Perspectives. LGBT health. 2016;3(6):416-423.
363. Cicero EC, Perry Black B. “I Was a Spectacle… A Freak Show at the Circus”: A Transgender Person’s ED Experience and Implications for Nursing Practice. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2016;42(1):25-30.
364. Jalali S, Levy MJ, Tang N. Prehospital emergency care training practices regarding lesbian, gay, bisexual, and transgender patients in Maryland (USA). Prehospital and disaster medicine. 2015;30(2):163-166.
365. Currier GW, Brown G, Walsh PG, et al. Screening for sexual orientation in psychiatric emergency departments. The western journal of emergency medicine. 2015;16(1):80-84.
366. Moll J, Krieger P, Moreno-Walton L, et al. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know?. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014;21(5):608-611.
367. Bauer GR, Scheim AI, Deutsch MB, et al. Reported emergency department avoidance, use, and experiences of transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. Annals of emergency medicine. 2014;63(6):713-720.e711.
368. Bristol S, Kostelec T, MacDonald R. Improving Emergency Health Care Workers’ Knowledge, Competency, and Attitudes Toward Lesbian, Gay, Bisexual, and Transgender Patients Through Interdisciplinary Cultural Competency Training. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2018;44(6):632-639.
369. Sutter ME, Schabath MB, Quinn GP. Patients Seeking Care in Emergency Departments Prefer to Nonverbally Disclose Sexual Orientation and Gender Identity-Are We Ready to Act?. JAMA network open. 2018;1(8):e186457.
370. Gorton RN, Berdahl CT. Improving the Quality of Emergency Care for Transgender Patients. Annals of emergency medicine. 2018;71(2):189-192.e181.
371. Ehrenfeld J, Gridley S. Education Creates Welcoming Environment for Transgender Patients. ED management : the monthly update on emergency department management. 2016;28(8):90-93.
372. Taylor M. Holistic Care of Older Lesbian, Gay, Bisexual, and Transgender Patients in the Emergency Department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2016;42(2):170-173.
373. Jalali S, Sauer LM. Improving Care for Lesbian, Gay, Bisexual, and Transgender Patients in the Emergency Department. Annals of emergency medicine. 2015;66(4):417-423.
374. Brown JF, Fu J. Emergency department avoidance by transgender persons: another broken thread in the “safety net” of emergency medicine care. Annals of emergency medicine. 2014;63(6):721-722.
375. Shaffer N. Transgender patients: implications for emergency department policy and practice. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2005;31(4):405-407.
376. Rodriguez RM, Torres JR, Sun J, et al. Declared impact of the US President’s statements and campaign statements on Latino populations’ perceptions of safety and emergency care access. PloS one. 2019;14(10):e0222837.
377. Saunders NR, Gill PJ, Holder L, et al. Use of the emergency department as a first point of contact for mental health care by immigrant youth in Canada: a population-based study. CMAJ. 2018;190(40):E1183-E1191.
378. Wang Y, Wilson FA, Stimpson JP, et al. Fewer immigrants have preventable ED visits in the United States. The American journal of emergency medicine. 2018;36(3):352-358.
379. Ohle R, Bleeker H, Yadav K, et al. The immigrant effect: factors impacting use of primary and emergency department care – a Canadian population cross-sectional study. Cjem. 2018;20(2):260-265.
380. McRoy L, Ramamonjiarivelo Z, Epane J, et al. Country of Birth and Variations in Asthma and Wheezing Prevalence, and Emergency Department Utilization in Children: A NHANES Study. J Immigr Minor Health. 2017;19(6):1290-1295.
381. Allen L, Cummings J. Emergency Department Use Among Hispanic Adults: The Role of Acculturation. Medical care. 2016;54(5):449-456.
382. Saunders NR, To T, Parkin PC, et al. Emergency Department Revisits by Urban Immigrant Children in Canada: A Population-Based Cohort Study. The Journal of pediatrics. 2016;170:218-226.
383. Geissler KH, Holmes GM. Emergency Department Use in the US-Mexico Border Region and Violence in Mexico: Is There a Relationship?. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2015;31(3):316-325.
384. Stimpson JP, Wilson FA, Zallman L. ED visits and spending by unauthorized immigrants compared with legal immigrants and US natives. The American journal of emergency medicine. 2014;32(6):679-680.
385. Tarraf W, Vega W, Gonzalez HM. Emergency department services use among immigrant and non-immigrant groups in the United States. J Immigr Minor Health. 2014;16(4):595-606.
386. Maldonado CZ, Rodriguez RM, Torres JR, et al. Fear of discovery among Latino immigrants presenting to the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2013;20(2):155-161.
387. Vaughn LM, Jacquez F. Characteristics of newly immigrated, Spanish-speaking Latinos who use the pediatric emergency department: preliminary findings in a secondary migration city. Pediatric emergency care. 2012;28(4):345-350.
388. Ferayorni A, Sinha M, McDonald FW. Health issues among foreign born uninsured children visiting an inner city pediatric emergency department. J Immigr Minor Health. 2011;13(3):434-444.
389. Bowen DJ, Mickus M, Rosales AN. Factors Influencing Physician Assistant Students’ Attitudes Toward Deservingness of Care for Undocumented Mexicans. J Physician Assist Educ. 2018;29(1):35-38.
390. Hynie M, Ardern CI, Robertson A. Emergency Room Visits by Uninsured Child and Adult Residents in Ontario, Canada: What Diagnoses, Severity and Visit Disposition Reveal About the Impact of Being Uninsured. J Immigr Minor Health. 2016;18(5):948-956.
