| Author | Affiliations |
| Kristi L. Koenig, MD | University of California at Irvine, Center for Disaster Medical Sciences and Department of Emergency Medicine, Orange, California |
| Cassondra Majestic, MD | University of California at Irvine, Center for Disaster Medical Sciences and Department of Emergency Medicine, Orange, California |
| Michael J. Burns, MD | University of California at Irvine, Department of Emergency Medicine and Department of Medicine, Division of Infectious Diseases, Orange, California |
ABSTRACT
Ebola Virus Disease (EVD) has become a public health emergency of international concern. The World Health Organization and Centers for Disease Control and Prevention have developed guidance to educate and inform healthcare workers and travelers worldwide. Symptoms of EVD include abrupt onset of fever, myalgias, and headache in the early phase, followed by vomiting, diarrhea and possible progression to hemorrhagic rash, life-threatening bleeding, and multi-organ failure in the later phase. The disease is not transmitted via airborne spread like influenza, but rather from person-to-person, or animal to person, via direct contact with bodily fluids or blood. It is crucial that emergency physicians be educated on disease presentation and how to generate a timely and accurate differential diagnosis that includes exotic diseases in the appropriate patient population. A patient should be evaluated for EVD when both suggestive symptoms, including unexplained hemorrhage, AND risk factors within 3 weeks prior, such as travel to an endemic area, direct handling of animals from outbreak areas, or ingestion of fruit or other uncooked foods contaminated with bat feces containing the virus are present. There are experimental therapies for treatment of EVD virus; however the mainstay of therapy is supportive care. Emergency department personnel on the frontlines must be prepared to rapidly identify and isolate febrile travelers if indicated. All healthcare workers involved in care of EVD patients should wear personal protective equipment. Despite the intense media focus on EVD rather than other threats, emergency physicians must master and follow essential public health principles for management of all infectious diseases. This includes not only identification and treatment of individuals, but also protection of healthcare workers and prevention of spread, keeping in mind the possibility of other more common disease processes. [West J Emerg Med. 2014;15(7):728–731.]
On August 8, 2014, the World Health Organization (WHO) declared the Ebola outbreak in West Africa a public health emergency of international concern, noting that all nations “should be prepared to detect, investigate, and manage Ebola cases.” Enormous media attention and public health resources have been expended, yet the average clinician will never see a case. To complicate matters, as was seen in the 2009 H1N1 pandemic, authoritative bodies such as WHO and the U.S. Centers for Disease Control and Prevention (CDC) may issue conflicting recommendations during these types of evolving public health emergencies, e.g., no travel restrictions versus limiting travel to West Africa. In addition, in a global environment, international policy makers have made seemingly contradictory statements to include that, “the threat from Ebola is vastly underestimated” while also suggesting that “the threat to the U.S. is extremely small.” Nevertheless, the basic principles of management of a febrile traveler are essential competencies for physicians worldwide, in particular emergency physicians on the frontlines, who are often the first to encounter an acutely ill patient. These standards will remain important even as Ebola Virus Disease (EVD) fades and the next infectious disease emerges.
According to CDC, as of September 25, 2014, there have been at least 6,263 suspected and confirmed cases and 2,917 suspected case deaths across five countries in West Africa, and the numbers continue to grow.1 This is the first recorded outbreak of Ebola in West Africa and the largest outbreak ever documented. EVD is an often-fatal disease (mortality rate 50%-70%) that is spread from person-to-person or animal to person via direct contact with bodily fluids or blood. The infectious dose is ≤10 viral particles. The incubation period ranges from 2-21 days (average 5-6 days). Early symptoms include abrupt onset of fever, myalgias, and headache. Vomiting, diarrhea and abdominal pain follow in 1 to 2 days, often progressing to hemorrhagic rash and life-threatening bleeding and multi-organ failure (acute respiratory, liver and renal) within a few days.2 Laboratory findings include thrombocytopenia, leukopenia, and elevation in liver function enzymes. The disease is not transmissible until the patient is symptomatic, but continues to be contagious, even postmortem. A patient should be evaluated for EVD with both suggestive symptoms including unexplained hemorrhage, AND risk factors within 3 weeks prior, such as travel to an endemic area, direct handling of animals from outbreak areas, or ingestion of fruit or other uncooked foods contaminated with bat feces containing the virus are present.2
Current treatment of EVD is mainly supportive. This includes early implementation of intravenous fluids (or oral rehydration) and maintenance of adequate electrolyte balance, oxygen therapy, blood pressure control, and treatment of other infections if they occur.2 The clinician should also consider ordering additional lab studies such as complete blood count, complete metabolic panel, coagulation factors, and type and cross or type and screen in cases with concern for hemorrhage.
