| Author | Affiliation |
|---|---|
| Unnikrishnan Ponnamma Kunjan Pillai, MD | Wayne State University, Department of Medicine, Detroit, Michigan |
| Krishna Balabhadrapatruni, MD | Wayne State University, Department of Medicine, Detroit, Michigan |
| Jatinder Hothi, MD | Wayne State University, Department of Medicine, Detroit, Michigan |
| Syed Mohsin Raza, MD | Wayne State University, Department of Nephrology, Detroit, Michigan |
| Yahya Osman Malik, MD | Wayne State University, Department of Nephrology, Detroit, Michigan |
An 81-year-old female with history of end stage renal disease on hemodialysis presented with worsening of abdominal pain of 2 days’ duration. The pain started as a dull ache over the lower abdomen 2 months earlier, diffuse but especially prominent over the lower quadrant, and was unrelieved by analgesic medications. On physical examination her whole abdomen was diffusely tender, but the lower quadrant was extremely tender with palpable nodular lesions. Her laboratory work showed a normal amylase and lipase level along with a white cell count of 13.5K/CUMM (3.5–10.6 K/CUMM), calcium of 10.6 mg/dL (8.2–10.6 mg/dL), phosphorus of 5.9 mg/dL (2.3–5.0 mg/dL) and intact PTH 880 pg/mL (18–86 pg/mL).
She had a computed tomography of the abdomen and pelvis (Figure), which showed multiple soft tissue densities in the lower quadrant of anterior abdominal wall, while the ultrasound of her abdomen (Video) revealed subcutaneous nodule with internal septations and calcified vessels. Both these findings in the setting of end stage renal disease were consistent with calciphylaxis, a rare, and often fatal, complication. Although ulceration is considered a hallmark of calciphylaxis, it can also present as non-ulcerative nodular lesions, as in our patient.1 Various putative risk factors for calciphylaxis include obesity; serum aluminum is greater than 25 ng/mL and serum calcium phosphorus product more than 70.2 Treatment is multifaceted, including strict control of secondary hyperparathyroidism, maintenance of calcium phosphate product below 55 mg2/dL2 using non-calcium containing phosphate binders, administration of intravenous sodium thiosulfate with each dialysis (6–12 weeks), and a trial of prednisone tapered over a period of a couple of weeks.1 With the above treatment, she had significant improvement of symptoms. Our case highlights the need for emergency physicians to be cognizant of this life-threatening complication in end stage renal disease patients and of the fact that calciphylaxis has different modes of presentation, among which is acute abdominal pain.
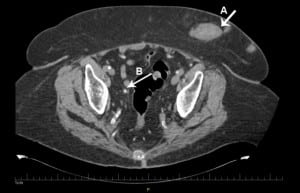
Computed tomography of the abdomen and pelvis without contrast showing multiple soft tissue densities in the anterior abdominal wall (A). Calcification of blood vessels within the abdomen and pelvis was also noted (B).
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted April 30, 2012; Revision received July 17, 2012; Accepted August 3, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.8.12948
Address for Correspondence: Unnikrishnan Ponnamma Kunjan Pillai, MD. Wayne State University, Department of Nephrology, STE 908, Detroit 48201. Email: unnikrishnanpk@yahoo.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Fine A, Zacharias J. Calciphylaxis is usually non-ulcerating: risk factors, outcome and therapy.Kidney Int. 2002 Jun;61(6):2210–2217. [PubMed]
2. Weenig RH, Sewell LD, Davis MD, et al. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56(4):569–579. [PubMed]