391. Mitchell CD, Truitt MS, Shifflette VK, et al. Who will cover the cost of undocumented immigrant trauma care?. The journal of trauma and acute care surgery. 2012;72(3):609-612.
392. Cervantes L, Tuot D, Raghavan R, et al. Association of Emergency-Only vs Standard Hemodialysis With Mortality and Health Care Use Among Undocumented Immigrants With End-stage Renal Disease. JAMA internal medicine. 2018;178(2):188-195.
393. Nguyen OK, Vazquez MA, Charles L, et al. Association of Scheduled vs Emergency-Only Dialysis With Health Outcomes and Costs in Undocumented Immigrants With End-stage Renal Disease. JAMA internal medicine. 2019;179(2):175-183.
394. Royl G, Ploner CJ, Leithner C. Headache in the emergency room: the role of immigrant background on the frequency of serious causes and diagnostic procedures. Neurol Sci. 2012;33(4):793-799.
395. Waldrop RD, Felter RA. Inaccurate trauma history due to fear of health care personnel involving law enforcement in children of noncitizen immigrants. Pediatric emergency care. 2010;26(12):928-929.
396. Samra S, Taira BR, Pinheiro E, et al. Undocumented Patients in the Emergency Department: Challenges and Opportunities. The western journal of emergency medicine. 2019;20(5):791-798.
397. Schneberk T, Cooper RJ. Dialysis in Undocumented Patients: Death on the Doorstep of the Emergency Department: May 2018 Annals of Emergency Medicine Journal Club. Annals of emergency medicine. 2018;71(5):650-651.
398. Hacker K, Hurwitz A, Shy B. Providers Fear Immigration Proposals May Cause Some Patients to Nix Care. ED management : the monthly update on emergency department management. 2017;29(5):49-53.
399. DeCamp LR, Godage SK, Valenzuela Araujo D, et al. A Texting Intervention in Latino Families to Reduce ED Use: A Randomized Trial. Pediatrics. 2020;145(1).
400. Kouyoumdjian FG, Cheng SY, Fung K, et al. The health care utilization of people in prison and after prison release: A population-based cohort study in Ontario, Canada. PloS one. 2018;13(8):e0201592.
401. Aalsma MC, Anderson VR, Schwartz K, et al. Preventive Care Use Among Justice-Involved and Non-Justice-Involved Youth. Pediatrics. 2017;140(5).
402. Wood DB, Donofrio JJ, Santillanes G, et al. Treating psychiatric emergencies in incarcerated minors in the emergency department: what is the cost and what is their disposition?. Pediatric emergency care. 2014;30(6):403-408.
403. Frank JW, Andrews CM, Green TC, et al. Emergency department utilization among recently released prisoners: a retrospective cohort study. BMC emergency medicine. 2013;13:16.
404. Winkelman TNA, Genao I, Wildeman C, et al. Emergency Department and Hospital Use Among Adolescents With Justice System Involvement. Pediatrics. 2017;140(5).
405. Meyer JP, Qiu J, Chen NE, et al. Emergency department use by released prisoners with HIV: an observational longitudinal study. PloS one. 2012;7(8):e42416.
406. Nowotny KM. Health care needs and service use among male prison inmates in the United States: A multi-level behavioral model of prison health service utilization. Health & justice. 2017;5(1):9.
407. Martin RA, Couture R, Tasker N, et al. Emergency medical care of incarcerated patients: Opportunities for improvement and cost savings. PloS one. 2020;15(4):e0232243.
408. Wang EA, Hong CS, Shavit S, et al. Engaging individuals recently released from prison into primary care: a randomized trial. American journal of public health. 2012;102(9):e22-29.
409. Wang EA, Hong CS, Samuels L, et al. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public health reports (Washington, DC : 1974). 2010;125(2):171-177.
410. Lessenger JE. Prisoners in the emergency department. Annals of emergency medicine. 1985;14(2):179-183.
411. Zamor R, Byczkowski T, Zhang Y, et al. Language Barriers and the Management of Bronchiolitis in a Pediatric Emergency Department. Academic pediatrics. 2020;20(3):356-363.
412. Taira BR, Torres J, Nguyen A, et al. Language Assistance for the Care of Limited English Proficiency (LEP) Patients in the Emergency Department: A Survey of Providers and Staff. J Immigr Minor Health. 2020;22(3):439-447.
413. Benda NC, Fairbanks RJ, Higginbotham DJ, et al. Observational study to understand interpreter service use in emergency medicine: why the key may lie outside of the initial provider assessment. Emergency medicine journal : EMJ. 2019;36(10):582-588.
414. Aratani Y, Nguyen HA, Sharma V. Asthma-Related Emergency Department Visits Among Low-Income Families With Young Children by Race/Ethnicity and Primary Language. Pediatric emergency care. 2019.
415. Taira BR, Orue A. Language assistance for limited English proficiency patients in a public ED: determining the unmet need. BMC Health Serv Res. 2019;19(1):56.
416. Litzau M, Turner J, Pettit K, et al. Obtaining History with a Language Barrier in the Emergency Department: Perhaps not a Barrier After All. The western journal of emergency medicine. 2018;19(6):934-937.
417. Gutman CK, Cousins L, Gritton J, et al. Professional Interpreter Use and Discharge Communication in the Pediatric Emergency Department. Academic pediatrics. 2018;18(8):935-943.
418. Sarangarm D, Ernst A, Horner R, et al. Cross-Sectional Study of the Relation of Health Literacy to Primary Language and Emergency Department Length of Stay. South Med J. 2017;110(12):796-801.
419. Davey K, Olivieri P, Saul T, et al. Impact of patient race and primary language on ED triage in a system that relies on chief complaint and general appearance. The American journal of emergency medicine. 2017;35(7):1013-1015.