Viremia develops after the fever. It may take up to 72 hours to confirm the diagnosis by laboratory testing.3 Early diagnosis is confirmed by obtaining a blood sample that is tested for viral antigens by antigen-capture enzyme-linked immunosorbent assay or polymerase chain reaction in the lab. Later in the disease course, antibodies for the virus such as IgM and IgG, can also be detected.4 If testing is indicated, local and state health departments should be notified immediately. CDC recommends that healthcare providers collect serum, plasma, or whole blood samples of at least 4 mL, to be shipped refrigerated or on ice to the appropriate health department for further testing.2
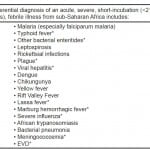
Physicians must be vigilant in the clinical workup of febrile travelers, especially important in the emergency department during the initial workup of disease. A timely and accurate differential diagnosis including exotic diseases, is essential. Knowledge of disease risk by geographic area is critical to evaluation of the traveler who returns ill. This will help guide the decision making of clinicians to order appropriate tests and treatment.5 The likelihood of encountering a patient with EVD outside of the region of the outbreak is small. Returning travelers often do not have an exotic tropical infection as the cause of their illness. Instead they may have influenza, streptococcal pharyngitis, pneumococcal pneumonia, pyelonephritis, or other uncommon infectious diseases with hemorrhagic manifestations including meningococcemia, Staphylococcus aureus bacteremia, or rickettsial infections. Despite the low likelihood of encountering a patient with severe febrile illness, travelers may acquire unusual infections that are unfamiliar to most healthcare staff.5 Clinicians should develop an appropriate list of differential diagnoses, taking travel history into consideration (Figure 1).
Figure 1. Differential diagnosis of he febrile traveler.
Infections found in sub-Saharan Africa having incubation periods >21 days should be considered if the patient has stayed in the endemic area for some time, including acute HIV infection*, African trypanosomiasis, brucellosis, filariasis (various types), malaria, secondary syphilis*, visceral leishmaniasis, acute schistosomiasis, amebic liver abscess, viral hepatitis*, rabies*, tuberculosis*, and melioidosis.
* Transmissible from person-to-person.
Many of these diseases present non-specifically, often with fever and malaise. In advanced cases, hemorrhage is common, but may be present in only about 50% of EVD cases. There have been at least 20 suspected cases of EVD in the U.S.; however, only about one-fifth of these cases met criteria for testing. Nevertheless, these suspected cases drain limited healthcare resources because of the heightened concern for EVD. Some of the patients ultimately had malaria and influenza.1
On September 30, 2014, CDC Director Dr. Tom Frieden announced at a national press conference that a visitor to the U.S. has been diagnosed with Ebola at a hospital in Dallas, Texas. This is the first person to be diagnosed in the U.S. after arrival here from an endemic area. He reportedly arrived 10 days earlier by air from Liberia and did not develop fever or other symptoms until 4-5 days later. He reportedly was initially seen at a healthcare facility when he first became symptomatic but was not isolated, not tested for Ebola, and was sent home. He was admitted to a Dallas hospital a few days later, placed in isolation, and viral testing confirmed Ebola.
If there is suspicion for a transmissible pathogen based on the patient’s travel history and symptoms, the patient should be isolated immediately in a single-patient room with standard and droplet precautions. Only essential personnel should enter; medical equipment should be disposable. Despite what is shown with high-profile media cases, gloves, gowns, goggles, and a fluid resistant face mask to cover the nose and mouth are generally adequate for personal protective equipment (PPE). If copious amounts of blood, emesis or diarrhea are present, higher levels of PPE, e.g., double gloving, shoe and leg covers should be added. Aerosol-generating procedures should be avoided, but higher-level respiratory protection is required if these procedures must be performed.6 This includes isolating the patient in a negative pressure room with the use of N95 respirators or possibly powered air purifying respirators (PAPR) utilized by staff caring for the patient. Ensure that all laboratory samples are transported in person rather than using tubing systems, and notify laboratory personnel regarding the possible infectious nature of the samples. Avoidance of the tube system is necessary in attempt to avoid damage of the tubes en route and risk of any viral sample aerosolizing. Blood draws in these high-risk patients should also be minimized to reduce the risk of needle sticks in hospital personnel.
Contacting the local health department and state, national, and international authorities if necessary is an essential step in care of these types of patients. The U.S. CDC classifies EVD as a category A bioterrorism agent; thus, these notifications should include law enforcement for suspicious circumstances.7 In general, bioterrorism should be considered as a causative factor in an infectious disease case when: 1) there is a single suspected case of an uncommon disease, 2) similar disease is clustered in different locales but within the same time frame, 3) there is an unusual clinical, geographical, or seasonal presentation, or 4) there are increased deaths in an animal population.
