| Author | Affiliation |
|---|---|
| Alexander J. Scumpia, DO, MSc | Mount Sinai Medical Center, Department of Emergency Medicine, Miami Beach, Florida |
| John Serak, MD | Jackson Memorial Health System, Department of Neurosurgery, Miami, Florida |
| Kirsten L. Ritchie, DO, MSc | Mount Sinai Medical Center, Department of Emergency Medicine, Miami Beach, Florida |
| Scott Kohl, DO | Jackson Memorial Health System, Department of Emergency Medicine, Miami, Florida |
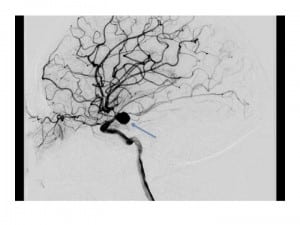
A 20-year-old-female presented to the emergency department (ED) with a chief complaint of a persistent dull headache associated with a 7 mm dilated, non-reactive right pupil, and occasional blurry vision for 4 days. The patient had a past medical history significant for Noonan’s syndrome (NS). In the ED the patient’s physical examination demonstrated normal vital signs, chronic right divergent strabismus (Figure 1), a dilated right 7 mm pupil (Figure 2), and intact extraocular muscles without visual field cuts or other acute neurological deficits. Computed tomography angiography of the brain demonstrated the diagnosis (Figure 3).

The patient is shown demonstrating right ocular divergent strabismus hypertelorism, low set ears, and craniofacial dysmorphism. The patient’s low posterior hairline and webbed neck are not visualized.

The patient’s 7 mm dilated non-reactive right pupil.
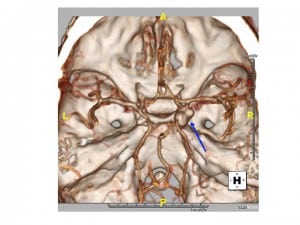
Computed tomography angiography of the brain illustrating homogeneous enhancement of a 1.1 × 0.8 × 0.8 cm bilobed, saccular aneurysm (blue arrow) in the region of the right posterior communicating artery.
Oculomotor nerve palsy (ONP) in patients with posterior communicating artery aneurysms (PCoA) is known clinically.1 Direct compression of the oculomotor nerve by the aneurysm itself is considered to be the mechanism causing ONP in patients without subarachnoid hemorrhage.2 NS is an autosomal-dominant condition of multiple congenital abnormalities, regarded as a type of dwarfism with a reported incidence of between 1 in 1,000 and 1 in 2,500 live births.3 These abnormalities include craniofacial anomalies, such as ocular hypertelorism, low-set ears, low posterior hairline and webbed neck; shield-shaped chest; cubitus valgus; cryptorchidism; and congenital heart defects.4Interestingly, well documented cases of patients with NS and valvular and non-cerebral vascular lesions may show a preponderance for underlying defects in vascular architecture, i.e. Ehlers-Danlos syndrome.3 Only 4 cases of intracranial aneurysms have been previously reported in individuals with NS.3 Finally, careful attention must be paid to all patients, not just those with NS, who present with a new onset dilated pupil; and should raise one’s suspicion of an underlying PCoA (Figure 4).
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted October 25, 2012; Accepted November 19, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.11.14368
Address for Correspondence: Alexander J. Scumpia, DO. Mount Sinai Medical Center, 4300 Alton Road. Miami Beach, FL 33140. Email: ascumpia@yahoo.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Soni SR. Aneurysms of the posterior communicating artery and oculomotor paresis. J Neurol Neurosurg Psychiatry. 1974;37:475–484. [PMC free article] [PubMed]
2. Fujiwara S, Fujii K, Nishio S, et al. Oculomotor nerve palsy in patients with cerebral aneurysms.Neurosurg Rev. 1989;12:123–132. [PubMed]
3. Aneurysmal sub-arachnoid haemorrhage in patients with Noonan syndrome: a report of two cases and review of neurovascular presentations in this syndrome. Neuroradiology. 2004;46:301–305.[PubMed]
4. Collins E, Turner G. The Noonan Syndrome. J Paediatr. 1973;83:941–950. [PubMed]