420. Kidd RS, Hamdan S, Carlson KL, et al. Impact of language on prescription fill rates after discharge from a pediatric ED. The American journal of emergency medicine. 2017;35(1):182-183.
421. Olivarez GA, Pham PK, Liberman DB. The Effect of Language on the Discharge Process in a Pediatric Emergency Department. J Immigr Minor Health. 2017;19(6):1397-1403.
422. Samuels-Kalow ME, Stack AM, Amico K, et al. Parental Language and Return Visits to the Emergency Department After Discharge. Pediatric emergency care. 2017;33(6):402-404.
423. McKee MM, Winters PC, Sen A, et al. Emergency Department utilization among Deaf American Sign Language users. Disabil Health J. 2015;8(4):573-578.
424. Njeru JW, St Sauver JL, Jacobson DJ, et al. Emergency department and inpatient health care utilization among patients who require interpreter services. BMC Health Serv Res. 2015;15:214.
425. Samuels-Kalow ME, Stack AM, Porter SC. Parental language and dosing errors after discharge from the pediatric emergency department. Pediatric emergency care. 2013;29(9):982-987.
426. Gallagher RA, Porter S, Monuteaux MC, et al. Unscheduled return visits to the emergency department: the impact of language. Pediatric emergency care. 2013;29(5):579-583.
427. Grover A, Deakyne S, Bajaj L, et al. Comparison of throughput times for limited English proficiency patient visits in the emergency department between different interpreter modalities. J Immigr Minor Health. 2012;14(4):602-607.
428. Ginde AA, Sullivan AF, Corel B, et al. Reevaluation of the effect of mandatory interpreter legislation on use of professional interpreters for ED patients with language barriers. Patient Educ Couns. 2010;81(2):204-206.
429. Ginde AA, Clark S, Camargo CA. Language barriers among patients in Boston emergency departments: use of medical interpreters after passage of interpreter legislation. J Immigr Minor Health. 2009;11(6):527-530.
430. Goldman RD, Amin P, Macpherson A. Language and length of stay in the pediatric emergency department. Pediatric emergency care. 2006;22(9):640-643.
431. Hampers LC, McNulty JE. Professional interpreters and bilingual physicians in a pediatric emergency department: effect on resource utilization. Archives of pediatrics & adolescent medicine. 2002;156(11):1108-1113.
432. Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. Journal of general internal medicine. 2000;15(4):256-264.
433. Hampers LC, Cha S, Gutglass DJ, et al. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103(6 Pt 1):1253-1256.
434. Carrasquillo O, Orav EJ, Brennan TA, et al. Impact of language barriers on patient satisfaction in an emergency department. Journal of general internal medicine. 1999;14(2):82-87.
435. Enguidanos ER, Rosen P. Language as a factor affecting follow-up compliance from the emergency department. The Journal of emergency medicine. 1997;15(1):9-12.
436. Manson A. Language concordance as a determinant of patient compliance and emergency room use in patients with asthma. Medical care. 1988;26(12):1119-1128.
437. Oviedo Ramirez S, Alvarez MJ, Field C, et al. Brief Intervention Among Mexican-Origin Young Adults in the Emergency Department at the USA-Mexico Border: Examining the Role of Patient’s Preferred Language of Intervention in Predicting Drinking Outcomes. Alcohol Alcohol. 2018;53(6):728-734.
438. Sinha M, Khor KN, Amresh A, et al. The use of a kiosk-model bilingual self-triage system in the pediatric emergency department. Pediatric emergency care. 2014;30(1):63-68.
439. Nasr I, Cordero M, Houmes B, et al. Use of a bilingual medical history questionnaire in the emergency department. Annals of emergency medicine. 1993;22(5):824-828.
440. Smith KL. Language barriers in the emergency room. Virtual Mentor. 2012;14(4):301-304.
441. Chan YF, Alagappan K, Rella J, et al. Interpreter services in emergency medicine. The Journal of emergency medicine. 2010;38(2):133-139.
442. Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. Journal of health care for the poor and underserved. 2008;19(2):352-362.
443. Dayaa JA, Bush M, Richmond NL, et al. Patient health literacy and the receipt of opioids in the emergency department. J Opioid Manag. 2019;15(4):267-271.
444. Marco CA, LaFountain A, Thenappan A, et al. Consent for emergency treatment: Emergency department patient recall and understanding. The American journal of emergency medicine. 2019;37(7):1387-1388.
445. Henderson E, Dalawari P, Fitzgerald J, et al. Association of Oral Health Literacy and Dental Visitation in an Inner-City Emergency Department Population. Int J Environ Res Public Health. 2018;15(8).
446. Drent AM, Brousseau DC, Morrison AK. Health Information Preferences of Parents in a Pediatric Emergency Department. Clinical pediatrics. 2018;57(5):519-527.
447. Balakrishnan MP, Herndon JB, Zhang J, et al. The Association of Health Literacy With Preventable Emergency Department Visits: A Cross-sectional Study. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2017;24(9):1042-1050.
448. May M, Brousseau DC, Nelson DA, et al. Why Parents Seek Care for Acute Illness in the Clinic or the ED: The Role of Health Literacy. Academic pediatrics. 2018;18(3):289-296.
449. Kumar VA, Albert NM, Medado P, et al. Correlates of Health Literacy and Its Impact on Illness Beliefs for Emergency Department Patients With Acute Heart Failure. Crit Pathw Cardiol. 2017;16(1):27-31.
450. Samuels-Kalow M, Hardy E, Rhodes K, et al. “Like a dialogue”: Teach-back in the emergency department. Patient Educ Couns. 2016;99(4):549-554.
