| Author | Affiliation |
|---|---|
| Parveen Parmar, MD, MPH | Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts |
| Craig A. Goolsby, MD | Uniformed Services University of the Health Sciences, Bethesda, Maryland |
| Kavid Udompanyanan, MD | Kaiser Santa Clara, Stanford/Kaiser Emergency Medicine Residency, Santa Clara, California |
| Leslie D. Matesick, DO | Wilford Hall Medical Center, San Antonio, Texas |
| Kirk P. Burgamy, MD | Cedars-Sinai Medical Center, Los Angeles, California |
| William R. Mower, MD, PhD | University of California, Los Angeles Emergency Medicine Center, University of California Geffen School of Medicine, Los Angeles, California |
ABSTRACT
Introduction:
Laboratory and radiographic studies are often required by psychiatric services prior to admitting emergency patients who are otherwise deemed medically stable. Such testing may represent an unnecessary expense that prolongs emergency department stays without significantly improving care. This study determines the prevalence of such testing and how often it leads to changes in care.
Methods:
We prospectively tracked laboratory testing among psychiatric patients presenting to the emergency departments of two academic tertiary care facilities. For each visit we determined whether laboratory or radiographic studies were ordered, and whether the examination was conducted at the request of the emergency physician as part of a medical screening examination or requested by the psychiatry service. We then determined if this testing changed patient disposition.
Results:
Our study enrolled 598 patients. Of these, emergency physicians ordered testing as a part of medical screening on 155 patients (25.9%). We found the psychiatry service ordered laboratory or radiographic studies for 191 of 434 patients (44.0%) who emergency physicians determined did not require ancillary testing for medical clearance. Of these 191 patients, only one (0.5%; 95% Confidence Interval: 0.01% – 2.9%) had an abnormal result that led to a change in disposition. Total Medicare reimbursement rates for the additional ancillary testing in this study was $37,682.
Conclusion:
Ancillary testing beyond what is required for medical clearance of psychiatric emergency patients rarely alters care. Policies that require panels of testing prior to psychiatric admission are costly and appear to be unnecessary.
INTRODUCTION
Patients with psychiatric complaints comprised 5.4% of all visits to U.S. emergency departments (ED) in the year 2000. Emergency psychiatric visits appear to be increasing over time, and patients with psychiatric complaints are more likely to require hospitalization than non-psychiatric patients.1
Many of these patients undergo laboratory and radiologic testing as part of their medical screening prior to psychiatric evaluation. Most recommendations for routine screening stem from expert opinion and case series and are often based on medical screening performed by psychiatrists, not emergency physicians (EP).2–8 EPs are uniquely trained to evaluate a variety of patients and rapidly determine the presence of serious medical illness, even among those with limited ability to effectively communicate. In daily practice, EPs often complete their evaluations and determine patient dispositions without using laboratory or radiologic testing.
In modern practice environments, resource optimization, patient safety and throughput are increasingly important. Streamlined patient testing could improve patient care and potentially decompress overcrowded EDs. Critics of mandatory testing cite wasted money, time and the potential patient harm from false test results, while proponents think psychiatric patients represent a vulnerable population that is impossible to evaluate on the basis of history and physical examination alone.
From this perspective it is unclear whether mandatory ancillary testing of psychiatric patients is useful or beneficial. Several retrospective studies suggest that screening labs are unlikely to reveal significant medical problems once a physician has determined, based on history and physical exam, that a psychiatric patient is medically stable for admission to a psychiatric facility.9–16 A study by Korn et al concluded that patients with a psychiatric chief complaint, normal physical exam and documented psychiatric history may be safely referred to psychiatric services without the use of ancillary ED testing.16
Previous work in this area has been limited to case series and retrospective analyses.2,4,8,10,11,16 In this study, we sought to prospectively determine the effect that mandatory ancillary testing has on the disposition of psychiatric patients. We hypothesized that ancillary testing does not alter the disposition of patients with psychiatric disease who have been deemed medically stable for admission to a psychiatric facility by an EP. We hypothesized that a careful history and physical examination by an EP can determine which patients require studies prior to medical clearance, and which patients can be safely admitted without further testing. Our primary outcome measure was the proportion of dispositions among psychiatric patients that changed from psychiatric ward to admission elsewhere in the hospital based on screening studies.
As secondary outcomes, we collected data on the types and numbers of laboratory and radiographic studies performed. We also looked at how frequently tests were performed and the costs for these screening tests.
METHODS
Study Design
This was a multi-center, prospective observational study.