There are therapeutic agents that may be available from CDC, such as the investigational new drug artesunate in a malaria patient. Emergency Use Authorization authority in the U.S. allows the Food and Drug Administration (FDA) commissioner to approve medical agents to be used for diagnosis, therapy, or prevention of disease when they are not the standard of care or supported by research that proves their safety.8 This is exemplified in the recent cases of EVD, for which the two infected U.S. citizens received ZMapp, monoclonal antibodies produced in specially modified tobacco plants.9 The FDA is reportedly permitting a second experimental drug, TKM-Ebola, to be used in infected patients. Although CDC, NIH and other federal agencies are working to produce a vaccine and continue production of these experimental therapies, supportive care remains the current standard treatment.10
With dozens of emerging infections identified each year,11 it is essential for physicians to avoid undue influence from current media attention on a single disease and focus on implementation of systems and education and training on general principles that extend to all such situations. Additional issues to consider include: 1) planning for healthcare worker absenteeism (ill/dead, caring for loved ones, afraid or unable to come to work); and 2) being familiar with EVD in order to identify suspected cases, consider the differential diagnosis, and also to reassure patients seeking care who are concerned about the disease due to the media hype.
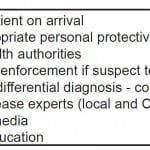
The current globalization of healthcare, including rapid international travel, climate change, economic development, and environmental and agricultural practices, means that microbial threats to the population have increased. Nevertheless, countries with modern healthcare facilities are well equipped to manage febrile travelers and limit disease spread if clinicians follow appropriate guidelines (Figure 2). These basic principles are valid for every infectious disease. A case could be made that the threat from seasonal influenza, with approximately 36,000 deaths per year in the U.S. alone and rapid airborne transmission potentially even before a patient is symptomatic, is as great or greater than that from EVD. Regardless of the perspective, the listed actions are critical competencies for all emergency physicians in order to manage both the threat from EVD and the next big thing, whatever emerging infectious disease that might be.
Figure 2. Critical actions for emergency physicians caring for febrile travelers who might have Ebola or other infections transmitted from person-to-person.
CDC, Centers for Disease Control and Prevention
Footnotes
Supervising Section Editor: Gregory Moore, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Kristi L. Koenig, MD. Center for Disaster Medical Sciences, Department of Emergency Medicine, UC Irvine Medical Center, 101 The City Dr. South, Route 128, Orange, CA 92868. E-mail: kkoenig@uci.edu.
Submission history: Submitted August 20, 2014; Revision received October 19, 2014; Accepted November 12, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Centers for Disease Control and Prevention. 2014 Ebola Outbreak in West Africa. Available at: http://www.cdc.gov/vhf/ebola/outbreaks/guinea/index.html. Accessed Aug 18, 2014.
- Centers for Disease Control and Prevention. Treatment, Sept 19, 2014. Available at: http://www.cdc.gov/vhf/ebola/treatment/index.html. Accessed Sept 21, 2014.
- Centers for Disease Control and Prevention. Guidelines for Evaluation of US Patients Suspected of Having Ebola Virus Disease, Aug 1, 2014. Available at: http://emergency.cdc.gov/han/han00364.asp. Accessed Sept 21, 2014.
- Centers for Disease Control and Prevention. Diagnosis, Aug 5, 2014. Available at: http://www.cdc.gov/vhf/ebola/diagnosis/index.html. Accessed Aug 18, 2014.
- Wilson ME, Weld LH, Boggild A, et al. Fever in returned travelers: results from the GeoSentinal Surveillance Network. Clin Infect Dis. 2007;44:1560-1568.
- Centers for Disease Control and Prevention. Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Hemorrhagic Fever in U.S. Hospitals, 2014. Available at: http://www.cdc.gov/vhf/ebola/hcp/infection-prevention-and-control-recommendations.html. Accessed August 21, 2014.
- Centers for Disease Control and Prevention. Bioterrorism Agents/Diseases, 2014. Available at: http://www.bt.cdc.gov/agent/agentlist-category.asp. Accessed Aug 21, 2014.
- United States Food and Drug Administration. Emergency Use Authorization of Medical Products, 2007. Available at: http://www.fda.gov/regulatoryinformation/guidances/ucm125127.htm#.U-D_lUFoFkk.email. Accessed Aug 18, 2014.
- Centers for Disease Control and Prevention. Questions and Answers on Experimental Treatments and Vaccines for Ebola. 2014. Available at: at http://www.cdc.gov/vhf/ebola/outbreaks/guinea/qa-experimental-treatments.html. Accessed Sept 20, 2014.
- American College of Emergency Physicians. Healthcare Resources for Suspected Ebola Cases, 2014. Available at: http://www.acep.org/ebola. Accessed Aug18, 2014.
- Gamage SD, Kralovic SM, Roselle GA. Emerging infectious diseases: concepts in preparing for and responding to the next microbial threat. Chapter 6 in: Koenig KL, Schultz CH (eds.): Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices. Cambridge University Press, American College of Emergency Physicians, 2010.