451. Sheikh S, Hendry P, Kalynych C, et al. Assessing patient activation and health literacy in the ED. The American journal of emergency medicine. 2016;34(1):93-96.
452. Lin MJ, Tirosh AG, Landry A. Examining patient comprehension of emergency department discharge instructions: Who says they understand when they do not?. Intern Emerg Med. 2015;10(8):993-1002.
453. Kiechle ES, Hnat AT, Norman KE, et al. Comparison of brief health literacy screens in the emergency department. J Health Commun. 2015;20(5):539-545.
454. Morrison AK, Brousseau DC, Brazauskas R, et al. Health literacy affects likelihood of radiology testing in the pediatric emergency department. The Journal of pediatrics. 2015;166(4):1037-1041.e1031.
455. Griffey RT, Kennedy SK, D’Agostino McGowan L, et al. Is low health literacy associated with increased emergency department utilization and recidivism?. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014;21(10):1109-1115.
456. Musso MW, Perret JN, Sanders T, et al. Patients’ comprehension of their emergency department encounter: a pilot study using physician observers. Annals of emergency medicine. 2015;65(2):151-155.e154.
457. Morrison AK, Chanmugathas R, Schapira MM, et al. Caregiver low health literacy and nonurgent use of the pediatric emergency department for febrile illness. Academic pediatrics. 2014;14(5):505-509.
458. Morrison AK, Schapira MM, Gorelick MH, et al. Low caregiver health literacy is associated with higher pediatric emergency department use and nonurgent visits. Academic pediatrics. 2014;14(3):309-314.
459. Griffey RT, Melson AT, Lin MJ, et al. Does numeracy correlate with measures of health literacy in the emergency department?. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014;21(2):147-153.
460. Schumacher JR, Hall AG, Davis TC, et al. Potentially preventable use of emergency services: the role of low health literacy. Medical care. 2013;51(8):654-658.
461. Smith PC, Brice JH, Lee J. The relationship between functional health literacy and adherence to emergency department discharge instructions among Spanish-speaking patients. J Natl Med Assoc. 2012;104(11–12):521-527.
462. Engel KG, Buckley BA, Forth VE, et al. Patient understanding of emergency department discharge instructions: where are knowledge deficits greatest?. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2012;19(9):E1035-1044.
463. McNaughton C, Wallston KA, Rothman RL, et al. Short, subjective measures of numeracy and general health literacy in an adult emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2011;18(11):1148-1155.
464. Olives T, Patel R, Patel S, et al. Health literacy of adults presenting to an urban ED. The American journal of emergency medicine. 2011;29(8):875-882.
465. Joyner-Grantham J, Mount DL, McCorkle OD, et al. Self-reported influences of hopelessness, health literacy, lifestyle action, and patient inertia on blood pressure control in a hypertensive emergency department population. Am J Med Sci. 2009;338(5):368-372.
466. Engel KG, Heisler M, Smith DM, et al. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand?. Annals of emergency medicine. 2009;53(4):454-461.e415.
467. Macy ML, Davis MM, Clark SJ, et al. Parental health literacy and asthma education delivery during a visit to a community-based pediatric emergency department: a pilot study. Pediatric emergency care. 2011;27(6):469-474.
468. Shields WC, McDonald EM, McKenzie LB, et al. Does Health Literacy Level Influence the Effectiveness of a Kiosk-Based Intervention Delivered in the Pediatric Emergency Department?. Clinical pediatrics. 2016;55(1):48-55.
469. Ladley A, Hieger AW, Arthur J, et al. Educational Text Messages Decreased Emergency Department Utilization Among Infant Caregivers: A Randomized Trial. Academic pediatrics. 2018;18(6):636-641.
470. Simmons S, Sharp B, Fowler J, et al. Mind the (knowledge) gap: the effect of a communication instrument on emergency department patients’ comprehension of and satisfaction with care. Patient Educ Couns. 2015;98(2):257-262.
471. Merchant RC, Liu T, Clark MA, et al. Facilitating HIV/AIDS and HIV testing literacy for emergency department patients: a randomized, controlled, trial. BMC emergency medicine. 2018;18(1):21.
472. Griffey RT, McNaughton CD, McCarthy DM, et al. Shared Decision Making in the Emergency Department Among Patients With Limited Health Literacy: Beyond Slower and Louder. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2016;23(12):1403-1409.
473. Morrison AK, Myrvik MP, Brousseau DC, et al. The relationship between parent health literacy and pediatric emergency department utilization: a systematic review. Academic pediatrics. 2013;13(5):421-429.
474. Alberti TL, Nannini A. Patient comprehension of discharge instructions from the emergency department: a literature review. J Am Assoc Nurse Pract. 2013;25(4):186-194.
475. Herndon JB, Chaney M, Carden D. Health literacy and emergency department outcomes: a systematic review. Annals of emergency medicine. 2011;57(4):334-345.
476. Carpenter CR, Kaphingst KA, Goodman MS, et al. Feasibility and diagnostic accuracy of brief health literacy and numeracy screening instruments in an urban emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014;21(2):137-146.
477. Riley ED, Vittinghoff E, Kagawa RMC, et al. Violence and Emergency Department Use among Community-Recruited Women Who Experience Homelessness and Housing Instability. J Urban Health. 2020;97(1):78-87.
478. Gabet M, Grenier G, Cao Z, et al. Predictors of Emergency Department Use among Individuals with Current or Previous Experience of Homelessness. Int J Environ Res Public Health. 2019;16(24).
479. Lombardi K, Pines JM, Mazer-Amirshahi M, et al. Findings of a national dataset analysis on the visits of homeless patients to US emergency departments during 2005–2015. Public Health. 2020;178:82-89.