Setting
We conducted our study in the EDs of two academic tertiary centers: Ronald Reagan-University of California, Los Angeles Medical Center (UCLA) in Los Angeles, California, and Wilford Hall Medical Center (WHMC) at Lackland Air Force Base in San Antonio, Texas. Both hospitals have inpatient psychiatric wards and ED consultation by psychiatry residents available 24 hours/day. Ronald Regan-UCLA serves a diverse, urban patient population located in west Los Angeles with an annual volume of about 40,000 patients. WHMC has an annual volume of about 50,000 patients and serves a military population, which includes active duty troops from all services, activated reservists and National Guard troops, a large retiree population, family members of all ages, and civilians who either have base access or arrive via ambulance for medical or traumatic emergencies.
Selection of Participants
We conducted the study from June 15, 2008 to July 15, 2009 at UCLA and from December 17, 2008 to July 5, 2009 at WHMC. To ensure that our study achieved a power of 98%, we continuously enrolled patients until we had obtained data on 183 cases. Patients with a psychiatric chief complaint, as determined by the examining EP, were eligible for enrollment. The physician was not limited to a specific complaint list, or specific diagnostic codes, but rather instructed to enroll patients they thought had a primary psychiatric complaint as the reason for their presentation. We conducted the study using convenience sampling where all EPs (both residents and attendings) participated in data collection and enrollment at the WHMC ED, while 12 residents (under direct attending supervision) and one attending EP collected data in the UCLA ED during the course of their normal shifts.
Outcome Measures
Our primary outcome measure was the proportion of dispositions that changed as a consequence of ancillary testing in patients who had received medical clearance. We therefore tabulated the number of patients with primary psychiatric complaints who were deemed medically clear for psychiatric admission (our denominator), as well as the subset of these patients who underwent further laboratory or radiographic testing. From among patients who received further testing, we recorded the number who had their disposition changed from psychiatric service to admission under another hospital service (our numerator).
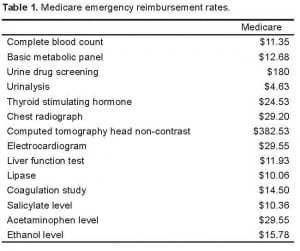
We also tabulated the types and numbers of laboratory and radiographic tests ordered on enrollees, as well as Medicare reimbursement charges for these tests (Table 1).
Method of Measurement and Data Collection
Physicians completed an initial history and physical examination on each patient, and based on this assessment determined whether or not laboratory or radiographic testing was indicated should the patient require inpatient psychiatric admission. We excluded all patients that the EPs thought required testing prior to psychiatric admission.
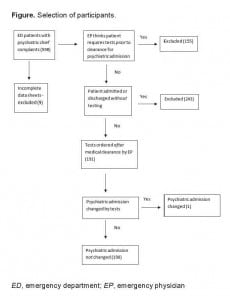
For patients whom the EP felt could be safely admitted without testing, the physician recorded whether or not tests were ordered, and, if so, which ones. Physicians also recorded whether the patient was admitted to a service other than psychiatry, and if so, whether laboratory or radiology studies led to this change in disposition. We excluded any incomplete data sheets from the study (Figure).
We did not collect any identifying information on enrolled patients or enrolling physicians, and our study did not require a change in usual care of any enrolled patients. Our study was reviewed and approved by the UCLA and WHMC Institutional Research Boards.
RESULTS
We collected 598 data sheets during the study (504 UCLA, 94 WHMC (Table 1). Nine patients (1.5% of the total; 6 UCLA, 3 WHMC) had incomplete forms and were excluded. EPs determined that 155 patients (134 UCLA, 21 WHMC) required laboratory or radiographic testing prior to admission and could not be medically cleared based on history and physical examination alone. Laboratory or radiographic testing was obtained on 191 of the remaining 434 patients deemed medically stable for psychiatric admission (44.0%; 95% Confidence Interval (CI): 39.3% – 48.8%). Only one of these 191 patients (0.5%; 95% CI: 0.01 – 2.9%) was found to have an abnormal study that led to a change in disposition. The sole screening study that resulted in a change in admission was an abnormal acetaminophen level that prompted admission to a medical ward for N-acetylcysteine treatment.
Table 2 presents the number of laboratory and imaging studies performed on patients deemed medically clear. The most frequently ordered studies were complete blood count, blood chemistries and urine drug screens. Other frequently ordered tests included measuring specific levels for alcohol, acetaminophen, aspirin, and thyroid-stimulating hormone. Tests that were infrequently ordered included chest radiographs, computed tomography (CT) of the head, lipase, and coagulation studies. The total monetary impact of all labs, based on Medicare reimbursement rates, was $37,682. The average charge per patient for these studies was $197.29.
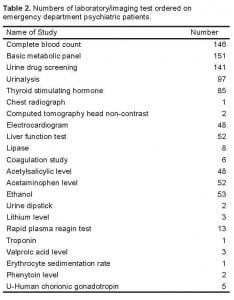
Numbers of laboratory/imaging test ordered on emergency department psychiatric patients.
