| Author | Affiliation |
|---|---|
| Daniel C. McGillicuddy, MD | Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA |
| Jennifer de La Pena, MD | Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA |
| James Scott Goudie, MD | Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA |
| Jonathan Fisher, MD, MPH | Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA |
| Nathan Shapiro, MD, MPH | Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA |
| Leon D. Sanchez, MD, MPH | Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA |
INTRODUCTION
Many medications are administered according to the weight of the patient. Because it is often not available in the emergency department (ED), the patient’s weight is therefore estimated. Several studies have shown that emergency physicians are inaccurate at estimating a patient’s weight.1–3Medications to facilitate intubation, induction agents and paralytics are often weight-based. This study evaluated the accuracy of dosing succinylcholine, a paralytic and etomidate, an induction agent, in our ED.
METHODS
We conducted a retrospective chart review of all patients intubated in the ED between January 1, 2004 and December 31, 2004, at an urban Level I trauma center with approximately 50,000 ED visits annually. We identified all ED intubations by retrospectively reviewing the hospital financial databases for intubations of ED patients, and by patients who had critical care billing for an intubation procedure or for ventilator use in the ED. We also examined ED patient logs to identify all patients who were admitted to the intensive care unit (ICU), the operating rooms, or had expired. All intubations were tied to a unique visit. We reviewed the charts to determine if an intubation took place in the ED, and we recorded the dosages of all intubation medications used. We excluded from our cohort patients who were intubated prior to arrival in our ED either by another hospital or by pre-hospital personnel.
We measured the patient’s actual weight using standard ICU bed scales on admission and then recorded it. The dosages of the intubation medications were calculated in mg/kg and compared to the standard dosages (etomidate 0.2–0.3mg/kg and succinylcholine 1–1.5mg/kg) to determine if they were accurate. We obtained the standard dose of succinylcholine from Micromedex Health Care Series Drugdex, which is the standard dosing in our ED. Etomidate dosing in our ED is 0.2–0.3mg/kg by our standard protocols. Succinylcholine and etomidate are the standard medications used for rapid sequence intubation (RSI) and were the medications used in all of the ED RSI we examined.
We entered de-identified data into a Microsoft Excel 2003 (Redmond, WA) database. Descriptive statistics, 95 % confidence intervals (CI) and standard deviations (SD) are reported when appropriate. We analyzed data using SPSS14 (Chicago Il.). The study was approved by the hospital institutional review board.
RESULTS
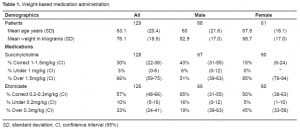
We identified 148 patients as being intubated in our ED during the one-year study period. This represents 2.7 intubations for every 1,000 patients seen. Of these, 129 were included in the analysis. Nineteen patients were excluded due to the absence of a recorded weight and/or medication dosage. Table 1 shows the data by gender. Sixty-one (47%) were female. The mean weight of patients was 82.9 kg (SD:17) for males and 68.7 kg (SD:17) for females. One hundred twenty-eight patients were intubated with succinylcholine. Seventy-seven patients (60% CI: 51–68) were given 120 mg of succinylcholine. Using a range of 1.0–1.5 mg per kg for succinylcholine, only 30% (CI: 22–38) of patients received a dose in the correct range. In the group of patients receiving succinylcholine, four (3%) were underdosed, and two (1.5%) were given less than 0.9mg/kg of succinylcholine. The mean weight of patients with an underdose was 111 kg (CI: 108–114). All of the patients given less than 0.9 mg/kg of succinylcholine were male. Sixty-six percent of patients received an excessive dose of succinylcholine (51% of men and 85% of women). Twenty-four (18%) received more than 2mg/kg of succinylcholine, including six female patients (5%) who received greater than 2.5mg/kg of succinylcholine. The mean weight for the group receiving an excessive dose of succinylcholine was 67 kg (CI: 64–70). Etomidate was given in 126 of 129 intubations. Ninety-five percent of patients (CI: 91–99) were given 20 mg of etomidate. Fifty-seven percent (CI: 48–66) of patients were given a dose of etomidate within the correct range of 0.2–0.3mg per kg. Ten percent (CI: 5–15) were underdosed with etomidate. Three patients (2%) were given a dose of ≤0.15mg/kg of etomidate. The mean weight of a patient with an underdose of etomidate was 102 kg (CI: 98–106). Thirty-five patients (27%) were given an excessive dose of etomidate. The mean weight of those getting an excessive dose of etomidate is 57 kg (CI: 53–61). Seven patients (5%) were given a dose of 0.4mg/kg or higher of etomidate.