480. Yamamoto A, Needleman J, Gelberg L, et al. Association between homelessness and opioid overdose and opioid-related hospital admissions/emergency department visits. Social science & medicine (1982). 2019;242:112585.
481. Jackson TS, Moran TP, Lin J, et al. Homelessness Among Patients in a Southeastern Safety Net Emergency Department. South Med J. 2019;112(9):476-482.
482. McCallum R, Medved MI, Hiebert-Murphy D, et al. Fixed Nodes of Transience: Narratives of Homelessness and Emergency Department Use. Qual Health Res. 2020;30(8):1183-1195.
483. Moore M, Conrick KM, Reddy A, et al. From Their Perspective: The Connection between Life Stressors and Health Care Service Use Patterns of Homeless Frequent Users of the Emergency Department. Health Soc Work. 2019;44(2):113-122.
484. Moulin A, Evans EJ, Xing G, et al. Substance Use, Homelessness, Mental Illness and Medicaid Coverage: A Set-up for High Emergency Department Utilization. The western journal of emergency medicine. 2018;19(6):902-906.
485. Stewart AM, Kanak MM, Gerald AM, et al. Pediatric Emergency Department Visits for Homelessness After Shelter Eligibility Policy Change. Pediatrics. 2018;142(5).
486. Kanak M, Stewart A, Vinci R, et al. Trends in Homeless Children and Young Adults Seeking Shelter in a Boston Pediatric Emergency Department Following State Housing Policy Changes, 2011–2016. American journal of public health. 2018;108(8):1076-1078.
487. Amato S, Nobay F, Amato DP, et al. Sick and unsheltered: Homelessness as a major risk factor for emergency care utilization. The American journal of emergency medicine. 2019;37(3):415-420.
488. Doran KM, Rahai N, McCormack RP, et al. Substance use and homelessness among emergency department patients. Drug Alcohol Depend. 2018;188:328-333.
489. Feldman BJ, Craen AM, Enyart J, et al. Prevalence of Homelessness by Gender in an Emergency Department Population in Pennsylvania. J Am Osteopath Assoc. 2018;118(2):85-91.
490. Berkowitz SA, Kalkhoran S, Edwards ST, et al. Unstable Housing and Diabetes-Related Emergency Department Visits and Hospitalization: A Nationally Representative Study of Safety-Net Clinic Patients. Diabetes Care. 2018;41(5):933-939.
491. Hwang YW, Lee YJ, Kong SY. Epidemiology and clinical outcomes of tuberculosis among homeless persons visiting emergency department in public hospital. The American journal of emergency medicine. 2018;36(1):164-166.
492. Gundlapalli AV, Jones AL, Redd A, et al. Characteristics of the Highest Users of Emergency Services in Veterans Affairs Hospitals: Homeless and Non-Homeless. Stud Health Technol Inform. 2017;238:24-27.
493. Holtyn AF, Jarvis BP, Subramaniam S, et al. An intensive assessment of alcohol use and emergency department utilization in homeless alcohol-dependent adults. Drug Alcohol Depend. 2017;178:28-31.
494. Jetelina KK, Reingle Gonzalez JM, Brown CVR, et al. Acute Alcohol Use, History of Homelessness, and Intent of Injury Among a Sample of Adult Emergency Department Patients. Violence and victims. 2017;32(4):658-670.
495. Mitchell MS, Leon CLK, Byrne TH, et al. Cost of health care utilization among homeless frequent emergency department users. Psychol Serv. 2017;14(2):193-202.
496. Moore DT, Rosenheck RA. Comprehensive services delivery and emergency department use among chronically homeless adults. Psychol Serv. 2017;14(2):184-192.
497. Feldman BJ, Calogero CG, Elsayed KS, et al. Prevalence of Homelessness in the Emergency Department Setting. The western journal of emergency medicine. 2017;18(3):366-372.
498. Gabrielian S, Chen JC, Minhaj BP, et al. Feasibility and Acceptability of a Colocated Homeless-Tailored Primary Care Clinic and Emergency Department. J Prim Care Community Health. 2017;8(4):338-344.
499. Hategan A, Tisi D, Abdurrahman M, et al. Geriatric Homelessness: Association with Emergency Department Utilization. Can Geriatr J. 2016;19(4):189-194.
500. Lam CN, Arora S, Menchine M. Increased 30-Day Emergency Department Revisits Among Homeless Patients with Mental Health Conditions. The western journal of emergency medicine. 2016;17(5):607-612.
501. Raven MC, Tieu L, Lee CT, et al. Emergency Department Use in a Cohort of Older Homeless Adults: Results From the HOPE HOME Study. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2017;24(1):63-74.
502. Jaworsky D, Gadermann A, Duhoux A, et al. Residential Stability Reduces Unmet Health Care Needs and Emergency Department Utilization among a Cohort of Homeless and Vulnerably Housed Persons in Canada. J Urban Health. 2016;93(4):666-681.
503. Moore DT, Rosenheck RA. Factors Affecting Emergency Department Use by a Chronically Homeless Population. Psychiatr Serv. 2016;67(12):1340-1347.
504. Figueiredo R, Dempster L, Quinonez C, et al. Emergency Department Use for Dental Problems among Homeless Individuals: A Population-Based Cohort Study. Journal of health care for the poor and underserved. 2016;27(2):860-868.
505. Doran KM, McCormack RP, Johns EL, et al. Emergency Department Visits for Homelessness or Inadequate Housing in New York City before and after Hurricane Sandy. J Urban Health. 2016;93(2):331-344.
