| Author | Affiliation |
|---|---|
| Mark Rosenberg, DO, MBA | Department of Emergency Medicine, St. Joseph’s Health Care System, Paterson, New Jersey |
| Lynne Rosenberg, PhD | Practical Aspects, LLC |
Palliative care initiative
The lsma program
Lessons learned
Future directions
ABSTRACT
An integrated model of palliative care in the emergency department (ED) of an inner city academic teaching center utilized existing hospital resources to reduce hospital length of stay (LOS) and reduce overall cost. Benefits related to resuscitation rates, intensity of care, and patient satisfaction are attributed to the ED-based palliative team’s ability to provide real time consults, and utilize InterQual criteria to admit to a less costly level of care or transfer directly to home or hospice.
Hospice and palliative medicine is the newest subspecialty of emergency medicine (EM), which concentrates on life-threatening illnesses whether they are curable or not. The illnesses may include terminal illness, organ failure, and/or frailty. Palliative medicine represents “the physician component of the interdisciplinary practice of palliative care.”1
Published work on palliative care in the emergency department (ED) is limited yet promising. Research supports the use of palliative care interventions early in the disease trajectory to promote quality of life, as well as reduce costs associated with treatments. 2–5 The ability to change the existing paradigm of care for chronic diseases, such as cardiac or respiratory diseases, stroke, cancer and diabetes, is an opportunity for palliative medicine – specifically palliative care in the ED – to alter the trajectory of care. Many ED palliative care delivery systems have emerged as providers design programs to meet the needs of diverse stakeholders resulting in three recurring models of palliative medicine/care which are ED-palliative care partnerships; ED palliative care champions; and ED hospice partnerships 6
The purpose of this article is to describe one hospital’s approach in expanding the role of the ED staff into palliative and end-of-life care. St. Joseph’s Regional Medical Center (SJRMC) in Paterson, New Jersey, developed a program, Life Sustaining Management and Alternatives (LSMA), to provide palliative consults in their urban ED, using the ED palliative care champion model.
Palliative Care Initiative
SJRMC is a major academic tertiary medical center and state-designated Level 2 trauma center with 651 beds and an annual ED volume of over 135,000 visits. The LSMA program was started by the chair of emergency medicine, boarded in EM and palliative medicine, who championed the palliative care initiative. The primary goal of the LSMA program was to identify those patients who might benefit from palliative care interventions upon entry into the healthcare system. The use of a trigger sheet (Figure 1) assists the staff in identifying patients for real-time palliative consults in the ED.
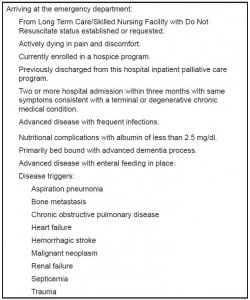
Triggers for emergency department palliative care consult.
Early in the LSMA program, it was recognized that a distinction was needed between palliative care and end of life as both terms were used interchangeably. This same phenomenon has been noted in the literature, representing a barrier to research striving to improve care and support during this time of life.7–9 The LSMA program defines palliative care as “providing palliative treatment while curative treatment is continued and is inclusive of end of life care.” The inclusion of curative treatment is an important distinction that is in contrast to the stereotypical image of palliative care’s association with comfort and death. Palliative care is not to be confused with hospice care in which patients have less than a 6-month life expectancy. Palliative care focuses on the disease trajectories of terminal illness (e.g. cancer), organ failure (e.g. congestive heart failure), and frailty (e.g. Parkinson’s disease).