DISCUSSION
Psychiatric patients present unique challenges for emergency care, with one of the foremost problems involving the optimal way to assess whether these patients are suitable for admission to psychiatric facilities. Prior literature regarding this clearance process consists largely of expert opinion and retrospective analysis. Our study advances understanding in this area by providing prospective data to this body of literature, and specifically focuses on whether mandatory test panels change disposition after EPs have cleared a psychiatric patient for admission by history and physical exam.
This multi-center study overwhelmingly demonstrates that routine or mandatory studies do not change the disposition of psychiatric patients after EPs have cleared them for admission. Of the 191 patients evaluated in this study, only one (0.52%) patient’s disposition was changed by additional tests.
With only 1 exception, none of the studies performed on medically cleared patients, including complete blood count and blood chemistries, alcohol levels, urine drug screens, aspirin levels, thyroid-stimulating hormone levels, electrocardiograms, urinalysis, chest radiographs, CT scans of the head, liver function tests, lipase, or coagulation studies, altered a patient’s disposition. The one test that did change a disposition, a positive acetaminophen level that led to medical admission for N-acetylcysteine treatment, was a focused evaluation that addressed a specific medical question that can be difficult to assess by history or physical examination in some patients. Unlike most pathologies affecting psychiatric patients, such as salicylate toxicity, infection, or trauma, early acetaminophen overdose may present with no toxidrome—normal vitals and physical exam—and few historical clues. If the patient lies about the ingestion, acetaminophen overdose could go clinically undetected even with a diligent EP’s history and physical exam. Missing an acetaminophen overdose could lead to a poor patient outcome. This suggests that one means of optimizing screening tests for psychiatric patients, and a possible future strategy, would be to mandate acetaminophen levels on suicidal patients, while eliminating other testing that is unlikely to impact disposition or management.
Our study suggests extensive routine screening studies for all psychiatric patients are likely unnecessary, and that EPs are very unlikely to change a psychiatric patient’s disposition after clearing them with a history and physical examination. Future studies examining other populations could help validate this conclusion for a wider spectrum of ED environments.
Our study also reveals that mandatory testing leads to significant expense. The relatively small group of patients evaluated at two centers accounted for $37,682 in tests. The charges would be significantly larger for patients with private insurance, or patients receiving a direct bill from a hospital. Remarkably, more than $25,000 was spent on urine drug screens (Table 3). The combination of how commonly this test was ordered and its high cost ($180) made it responsible for the highest percentage of costs attributed to one test. Furthermore, these drug screens never led to a change in patient disposition. While these tests may be useful in the overall management of specific patients, there is no reason they need to be performed in the ED.14 It therefore appears reasonable to curtail the mandatory use of urine drug screens when evaluating ways to optimize patient testing prior to psychiatric admission.
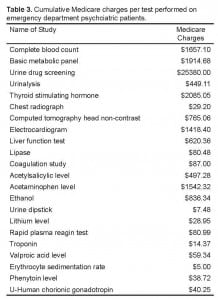
Cumulative Medicare charges per test performed on emergency department psychciatric patients.
A key assumption is that the EP conducts a thorough history and physical. If the EP feels a thorough assessment cannot be conducted, or there are high-risk features for organic illness, testing may prove useful.4,17 Indeed, EPs thought 155 of the original 598 patients in the study required testing prior to medical clearance. The clinical judgment of the treating physician, rather than panels of routine tests, may more efficiently and appropriately guide this work-up.4 Further studies could analyze the cost effectiveness and patient safety outcomes of this notion.
In summary, routine testing of patients medically cleared for psychiatric admission by an EP’s history and physical rarely changes disposition. EPs and psychiatrists should work together to develop appropriate, cost-effective, testing strategies for admitting emergency psychiatric patients.
LIMITATIONS
We conducted this study at two tertiary care academic hospitals with residency programs. Consequently, our findings will be most relevant to similar institutions and may not translate directly to smaller or community EDs. Additionally, one of our sites is an Air Force hospital that treats patients of all ages, with all medical problems and levels of acuity (including Level 1 traumas), but the active duty population tends to be relatively young and healthy, which may not mirror other ED populations. These factors likely skew our results to the populations seen in these institutions, but probably have little effect on the ability of ED physicians to accurately screen psychiatric patients for underlying acute medical problems. Thus, while our population may not be representative of all institutions, we believe that our observations regarding testing on medically cleared patients are likely to be applicable to a wide variety of settings.