506. Tadros A, Layman SM, Brewer MP, et al. A 5-year comparison of ED visits by homeless and nonhomeless patients. The American journal of emergency medicine. 2016;34(5):805-808.
507. Mackelprang JL, Qiu Q, Rivara FP. Predictors of Emergency Department Visits and Inpatient Admissions Among Homeless and Unstably Housed Adolescents and Young Adults. Medical care. 2015;53(12):1010-1017.
508. Lin WC, Bharel M, Zhang J, et al. Frequent Emergency Department Visits and Hospitalizations Among Homeless People With Medicaid: Implications for Medicaid Expansion. American journal of public health. 2015;105:S716-722.
509. Cheung A, Somers JM, Moniruzzaman A, et al. Emergency department use and hospitalizations among homeless adults with substance dependence and mental disorders. Addict Sci Clin Pract. 2015;10:17.
510. Wang H, Nejtek VA, Zieger D, et al. The role of charity care and primary care physician assignment on ED use in homeless patients. The American journal of emergency medicine. 2015;33(8):1006-1011.
511. Forchuk C, Reiss JP, Mitchell B, et al. Homelessness and housing crises among individuals accessing services within a Canadian emergency department. J Psychiatr Ment Health Nurs. 2015;22(6):354-359.
512. Svoboda T. Difficult behaviors in the emergency department: a cohort study of housed, homeless and alcohol dependent individuals. PloS one. 2014;10(4):e0124528.
513. Thakarar K, Morgan JR, Gaeta JM, et al. Predictors of Frequent Emergency Room Visits among a Homeless Population. PloS one. 2015;10(4):e0124552.
514. Coe AB, Moczygemba LR, Harpe SE, et al. Homeless patients’ use of urban emergency departments in the United States. J Ambul Care Manage. 2015;38(1):48-58.
515. Doran KM, Curry LA, Vashi AA, et al. “Rewarding and challenging at the same time”: emergency medicine residents’ experiences caring for patients who are homeless. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014;21(6):673-679.
516. Ku BS, Fields JM, Santana A, et al. The urban homeless: super-users of the emergency department. Popul Health Manag. 2014;17(6):366-371.
517. Hammig B, Jozkowski K, Jones C. Injury-related visits and comorbid conditions among homeless persons presenting to emergency departments. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014;21(4):449-455.
518. Kay HF, Sathiyakumar V, Archer KR, et al. The homeless orthopaedic trauma patient: follow-up, emergency room usage, and complications. J Orthop Trauma. 2014;28(6):e128-132.
519. Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: national comparison of homeless and nonhomeless US veterans who use Veterans Affairs Emergency Departments. American journal of public health. 2013;103:S225-231.
520. Doran KM, Vashi AA, Platis S, et al. Navigating the boundaries of emergency department care: addressing the medical and social needs of patients who are homeless. American journal of public health. 2013;103:S355-360.
521. Chambers C, Chiu S, Katic M, et al. High utilizers of emergency health services in a population-based cohort of homeless adults. American journal of public health. 2013;103:S302-310.
522. Mackelprang JL, Graves JM, Rivara FP. Homeless in America: injuries treated in US emergency departments, 2007–2011. International journal of injury control and safety promotion. 2014;21(3):289-297.
523. Fine AG, Zhang T, Hwang SW. Attitudes towards homeless people among emergency department teachers and learners: a cross-sectional study of medical students and emergency physicians. BMC Med Educ. 2013;13:112.
524. Brown RT, Steinman MA. Characteristics of emergency department visits by older versus younger homeless adults in the United States. American journal of public health. 2013;103(6):1046-1051.
525. Tsai J, Rosenheck RA. Risk factors for ED use among homeless veterans. The American journal of emergency medicine. 2013;31(5):855-858.
526. Morrison A, Roman B, Borges N. Psychiatry and emergency medicine: medical student and physician attitudes toward homeless persons. Acad Psychiatry. 2012;36(3):211-215.
527. Ku BS, Scott KC, Kertesz SG, et al. Factors associated with use of urban emergency departments by the U.S. homeless population. Public health reports (Washington, DC : 1974). 2010;125(3):398-405.
528. Oates G, Tadros A, Davis SM. A comparison of National Emergency Department use by homeless versus non-homeless people in the United States. Journal of health care for the poor and underserved. 2009;20(3):840-845.
529. Pearson DA, Bruggman AR, Haukoos JS. Out-of-hospital and emergency department utilization by adult homeless patients. Annals of emergency medicine. 2007;50(6):646-652.
530. Han B, Wells BL. Inappropriate emergency department visits and use of the Health Care for the Homeless Program services by Homeless adults in the northeastern United States. J Public Health Manag Pract. 2003;9(6):530-537.
531. Kushel MB, Perry S, Bangsberg D, et al. Emergency department use among the homeless and marginally housed: results from a community-based study. American journal of public health. 2002;92(5):778-784.
532. D’Amore J, Hung O, Chiang W, et al. The epidemiology of the homeless population and its impact on an urban emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2001;8(11):1051-1055.
533. Padgett DK, Struening EL, Andrews H, et al. Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling and need factors. Social science & medicine (1982). 1995;41(4):547-556.
534. Orenstein JB, Boenning DA, Engh EP, et al. Emergency care of children in shelters. Pediatric emergency care. 1992;8(6):313-317.
535. Padgett DK, Struening EL. Influence of substance abuse and mental disorders on emergency room use by homeless adults. Hosp Community Psychiatry. 1991;42(8):834-838.
536. Bachrach LL, Santiago JM, Berren MR. Homeless mentally ill patients in the community: results of a general hospital emergency room study. Community Ment Health J. 1990;26(5):415-423.