The LSMA program adheres closely to the World Health Organization’s (WHO) definition and principles for palliative care, intervening as early as possible in the disease process to identify a plan of care that prolongs life while prioritizing the individual patient’s goals.10 End-of-life care, a component of the palliative care program, is defined as the care provided during the last likely hospitalization. It is impossible to know when a person is dying, hence the difficulty in defining end of life. This leaves the concept to regulatory interpretation rather than scientific evidence.9 However, end-of-life care usually encompasses a chronic disease with a progressive downward trajectory.9
The LSMA Program
The chair of the ED and a nurse coordinator initiated the LSMA program within an informal framework, identifying patients for palliative consults when they were working in the ED. While the ED staff had been responsive to multiple initiatives, such as the geriatric ED, resuscitation center, and the toxicology referral center, which have developed into successful programs, there was minimal interest in a palliative care program. Barriers to palliative care in the ED have been well documented and include staff resistance due to the stereotypical association with death, as well as financial barriers from insurance companies.6,11,12
In response, the LSMA program at SJRMC evolved slowly, using each patient’s unique situation to help build the necessary foundation for the acceptance, transition and success of the ED palliative care program. The ED chair set out to expand the role of the ED by identifying patients who would benefit from palliative care, allowing the trajectory of care to be decided at the front end of the hospital stay. It has been recognized that it is beneficial to all for palliative care to start early – preferably on the first day of admission, which may mean starting in the ED itself.1,13
The LSMA program officially started in 2010 when the first ED palliative consult resulted in a male patient being discharged from the ED with home hospice in place. The following month, there were 6 consults in the ED resulting in 5 admissions to medical/surgical units, and 1 discharge from the ED with home hospice in place. As interest in the program grew, any ED staff member could ask for a palliative care consult, resulting in 131 LSMA consults over 16 months between March 2010 and July 2011. Additional consults were performed in-house at the request of the medical staff.
The LSMA program includes a core team of one emergency physician and one master’s prepared nurse coordinator for the initial consult. Additional member involvement from the interdisciplinary team is determined by the plan of care. Other key members include nurses, nutritionists, chaplains, psychologists, social workers, physical therapists, occupational therapists, and other disciplines as required meeting the needs of each patient and family. Distinguishing itself from most other ED palliative programs, the LSMA program is open to all ages, including children. SJRMC has a pediatric ED with vast resources available to this population with a special focus on cancer trajectories.
Initial consultations range from a general introduction to in-depth communications regarding advanced directives and treatment plans. Consultations average 15 to 30 minutes or longer depending upon the patient/family circumstances. During the week, Monday through Friday from 7am to 6pm, consultations are within 30 minutes. Telephone consultation is available 24/7; the patient is seen the following morning if further follow up is needed.
Of utmost importance is the determination of the patient goals as early as possible, including discussions of “do not resuscitate” (DNR) status as appropriate to the individual patient.13 Most hospital settings, including SJRMC, continue to use DNR terminology even as competing terms, such as “do not attempt resuscitation” (DNAR) and “allow natural death” (AND), receive endorsement from the American Heart Association and the American Nurses Association.14,15 Regardless of the specific terminology chosen by an institution or provider, the patient’s resuscitation goals and choices need to be clearly understood by the patient, his family, and healthcare providers.14 The LSMA consults resulted in 73 of 131 (56%) patients initiating DNR orders in the ED (Figure 2). The LSMA program has not had an impact on the number of inpatient consultations for the inpatient palliative care service at SJRMC. This may suggest that the implementation of the LSMA program has identified a new subset of patients reflecting similar experiences noted in the literature.16
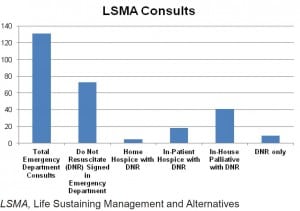
Emergency department palliative care consults March 2010 to July 2011 (n = 131).