We used non-randomized convenience sampling to assemble our cohort. We instructed physicians to gather data on all patients meeting enrollment criteria, but we did not track compliance. It is therefore possible that some eligible patients were not enrolled in the study. It is likely that missed enrollment occurred during times when the EDs were busy and clinical demands made it difficult for physicians to complete data collection in a timely fashion. While it is possible that this limitation could result in biased selection of patients, or altered the medical assessments of psychiatric patients, there is little reason to believe this actually occurred. There is also little reason to suspect that patients who were medically cleared without laboratory testing, but not included in the study, would be more likely than enrolled patients to have abnormal results that would require changes in admission.
Our calculated financial impacts included only Medicare reimbursements. The more elusive, and likely higher, costs of time spent in the ED, and additional nursing and physician care have not been included. Additionally, these financial impacts do not reflect the charges that patients may receive from a particular hospital, which could be much higher, nor do they reflect the actual costs of the tests themselves, which could be lower.
Finally, because we conducted an observational study, we did not blind ED physicians to diagnostic test ordering or patient outcomes. This lack of blinding is unlikely to be a source of bias because the physicians who made decisions regarding testing and admission, the evaluating psychiatrists, were unaware of the study.
Footnotes
Supervising Section Editor: Lesie Zun, MD, MBA
Submission history: Submitted March 25, 2011; Revision received August 31, 2011; Accepted January 11, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.1.6754
Address for Correspondence: Parveen Parmar, MD, MPH, Brigham and Women’s Hospital, 75 Francis St, Boston, MA 02115
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Hazlett SB, McCarthy ML, Loudner MS, et al. Epidemiology of Adult Psychiatric Visits to U.S. Emergency Departments. Acad Emerg Med. 2004;11:193–5. [PubMed]
2. Hatta K, Takahashi T, Nakamura H, et al. Abnormal physiological conditions in acute schizophrenic patients on emergency admission: dehydration, hypokalemia, leukocytosis and elevated serum muscle enzymes. Eur Arch Psychiatry Clin Neurosci. 1998;248:180–8. [PubMed]
3. Lagomasino I, Daly R, Stoudemire A. Medical assessment of patients presenting with psychiatric symptoms in the emergency setting. Psychiatr Clin North Am.1999;22:819–50. viii–ix. [PubMed]
4. Reeves RR, Pendarvis EJ, Kimble R. Unrecognized medical emergencies admitted to psychiatric units. Am J Emerg Med. 2000;18:390–3. [PubMed]
5. Williams ER, Shepherd SM. Medical clearance of psychiatric patients. Emerg Med Clin North Am. 2000;18:185–98. vii. [PubMed]
6. Hall RC, Gardner ER, Popkin MK, Lecann AF, Stickney SK. Unrecognized physical illness prompting psychiatric admission: a prospective study. Am J Psychiatry.1981;138:629–35. [PubMed]
7. White AJ, Barraclough B. Benefits and problems of routine laboratory investigations in adult psychiatric admissions. Br J Psychiatry. 1989;155:65–72. [PubMed]
8. Koran LM, Sox HC, Jr, Marton KI, et al. Medical Evaluation of psychiatric patients: Results in a state mental health system. Arch Gen Psychiatry. 1989;46:733–40.[PubMed]
9. Ferguson B, Dudleston K. Detection of physical disorder in newly admitted psychiatric patients. Acta Psychiatr Scand. 1986;74:485–9. [PubMed]
10. Olshaker JS, Browne B, Jerrard DA, et al. Medical clearance and screening of psychiatric patients in the emergency department. Acad Emerg Med. 1997;4:124–8.[PubMed]
11. Dolan JG, Mushlin AI. Routine laboratory testing for medical disorders in psychiatric inpatients. Arch Intern Med. 1985;145:2085–8. [PubMed]
12. Lukens TW, Wolf SJ, Edlow JA, et al. Clinical policy: critical issues in the diagnosis and management of the adult psychiatric patient in the emergency department. Ann Emerg Med. 2006;47:79–99. [PubMed]
13. Perrone J, De Roos F, Jayaraman S, et al. Drug screening versus history in detection of substance use in ED psychiatric patients. Am J Emerg Med. 2001;19:49–51. [PubMed]
14. Schiller MJ, Shumway M, Batki SL. Utility of routine drug screening in a psychiatric emergency setting. Psychiatr Serv. 2000;51:474–8. [PubMed]
15. Eisen JS, Sivilotti MLA, Boyd KU, et al. Screening urine for drugs of abuse in the emergency department: do tests results affect physicians’ patient care decisions. Can J Emerg Med. 2004;6:104–11.
16. Korn CS, Currier GW, Henderson SO. “Medical clearance” of psychiatric patients without medical complaints in the emergency department. J Emerg Med. 2000;18:173–6. [PubMed]
17. Henneman PL, Mendoza R, Lewis RJ. Prospective evaluation of emergency department medical clearance. Ann Emerg Med. 1994;24:672–7. [PubMed]