537. McCormack RP, Hoffman LF, Wall SP, et al. Resource-limited, collaborative pilot intervention for chronically homeless, alcohol-dependent frequent emergency department users. American journal of public health. 2013;103:S221-224.
538. Castillo EM, Chan TC, Tolia VM, et al. Effect of a Computerized Alert on Emergency Department Hepatitis A Vaccination in Homeless Patients During a Large Regional Outbreak. The Journal of emergency medicine. 2018;55(6):764-768.
539. Clarke GN, Herinckx HA, Kinney RF, et al. Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Ment Health Serv Res. 2000;2(3):155-164.
540. Redelmeier DA, Molin JP, Tibshirani RJ. A randomised trial of compassionate care for the homeless in an emergency department. Lancet. 1995;345(8958):1131-1134.
541. Sadowski LS, Kee RA, VanderWeele TJ, et al. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. Jama. 2009;301(17):1771-1778.
542. Doran KM. Commentary: How Can Emergency Departments Help End Homelessness? A Challenge to Social Emergency Medicine. Ann Emerg Med. 2019;74(5S):S41-S44.
543. Raven MC. Homelessness and the Practice of Emergency Medicine: Challenges, Gaps in Care, and Moral Obligations. Annals of emergency medicine. 2019;74(5S):S33-S37.
544. Komenski RR, Keaton K, Marsiglia C. Replacing a Revolving Door. Care transition programs that address homelessness are one way to reduce emergency visits. Healthc Exec. 2015;30(2):54-57.
545. Doran KM, Raven MC. Homelessness and Emergency Medicine: Where Do We Go From Here?. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2018;25(5):598-600.
546. Morris DM, Gordon JA. The role of the emergency department in the care of homeless and disadvantaged populations. Emergency medicine clinics of North America. 2006;24(4):839-848.
547. Bharel M. Emergency Care for Homeless Patients: A Window Into the Health Needs of Vulnerable Populations. American journal of public health. 2016;106(5):784-785.
548. Salhi BA, White MH, Pitts SR, et al. Homelessness and Emergency Medicine: A Review of the Literature. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2018;25(5):577-593.
549. Peltz A, Garg A. Food Insecurity and Health Care Use. Pediatrics. 2019;144(4).
550. Berkowitz SA, Seligman HK, Meigs JB, et al. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. The American journal of managed care. 2018;24(9):399-404.
551. Gerber E, Gelberg L, Rotrosen J, et al. Health-related material needs and substance use among emergency department patients. Substance abuse. 2020;41(2):196-202.
552. Schroeder EB, Zeng C, Sterrett AT, et al. The longitudinal relationship between food insecurity in older adults with diabetes and emergency department visits, hospitalizations, hemoglobin A1c, and medication adherence. Journal of diabetes and its complications. 2019;33(4):289-295.
553. Gattu RK, Paik G, Wang Y, et al. The Hunger Vital Sign Identifies Household Food Insecurity among Children in Emergency Departments and Primary Care. Children (Basel Switzerland). 2019;6(10).
554. Mendoza JA, Haaland W, D’Agostino RB, et al. Food insecurity is associated with high risk glycemic control and higher health care utilization among youth and young adults with type 1 diabetes. Diabetes research and clinical practice. 2018;138:128-137.
555. Robinson T, Bryan L, Johnson V, et al. Hunger: A Missed Opportunity for Screening in the Pediatric Emergency Department. Clin Pediatr (Phila). 2018;57(11):1318-1325.
556. Ojinnaka CO, Heflin C. Supplemental Nutrition Assistance Program size and timing and hypertension-related emergency department claims among Medicaid enrollees. Journal of the American Society of Hypertension : JASH. 2018;12(11):e27-e34.
557. Martel ML, Klein LR, Hager KA, et al. Emergency Department Experience with Novel Electronic Medical Record Order for Referral to Food Resources. The western journal of emergency medicine. 2018;19(2):232-237.
558. Burks CE, Jones CW, Braz VA, et al. Risk Factors for Malnutrition among Older Adults in the Emergency Department: A Multicenter Study. Journal of the American Geriatrics Society. 2017;65(8):1741-1747.
559. Basu S, Berkowitz SA, Seligman H. The Monthly Cycle of Hypoglycemia: An Observational Claims-based Study of Emergency Room Visits, Hospital Admissions, and Costs in a Commercially Insured Population. Medical care. 2017;55(7):639-645.
560. Pabalan L, Dunn R, Gregori K, et al. Assessment of Food Insecurity in Children’s Hospital of Wisconsin’s Emergency Department. WMJ : official publication of the State Medical Society of Wisconsin. 2015;114(4):148-151.
561. Sullivan AF, Clark S, Pallin DJ, et al. Food security, health, and medication expenditures of emergency department patients. The Journal of emergency medicine. 2010;38(4):524-528.
562. Semple-Hess JE, Pham PK, Cohen SA, et al. Community Resource Needs Assessment Among Families Presenting to a Pediatric Emergency Department. Academic pediatrics. 2019;19(4):378-385.
563. Nhoung HK, Goyal M, Cacciapuoti M, et al. Food Insecurity and Insulin Use in Hyperglycemic Patients Presenting to the Emergency Department. The western journal of emergency medicine. 2020;21(4):959-963.
564. Miner JR, Westgard B, Olives TD, et al. Hunger and Food Insecurity among Patients in an Urban Emergency Department. The western journal of emergency medicine. 2013;14(3):253-262.
565. Kersey MA, Beran MS, McGovern PG, et al. The prevalence and effects of hunger in an emergency department patient population. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1999;6(11):1109-1114.
566. Hendrickson MA, O’Riordan MA, Arpilleda JC, et al. Effects of food insecurity on asthma outcomes in the pediatric emergency department. Pediatric emergency care. 2010;26(11):823-829.