Benefits of the LSMA program have been numerous, extending beyond the patient and their families to the ED and hospital staff. First and foremost, the patient’s wishes are supported and carried out throughout the plan of care. The interdisciplinary team focuses on open communication to attain symptom management, choice of interventions and the treatment plan. General benefits include reducing hospital length of stay (LOS) and reduction of overall cost, which is well documented in the literature.17,18
Specifically, the LSMA program has provided benefits related to resuscitation rates, intensity of care and patient satisfaction. Some patients with “end of life” diagnoses have chosen not to have cardiac resuscitation if needed since it did not support their goals of care, thereby impacting overall resuscitation rates in the hospital. There are cost savings as a benefit of providing the appropriate level of service for the palliative patient in terms of level of care, support of disease trajectory and patient/family choices. ICU costs are associated with approximately 20% of overall hospital costs.5 InterQual level of care criteria for acute care was used to evaluate intensity of service and best location of care for patient consults in the LSMA program. InterQual is a medical necessity-screening tool used to determine if a hospital admission is medically necessary by correlating a patient’s severity of illness with intensity of care.19,20 Over one-half (57%) of all LSMA consult patients who were admitted to medical surgical units (lowest level of hospital inpatient care) met criteria for a higher level of care, either critical care or step-down. Of those LSMA patients discharged from the ED, 62% met admission criteria, with 50% of this cohort meeting critical care admission criteria. The decision to discharge or admit to a lower level of care was in accordance with the patient’s stated goals of care and advanced directives. All told, 48 of 131 (37%) LSMA patients were cared for at a lower level (presumably lower cost), than would likely have resulted without the LSMA program.
Billing for the consultation service varies on insurer and contracts. The coding and billing can be done using ED visit codes or initial hospital codes – whichever is more appropriate based on the patient’s disposition. Revenue for the service varies, but based on volume of consultations this service potentially can be self-sustaining.
Lessons Learned
The LSMA program grew from existing hospital resources. Currently, the program continues with the chair and nurse coordinator providing ED and in-house consults. These two positions (chair and nurse coordinator) are considered critical to the development of any ED-based program. It is essential to know the staff and community as well as nuances of the hospital in terms of leadership, internal politics and resources before designing an ED-based palliative care program. It is recommended that any ED-based program provide real-time consults, which has been a large part of the success of the LSMA program. As noted in the literature, contact with the patient and family on the first date of service provides the best opportunity to impact the plan of care.21
Education and certification of staff is an ongoing necessity including continual review of the literature. The development and maintenance of a data log are required to provide statistical evidence for over-site review, board and committee updates and to identify quality indicators for monitoring. The data log includes: date of service, medical record number, age, and gender. Quality indicators include: Reason for ED visit, reason for palliative consult, hospice referral, DNR status, and admission or discharge status.
Lastly and most importantly, an advocate of the palliative care program is needed (preferably an ED physician) who possesses the ability to work behind the scenes educating, recruiting, addressing barriers and promoting inclusion and continuity of the program within the individual hospital structure. The advocate becomes critical to the success and growth of the program. The LSMA program has survived the construction of a new 88-bed ED, as well as various personnel changes including the departure of the primary nurse coordinator. Implementing the LSMA program has met a variety of challenges in developing transition of care plans between the ED, inpatient and outpatient for multiple medical services while remaining responsive to the needs of this patient cohort and changing paradigm of care.
Future Directions
The LSMA focus has been on identifying patients for the palliative care program, providing both end-of-life and palliative consults. In the future, the emphasis will be on the transition of care and continuity throughout the hospital stay and patient discharge. This involves identifying a mechanism to follow-up with each ED palliative consult in 48 hours to define the plan of care. Currently, the LSMA team is strictly ED based and is working with hospital staff in establishing the continuity of care regardless of the patient’s disposition. Continuity of care and the role of the ED-based palliative program needs to be integrated with in-house and out-of-house patient transitions.
The staff will assist in identifying the main reason for ED visits for those in palliative care, which studies suggest are related to symptoms of pain, nausea, vomiting, constipation and shortness of breath.22 Emergency medical service protocols, time trial therapy and heart failure patients specifically will be monitored.
Above all, each palliative care team member is an advocate for this vulnerable population, reaching out to discover innovations and advancements in this growing specialty of care. Change is a slow process and the growth of any new program is arduous. However the LSMA program is impacting the delivery of care one medical resident at a time, one patient at a time, one person at a time.
Footnotes
Address for Correspondence: Mark Rosenberg, DO, MBA. Department of Emergency Medicine, St. Joseph’s Health Care System, Paterson, NJ. Email: mark.emergency@gmail.com. 11 / 2013; 14:633 – 636
Submission history: Revision received November 3, 2012; Submitted May 5, 2013; Accepted May 6, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.


