| Author | Affiliation |
| Caleb P. Canders, MD | University of California at Los Angeles Medical Center, Department of Emergency Medicine, Los Angeles, California |
| Angela J. Brown, MD | University of California at Los Angeles Medical Center, Department of Emergency Medicine, Los Angeles, California |
| Alan T. Chiem, MD, MPH | Olive View – University of California at Los Angeles Medical Center, Department of Emergency Medicine, Sylmar, California |
CASE
A 27-year-old woman presented with sharp, right lower quadrant abdominal pain for six hours. The pain was colicky, non-migratory, and non-radiating. She reported fevers, anorexia and nausea, and denied dysuria or hematuria. She had no significant past medial history or prior surgeries. Vital signs were notable for a pulse of 110 and an oral temperature of 39.3°C. She had tenderness in her right costovertebral angle and McBurney’s point. She had no rebound or guarding. White count was 16.6 x 109/L and point-of-care urine pregnancy test was negative. Bedside ultrasound with a 10-5Mhz linear transducer was performed at the point of maximal tenderness (Video).
DIAGNOSIS
The elongated and non-compressible tubular structure on ultrasound was initially thought to be the appendix, however an abdominal computed tomography showed right perinephric stranding and ureteritis without evidence of appendicitis. The structure visualized on ultrasound was in fact a dilated and inflamed ureter. Urine analysis revealed 124 white blood cells per high power field. The patient was diagnosed with pyelonephritis, and improved with fluid resuscitation and antibiotics.
Acute appendicitis, the most common abdominal surgical emergency, is a diagnostic challenge, especially in females. Given the perforation rate of 9-35%, an expedited diagnosis is useful to the emergency physician.1-3 Graded compression ultrasound is noninvasive, radiation-free and can be performed at the bedside. Sonographic findings of appendicitis include a non-compressible tubular structure greater than 6mm in the right lower quadrant, increased blood flow on color-flow Doppler, peri-appendiceal fluid, visible appendicolith, prominent pericecal fat and interruption of the submucosa.4 Ultrasound can also be used to make alternative diagnoses, such as ovarian cysts, nephrolithiasis, or pyelonephritis.
However, emergency physician-performed ultrasound for appendicitis is 68-90% specific, with a 75-84% positive-predictive value. When performed by specially trained emergency physicians and radiologists, specificity increases to 78-94%.5-10 Among false-positive appendiceal ultrasound examinations, the most common finding is a non-compressible tubular structure without any other sonographic findings of appendicitis.11 As our case demonstrates, this finding alone may lead to an incorrect diagnosis, and an inflamed and dilated ureter may mimic appendicitis on ultrasound. Additional research to determine the specificity of other sonographic findings, as well as how bedside ultrasonography can be incorporated into clinical decision guidelines for appendicitis, would be of benefit to emergency physicians.
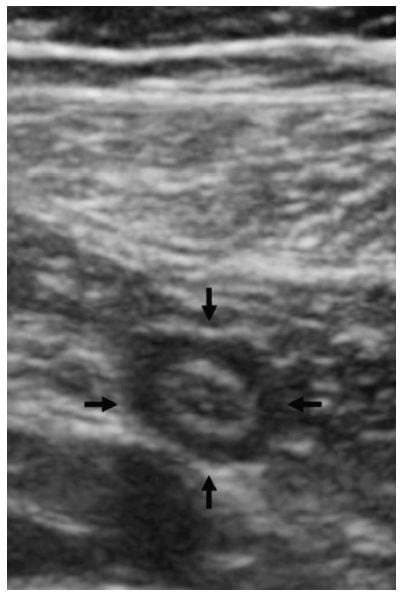
Figure. Cross-section of a tubular structure in the right lower quadrant.
Video. A noncompressible, non-peristalsing tubular structure in the right lower quadrant.
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Caleb Canders, MD, David Geffen School of Medicine at UCLA, 924 Westwood Boulevard, Suite 300, Box 951777, Los Angeles, CA 90095-1777. Email: ccanders@mednet.ucla.edu.
Submission history: Submitted August 16, 2014; Revision received August 21, 2014; Accepted September 23, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Guss DA, Richard C. Comparison of men and women presenting to an ED with acute appendicitis. Am J Emerg Med. 2000;18:372-375.
- Rothrock SG, Green SM, Dobson M, et al. Misdiagnosis of appendicitis in nonpregnant women of childbearing age. J Emerg Med. 1995;13:1-8.
- Jones K, Pena AA, Dunn EL, et al. Are negative appendectomies still acceptable? Am J Surg. 2004;188:748-754.
- Fox JC, Hunt MJ, Zlidenny AM, et al. A retrospective analysis of Emergency Department ultrasound for acute appendicitis. Cal J Emerg Med. 2007;8:41-5.
- Chen SC, Wang HP, Hsu HY, et al. Accuracy of ED sonography in the diagnosis of acute appendicitis. Am J Emerg Med. 2000;18:449–452.
- Brennan GD. Pediatric appendicitis: pathophysiology and appropriate use of diagnostic imaging. CJEM. 2006:8;425-432.
- Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006:1;83-94.
- Fox JC, Solley M, Anderson CL, et al. Prospective evaluation of emergency physician performed bedside ultrasound to detect acute appendicitis. Eur J Emerg Med. 2008:15:80-5.
- Pacharn P, Ying J, Linam LE, et al. Sonography in the evaluation of acute appendicitis: Are negative sonographic findings good enough? J Ultrasound Med. 2010;29:1749-55.
- Pohl D, Golub R, Schwartz GE, et al. Appendiceal ultrasonography performed by nonradiologists: Does it help in the diagnostic process? J Ultrasound Med. 1998;17(4):217-21.
- Trout AT, Sanchez R, Ladino-Torres MF, et al. A critical evaluation of US for the diagnosis of pediatric acute appendicitis in a real-life setting: how can we improve the diagnostic value of sonography? Pediatr Radiol. 2012:42;813-823.