DISCUSSION
The process of RSI is common practice in emergency medicine. A key aspect to RSI is administering sedation and paralytic medications. Several studies have demonstrated that ED physicians have poor accuracy when estimating a patient’s weight.1–5 Furthermore, a study by Naguib et al.6 has shown that underdosing succinylcholine can make adequate airway visualization and intubations more difficult. Our study set out to evaluate the accuracy of weight-based paralytic and induction agent dosing in ED patients. As an initial step, we chose to do a retrospective chart review of all ED intubations for a one-year period. Our intubation rate of 2.7 patients per 1,000 ED visits is very similar to prior work showing an ED intubation rate of 2.6 per 1,000 ED visits, which indicates our rate is similar to that of other urban EDs.7 From our data there seems to be little variation in the amount of induction-agent dosing. There also appears to be greater variation in succinylcholine dosing, which may be due to weight estimation.
Although the study was not set up to answer why there was variation, it does describe the presence of that variation in the dosing of paralytics and induction agents. Our data shows that men are more often underdosed, and women are more likely to be overdosed with succinylcholine. Our data shows that succinylcholine was given in doses of 2.5 mg/kg or greater in six patients, all of whom were women. Furthermore, our data also shows that a small percentage of patients were given paralytic doses of less than 0.9 mg/kg. Several studies have shown that adequate to higher dosing of paralytics leads to more optimal intubating conditions.8–10 Leemans et al.10 have shown that higher doses of succinylcholine based on patient actual body weight, not lean body weight or ideal body weight, can lead to more successful intubation conditions. In a patient population with an increasing obesity prevalence, dosing medications on estimated actual body weight could potentially affect patient care and intubating conditions. Our study also provides information on the accuracy of estimated weight-based administration of succinylcholine and etomidate in ED patients. While we did not study the effects of overdosing the amount of succinylcholine, it does help to clarify administration of weight-based medications in the ED. Further studies are needed to evaluate the effect on intubating conditions in the ED when using estimated actual body weights to determine the correct dosing of induction and paralytic medications for RSI.
Having shown the range of overdosing and underdosing of both paralytics and inducation agents in our ED, we believe that further studies should be done to detect difficulties during intubation that could result from this underdosing, including multiple intubation attempts, patient movement during intubation, and patients requiring redosing.
LIMITATIONS
As a single-center retrospective study we are limited in our ability to make general statements based on our study population. As we saw no pediatric patients, we cannot make any inferences about this population. Since there is no central way to identify patients intubated in our ED, we used multiple methods to identify cases; however, there is a chance we could have overlooked a particular group that could alter the outcome. Finally, we do not consider the clinical effects of the dosages administered; thus, a dose judged as inadequate may have been efficacious. Conversely, a dose judged as adequate could have been inadequate.
CONCLUSION
Footnotes
Supervising Section Editor: Brandon K. Wills, DO, MS
Submission history: Submitted October 14, 2009; Revision Received February 10, 2010; Accepted February 24, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Daniel C. McGillicuddy MD, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, One Deaconess Rd. West CC2, Boston, MA, 02215
Email: dmcgilli@bidmc.harvard.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Sanchez LD, Imperato J, Delapena JE, et al. Accuracy of weight estimation by ED personnel. Am J Emerg Med. 2005;23(7):915–6. [PubMed]
2. Menon S, Kelly AM. How accurate is weight estimation in the emergency department? Emerg Med Australas. 2005;17(2):113–6. [PubMed]
3. Hall WL, 2nd, Larkin GL, Trujillo MJ, et al. Errors in weight estimation in the emergency department: comparing performance by providers and patients. J Emerg Med. 2004;27(3):219–24.[PubMed]
4. Anglemyer BL, Hernandez C, Brice JH, et al. The accuracy of visual estimation of body weight in the ED. Am J Emerg Med. 2004;22(7):526–9. [PubMed]
5. Sagarin MJ, Barton ED, Sakles JC, et al. Underdosing of midazolam in emergency endotracheal intubation. Acad Emerg Med. 2003;10(4):329–38. [PubMed]
6. Naguib M, Samarkandi AH, El-Din ME, et al. The dose of succinylcholine required for excellent endotracheal intubating conditions. Anesth Analg. 2006 Jan;102(1):151–5. [PubMed]
7. Wong E, Ng YY. The difficult airway in the emergency department. Int J Emerg Med.2008;1(2):107–11. [PMC free article] [PubMed]
8. Mallon WK, Keim SM, Shoenberg JM, et al. Rocuronium vs. succinylcholine in the emergency department: a critical appraisal. J Emerg Med. 2010;39(3):245–6.
9. Bozeman WP, Kleiner DM, Huggett V. A comparison of rapid-sequence intubation and etomidate-only intubation in the prehospital air medical setting. Prehosp Emerg Care. 2006;10(1):8–13.[PubMed]
10. Lemmens HJ, Brodsky JB. The dose of succinylcholine in morbid obesity. Anesth Analg. 2006 Feb;102(2):438–42. [PubMed]