567. Biros MH, Hoffman PL, Resch K. The prevalence and perceived health consequences of hunger in emergency department patient populations. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2005;12(4):310-317.
568. Heflin C, Hodges L, Mueser P. Supplemental Nutrition Assistance Progam benefits and emergency room visits for hypoglycaemia. Public health nutrition. 2017;20(7):1314-1321.
569. Cotti CD, Gordanier JM, Ozturk OD. Hunger pains? SNAP timing and emergency room visits. Journal of health economics. 2020;71:102313.
570. Tarasuk V, Cheng J, Gundersen C, et al. The Relation between Food Insecurity and Mental Health Care Service Utilization in Ontario. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2018;63(8):557-569.
571. Bhargava V, Lee JS. Food Insecurity and Health Care Utilization Among Older Adults. Journal of applied gerontology : the official journal of the Southern Gerontological Society. 2017;36(12):1415-1432.
572. Makelarski JA, Abramsohn E, Benjamin JH, et al. Diagnostic Accuracy of Two Food Insecurity Screeners Recommended for Use in Health Care Settings. American journal of public health. 2017;107(11):1812-1817.
573. Skalicky A, Meyers AF, Adams WG, et al. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Maternal and child health journal. 2006;10(2):177-185.
574. Power-Hays A, Patterson A, Sobota A. Household material hardships impact emergency department reliance in pediatric patients with sickle cell disease. Pediatric blood & cancer. 2020:e28587.
575. Cullen D, Blauch A, Mirth M, et al. Complete Eats: Summer Meals Offered by the Emergency Department for Food Insecurity. Pediatrics. 2019;144(4).
576. Cullen D, Woodford A, Fein J. Food for Thought: A Randomized Trial of Food Insecurity Screening in the Emergency Department. Academic pediatrics. 2019;19(6):646-651.
577. Adams JG. Confronting hunger in the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1999;6(11):1082-1084.
578. Morris AM, Engelberg Anderson JK, Schmitthenner B, et al. Leveraging emergency department visits to connect older adults at risk for malnutrition and food insecurity to community resources: design and protocol development for the BRIDGE study. Pilot and feasibility studies. 2020;6:36.
579. Carlson LC, Baker ON, Schuur JD. A Geospatial Analysis of Freestanding and Hospital Emergency Department Accessibility via Public Transit. The western journal of emergency medicine. 2019;20(3):472-476.
580. Blome A, Rosenbaum J, Lucas N, et al. Ridesharing as an Alternative to Ambulance Transport for Voluntary Psychiatric Patients in the Emergency Department. The western journal of emergency medicine. 2020;21(3):618-621.
581. Kwa L, Silverberg JI. Financial burden of emergency department visits for atopic dermatitis in the United States. J Am Acad Dermatol. 2018;79(3):443-447.
582. Jackson TJ, Blumberg TJ, Shah AS, et al. Inappropriately Timed Pediatric Orthopaedic Referrals From the Emergency Department Result in Unnecessary Appointments and Financial Burden for Patients. Journal of pediatric orthopedics. 2018;38(3):e128-e132.
583. Jonassaint CR, Beach MC, Haythornthwaite JA, et al. The Association between Educational Attainment and Patterns of Emergency Department Utilization among Adults with Sickle Cell Disease. International journal of behavioral medicine. 2016;23(3):300-309.
584. Platts-Mills TF, Hunold KM, Bortsov AV, et al. More educated emergency department patients are less likely to receive opioids for acute pain. Pain. 2012;153(5):967-973.
585. Hamadi H, Apatu E, Osagiede O, et al. Insight Into Health Care Services: A Characterization of Emergency Room Visits and Economic Hazards in the United States. Disaster medicine and public health preparedness. 2019;13(3):470-475.
586. Madan AK, Sapozhnik J, Tillou A, et al. Unemployment rates and trauma admissions. World journal of surgery. 2007;31(10):1930-1933.
587. Giannouchos TV, Kum HC, Foster MJ, et al. Characteristics and predictors of adult frequent emergency department users in the United States: A systematic literature review. Journal of evaluation in clinical practice. 2019;25(3):420-433.
588. Balhara KS, Fisher L, El Hage N, et al. Social determinants of health associated with hemodialysis non-adherence and emergency department utilization: a pilot observational study. BMC Nephrol. 2020;21(1):4.
589. Cortright L, Buckman C, Tumin D, et al. Social Determinants of Health and Emergency Department Use Among Children With Sickle Cell Disease. J Pediatr Hematol Oncol. 2020;42(1):e42-e45.
590. Vest JR, Ben-Assuli O. Prediction of emergency department revisits using area-level social determinants of health measures and health information exchange information. Int J Med Inform. 2019;129:205-210.
591. Axelson DJ, Stull MJ, Coates WC. Social Determinants of Health: A Missing Link in Emergency Medicine Training. AEM Educ Train. 2018;2(1):66-68.
592. Anderson ES, Lippert S, Newberry J, et al. Addressing Social Determinants of Health from the Emergency Department through Social Emergency Medicine. The western journal of emergency medicine. 2016;17(4):487-489.
593. Palepu A, Strathdee SA, Hogg RS, et al. The social determinants of emergency department and hospital use by injection drug users in Canada. J Urban Health. 1999;76(4):409-418.
594. Moffett SE, Shahidi H, Sule H, et al. Social Determinants of Health Curriculum Integrated Into a Core Emergency Medicine Clerkship. MedEdPORTAL. 2019;15:10789.
595. The Culture of Gun Violence: An Active Learning Exercise. 2014.


